Dr. Jacqueline Watchmaker, a fellowship-trained cosmetic dermatologist at Southwest Skin Specialists in Scottsdale, Arizona, shared practical, evidence-informed guidance on assessing and managing complications from hyaluronic acid and other injectable fillers. She emphasized that, although complications can occur with frequent injections, an injector’s skill in prevention, early recognition, and appropriate management is what separates experts and safeguards patients. Her talk outlined strategies for differentiating early versus delayed-onset nodules and stepwise approaches to treatment, including hyaluronidase use and infection workup.
Filler Nodules: Early vs. Late Onset
Dr. Watchmaker referenced the Jones et al.’s article, “Preventing and Treating Adverse Events of Injectable Fillers: Evidence-Based Recommendations from the American Society for Dermatologic Surgery Multidisciplinary Task Force,” which differentiates filler nodules based on onset:
-
- Early onset (<4 weeks): Likely due to injection technique (i.e. superficial injections and excessive amount injected)
- Late onset (>4 weeks): Potentially caused by host sensitivity, poor aseptic technique, immune up-regulation (i.e. history of autoimmune disease), infection, or biofilm
For early onset nodules, hyaluronidase injections can be used to dissolve the nodules. Delayed onset nodules can be categorized as either non-inflammatory or inflammatory (i.e., erythematous, edematous, and tender). To address these complications, Dr. Watchmaker created a comprehensive chart detailing the treatment approach for each type of delayed onset nodule, providing clinicians with a clear guide for managing these more complex cases:
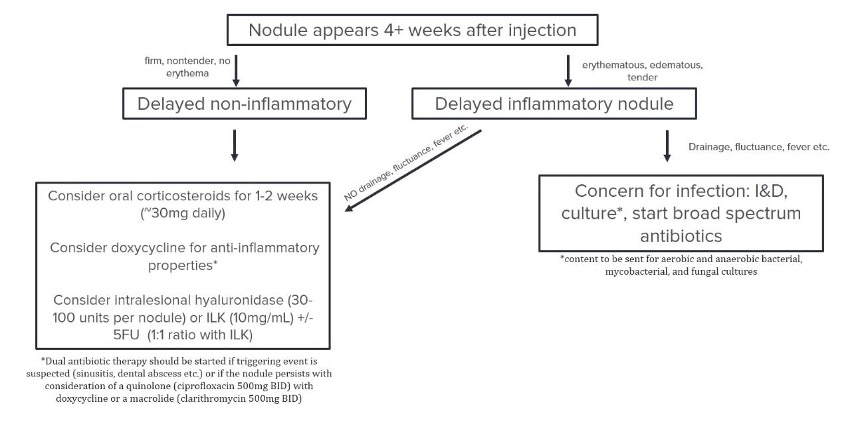
Treatment approach for delayed onset nodules. Photograph was provided courtesy of Dr. Jacqueline Watchmaker
Key points on hyaluronidase
Hyaluronidase is an off-label enzyme used to dissolve filler. There are two main brands in the US: Hylenex (human recombinant) and Vitrase (ovine). Prior to injecting, it is advisable to screen patients for bee/wasp sting allergy due to the risk of cross-reactivity.
Considerations for use:
-
- Can be reconstituted with bacteriostatic saline
- Lidocaine may affect enzymatic action
- Amount needed can vary with the product being dissolved (e.g., Vycross may require more)
Pro tip: For “puffy” or “overfilled” patients, Dr. Watchmaker recommends diluting hyaluronidase 1:1 with bacteriostatic saline and making multiple small injections in the area being treated.
Preventing Filler Complications
To reduce the overall incidence of inflammatory and non-inflammatory early and late nodules, Dr. Watchmaker summarized the findings of the ASDS task force recommendations, which included:
-
- Obtaining a thorough patient history
- Avoiding injection into areas with active inflammation
- Adopting aseptic technique
- Using small boluses (0.1 to 0.2 mL)
- Providing post-treatment patient education
- Avoiding dental or invasive procedures for >2 weeks before/after filler procedures
Managing Unhappy Patients: The B.L.A.S.T Technique
Dr. Watchmaker shared the B.L.A.S.T technique for managing displeased patients:
-
- Believe what they’re seeing and saying
- Listen and let them talk
- Apologize for any inconvenience
- Satisfy them by being available and offering solutions
- Thank them for coming to you with the complication
“Caviar” Complication
Dr. Watchmaker discussed the “caviar” complication – multiple superficial hyaluronic acid filler collections causing bluish-grey discoloration, often seen in the lateral oral commissure. She theorized that these small nodules occur secondary to one of three factors: (1) Filler placed too superficially, (2) filler with a high G’ placed in a highly mobile area, and (3) old filler migrating towards the surface. Her treatment approach included:
-
- Use a needle to puncture the skin
- Use a comedone extractor to expel the hyaluronic acid
Tips for Bruising
Prevention: Providers can change needles frequently, use cannulas, back-fill into small syringes (i.e., TB syringes), use vein finders (particularly around the eyes), and minimize fish oil and aspirin/ibuprofen intake.
