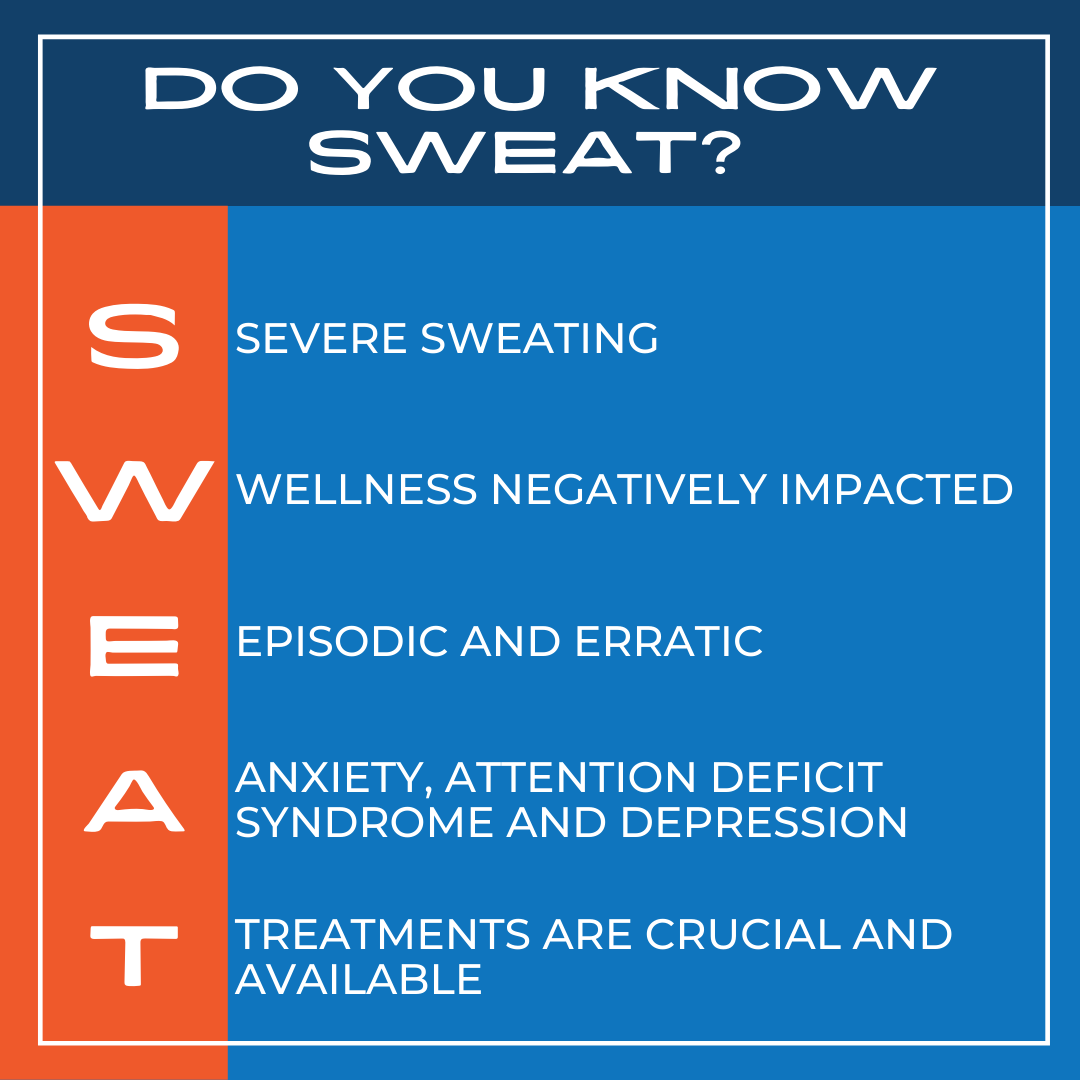
Improve Your Understanding of the Seriousness & Care of Hyperhidrosis with this SWEAT Mnemonic
Severe Sweating – Patients with excessive sweating or hyperhidrosis (Hh) experience severe sweating that is often four or five times more than what’s “normal,” or needed, to regulate body temperature or as a reaction to stress.1 This amount of sweat can be debilitating both physically and emotionally. Patients describe their Hh sweating as dripping, slipping, soaking, chilling, embarrassing, controlling, and damaging.
