Part 1 of 2
The process of billing and coding may at first seem daunting. But by doing a little research you’ll find these tasks to be easier than you thought. In part one of this series, we’ll take a look at electronic medical record systems. Next month’s part two will cover proper coding.
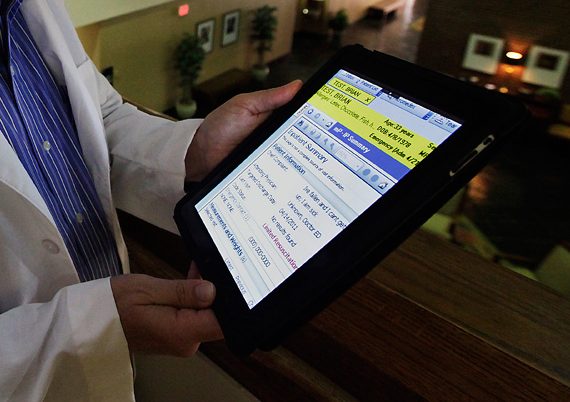
Dermatology training programs and practices are increasingly utilizing electronic medical record systems (EMRs) to document patient encounters, interface with other providers, and bill insurance companies. Outpatient EMRs are designed to be used by one specialty or formulated to be used across multiple different specialties, depending on the practice setting.
The use of SOAP (Subjective, Objective, Assessment, Plan) note templates, smart phrases. And point-and-click documentation can make for efficient documentation and help manage the information required for meaningful use. Additionally, many EMRs have the ability to automatically generate a level of service code based on the provided SOAP note documentation.
The efficiencies afforded by using EMRs must be weighed against the potential for misuse. While inpatient documentation often uses the “copy forward” button in daily progress notes, outpatient providers can use the “copy forward” feature to include past complicated medical histories in current SOAP notes, accompanied by an interval history. When using “copy forward” features, providers need to pay extra attention to the final generated document. To look for inaccuracies as too casual use may increase errors in documentation.
Another potential pitfall of EMRs is the notion of “over documentation.”
Templated notes, which automatically include multiple reviews of systems, family, past medical, and social histories, or extensive physical exam documentation, may support a higher level of service despite a provider billing for a lower level of service. This discrepancy in documentation and billing can be resolved by the provider removing templated elements of the history. And review of systems they did not specifically address during that visit. EMRs that automatically calculate level of service should always be reviewed by the billing provider prior to submitting a claim to insurance companies. EMRs may generate evaluation and management billing codes, but may not generate procedure CPT codes or apply appropriate modifiers. Providers should remember they are ultimately responsible for the billing codes submitted to insurance companies.
Many electronic record systems can facilitate communication, with use of templated consultation letters to communicate findings with referring providers. And patient portals where patients have the ability to submit prescription requests, communicate with providers via email. And view laboratory results.
Another benefit of EMRs lies in their ability to help providers transition to ICD-10 diagnosis codes. Many systems have easy search functions or the ability to carry forward diagnosis codes from prior visits. Which can cut down on time spent looking for unfamiliar codes.
These are just a few of the benefits and potential pitfalls of using electronic medical record systems. Dermatologists should take the time to compare different EMR systems and spend time learning all the features and functions of their chosen EMR to take full advantage of its efficiencies.