Minimize bruising: Dr. Watchmaker recommends using a pulsed dye laser 1-2 days after treatment at the following setting: 10mm, 7.75J, 6ms. Other options include gentle massage and arnica creams.
Vascular occlusions
Dr. Watchmaker emphasized the importance of recognizing signs of vascular occlusion, which can include pallor, reticular erythema, and pain. However, she noted that some other crucial indicators that some may overlook, such as:
-
- Whiteness or unusual rash
- Bruising outside the injected area
- Acneiform pustular rash
It’s important to note that the end stage of a vascular occlusion can present as a pustular rash, which may be mistaken for herpes zoster. To address these vascular occlusions, Dr. Watchmaker created a comprehensive chart detailing the treatment approach:
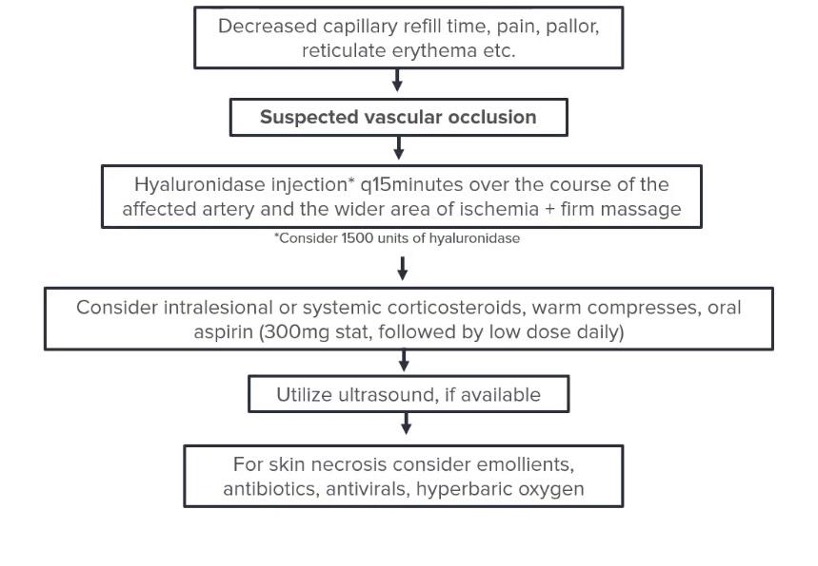 Treatment approach for vascular occlusions. Photograph was provided courtesy of Dr. Jacqueline Watchmaker
Treatment approach for vascular occlusions. Photograph was provided courtesy of Dr. Jacqueline Watchmaker
Additional tips:
-
- Check capillary refill time post-injection in high-risk areas
- Use a hemostat or paperclip to assess delayed capillary refill
- Remember that compression from high volumes of filler can cause occlusion without direct arterial injection
In summary, Dr. Watchmaker’s presentation provided comprehensive guidance on managing filler complications, emphasizing the importance of prevention, early recognition, and appropriate treatment strategies. Her insights offer valuable tools for dermatologists and aesthetic practitioners to enhance patient safety and satisfaction in their practices.
This information was presented by Dr. Jacqueline Watchmaker during the 2025 ODAC Dermatology Conference. The above session highlights were written and compiled by Dr. Vixey Silva.
Cover image: patient image used with permission from the Journal of Drugs in Dermatology | Nanda, Rahul, Jason Covone, and Joel L. Cohen. “Delayed Inflammatory Reactions to Hyaluronic Acid Fillers: A Case Series of Novel Associations.” Journal of drugs in dermatology: JDD 24.1 (2025): 101-103.
Did you enjoy this article? You can find more on Aesthetic Dermatology here.

