Part 1 in a 2 part series
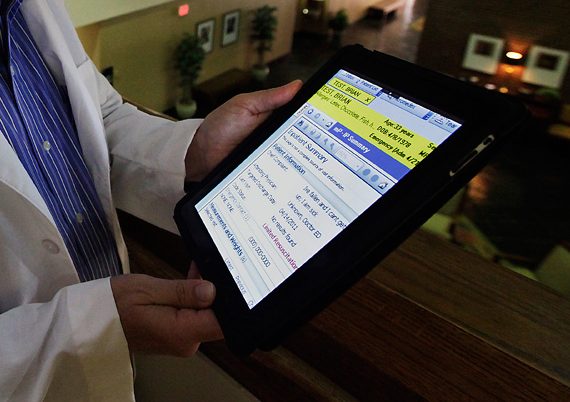
One of the most important decisions in any practice is the choice of using an Electronic Medical Record (EMR). Implementing an EMR from the outset is imperative and will enable you to conserve precious office space. This should also be a natural transition from a training/hospital environment for most MDs, as you will have all of your lab results and patient information in one place.
Do not be swayed by a single impressive presentation at a meeting; dedicate significant time and research into the right fit for your practice dynamics. Try multiple EMRs and call or visit with people who have experience with those systems. More useful information or reviews may come from listserves or specialty societies.
If you accept Medicare or Medicaid in your practice, make sure the EMR system you are considering meets all government reporting requirements, which will prevent payment penalties and ensure you qualify for incentive payments. These requirements currently include electronic prescribing, meaningful use, and quality reporting, but they are constantly evolving. For example, diagnosis coding shifted dramatically when ICD-10 was implemented in October 2015. Include written confirmation in any contract that the EMR will be updated and kept in compliance as requirements change. I made the error of starting with a cheaper EMR; I learned after two years that it did not meet new reporting requirements despite assurances from the vendor at the time of my purchase. For an entire year, my reimbursement for all Medicare patients was penalized. It was time-consuming and expensive to replace this system.
In next month’s Part 2 of this article, I will discuss the importance of finding an EMR that will adapt to changing workflows, as well as the pros and cons of using a cloud-based server versus housing a server in your office.