Wellness Negatively Impacted – Frequently, the impacts of excessive sweating are linked to emotional distress. In research presented at the American Academy of Dermatology Meeting in 2019, the International Hyperhidrosis Society shared sufferer testimonials with common themes of hyperhidrosis (Hh) contributing to feelings of self-harm, anxiety, isolation, and depression.2 The physical ramifications of Hh include a 300% greater risk of skin infections3and 60% of sufferers reporting negative impacts on general health.4
Episodic and Erratic – Hyperhidrosis (Hh) symptoms often manifest in episodes that can be unexpected and without explanation and with varying length/degree. The extreme, uncontrollable sweating will likely not be constant, and the episodes are not necessarily related to hot conditions, exercise, or stressful conditions. In fact, 65% of Hh sufferers say Hh is an issue no matter the season or weather.5
Anxiety, Attention Deficit Syndrome and Depression – In a study presented at the American Academy of Dermatology, results showed that among 500 hyperhidrosis (Hh) sufferers, 13.8% had anxiety, 12.4% had depression and 6.4% had attention deficit disorder — all of these are rates significantly higher than those reported in the general population.6 In other research, 5% of Hh sufferers say they take antidepressants or anti-anxiety medications due to their sweating.7With Hh getting in the way of socializing, relationships, and inclusion,4,8 helping patients find effective management techniques can be life-changing.
Treatments are crucial and available – With effective care, hyperhidrosis (Hh) sufferers experience significant improvements in well-being.9 Approximately 4.8% of the population4 suffer from excessive sweating but new research, greater understanding, and improved treatments are empowering people to take control and feel better. Antiperspirants of varying strengths and for different areas of the body are available. Iontophoresis, botulinum toxin injections, microwave thermolysis of the sweat glands and other localized underarm procedures, topical anticholinergics, oral anticholinergics, and, especially, combinations can be very effective and best practice information is accessible and free through the International Hyperhidrosis Society’s website at SweatHelp.org
 November is Hyperhidrosis Awareness Month. Learn more at SweatHelp.org and get involved on: Facebook @SweatingStopsHere, Twitter @WeKnowSweat, and Instagram @WeKnowSweat.
November is Hyperhidrosis Awareness Month. Learn more at SweatHelp.org and get involved on: Facebook @SweatingStopsHere, Twitter @WeKnowSweat, and Instagram @WeKnowSweat.
References:
-
- Hund M, Kinkelin I, Naumann M, Hamm H. Definition of axillary hyperhidrosis by gravimetric assessment. Arch Dermatol. 2002 Apr;138(4):539-41. doi: 10.1001/archderm.138.4.539. PMID: 11939828.
- Hebert AA, Glaser DA, Ballard AM, Pieretti LJ, Pariser DM. Voice of the hyperhidrosis patient: symptoms, impacts and treatments. Insights from a large, open, FDA-attended meeting. Poster presented at the 77th Annual Meeting of the American Academy of Dermatology, March 1-5, 2019, Washington, DC.
- Walling HW. Primary hyperhidrosis increases the risk of cutaneous infection: a case-control study of 387 patients. J Am Acad Dermatol. 2009 Aug;61(2):242-6. doi: 10.1016/j.jaad.2009.02.038. Epub 2009 Apr 23. PMID: 19395123.
- Doolittle J, Walker P, Mills T, Thurston J. Hyperhidrosis: an update on prevalence and severity in the United States. Arch Dermatol Res. 2016 Dec;308(10):743-749. doi: 10.1007/s00403-016-1697-9. Epub 2016 Oct 15. PMID: 27744497; PMCID: PMC5099353.
- Glaser DA, Ballard AM, Hunt NL, Pieretti LJ, Pariser DM. Prevalence of Multifocal Primary Hyperhidrosis and Symptom Severity Over Time: Results of a Targeted Survey. Dermatol Surg. 2016 Dec;42(12):1347-1353. doi: 10.1097/DSS.0000000000000949. PMID: 27879523.
- American Academy of Dermatology, 2019 Annual Meeting, Prevalence of Anxiety, Depression and Attention Deficit Disorder (ADD) in Patients with Primary Hyperhidrosis, https://server.aad.org/eposters/view/Abstract.aspx?id=8424
- Ruchinskas RA, Narayan RK, Meagher RJ, Furukawa S. The relationship of psychopathology and hyperhidrosis. Br J Dermatol. 2002 Oct;147(4):733-5. doi: 10.1046/j.1365-2133.2002.04857.x. PMID: 12366420.
- Kamudoni, P., Mueller, B., Halford, J. et al. The impact of hyperhidrosis on patients’ daily life and quality of life: a qualitative investigation. Health Qual Life Outcomes 15, 121 (2017). https://doi.org/10.1186/s12955-017-0693-x
- Glaser DA et al. Functional and dermatology-specific quality of life benefits with repeated botulinum toxin type A treatment of primary axillary hyperhidrosis over 4 years, presented at the 65th Annual Meeting of the American Academy of Dermatology, February 2-6, 2007, Washington, DC.
Content published with permission from the International Hyperhidrosis Society.
Did you enjoy this article? Find more on Hyperhidrosis here.