It’s time for a review of Dr. Adam Friedman’s presentation, “Complexities of Managing Inflammatory Diseases,” which was another one of the popular lectures from ODAC 2018. This lecture was case-based and full of helpful pearls. So let’s get to it!
CASE #1: 70-year-old female with red, pruritic “rash” involving her face, trunk, and extremities for several months. The rest of her history was non-contributory. See photo below…
What is your diagnosis?
- Granuloma annulare
- Sarcoidosis
- Necrobiosis lipoidica
- Leprosy
- Lupus
- Gyrate erythema
ANSWER: Granuloma Annulare (GA)
Quick Review
There are several variants of GA, including localized, generalized, perforating, subcutaneous/deep dermal, micropapular, patch, and nodular. Over the years, there have been many studies showing the association of diabetes (type 1 and 2). Also, a 2012 retrospective study revealed that GA patients are four times more likely to have dyslipidemia, which increases with the severity of GA.1 Generalized GA was shown to have the highest association with dyslipidemia.1
What are the current treatment options? Some patients were treated successfully with combination therapy of rifampin, ofloxacin, and minocycline for 3 months.2 Infliximab has also been reported to induce remission, while etanercept has had mixed results. Importantly, 50-75% of patients have spontaneous resolution, so no treatment may be the best treatment.
Case #2: 15 year old male with a history of an asymptomatic recurrent rash initially on the face but reoccurrence involving the face, ears, trunk and upper extremities. He had been treated with topical antibiotics and topical steroids.
What is your diagnosis?
- Cutaneous lupus
- Erythema multiforme
- Pemphigus vulgaris
- Linear IgA bullous dermatosis
- Paraneoplastic pemphigus
Answer: Erythema Multiforme (EM)
Quick Review
EM is typically triggered by infection, commonly HSV1, especially in recurrent cases. Mycoplasma pneumonia is the second major cause of EM, possibly the major cause in pediatric cases. Group A Streptococcus, Orf, VZV, Parvovirus, hepatitis B and C, as well as EBV have also been identified in case reports. Additional triggers also include various drugs. A significant portion of cases are idiopathic. Recurrent EM is common and may characterize the majority of cases, with the mean number of recurrences being greater than 6 attacks per year. The mean total duration of disease has been reported to be 9.5 years. 3
As mentioned earlier, HSV is the most common etiology associated with recurrent EM. Recurrences in the same patient can produce the classic targetoid lesions initially, while later producing plaques. At times, mucous membranes are severely involved.
How can we treat these patients? EM is typically self-limited; however, the use of anti-HSV drugs have demonstrated some utility. The use of systemic corticosteroids is controversial, given possible resulting complications. Treatment is typically aimed at symptomatic relief.
Case #3: 45 year old female with complaints of a pruritic, violaceous rash on the trunk and extremities, along with oral erosions for 5 years. She also reported hair loss on the scalp, axillae and groin. Treatment with high potency topical, intralesional, and oral steroids, topical retinoids, and antifungals.
What’s your diagnosis?
- Lichen planus
- DLE
- Lichen planopilaris
- Lichen simplex chronicus
- Psoriasis
- Secondary syphilis
Answer: Graham-Little-Piccardi-Lassueur Syndrome (LP+LPP+ alopecia of axillae/groin)
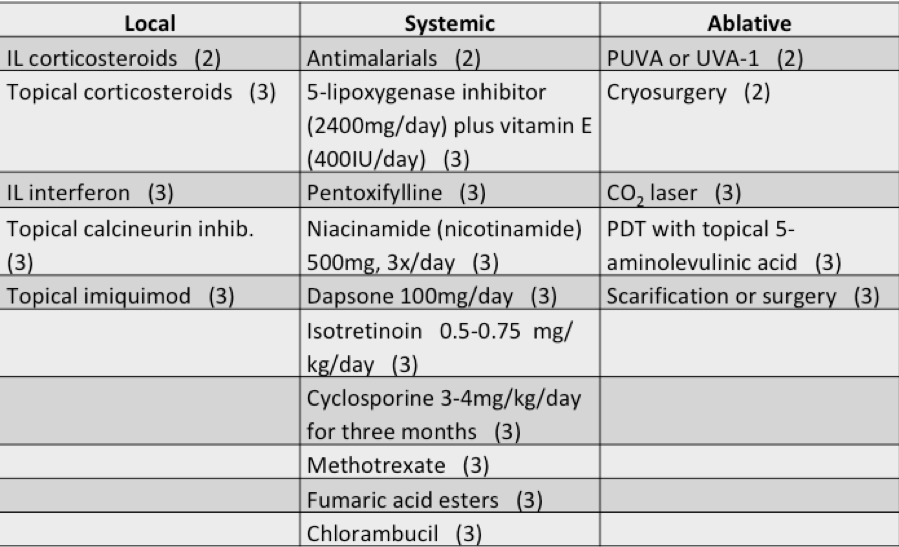
This patient has refractory cutaneous lichen planus, so let’s discuss potential treatment options for this group of patients. It is difficult to evaluate therapeutic options as most evidence consists of small case series or anecdotes. Spontaneous remissions of cutaneous LP has been observed in up to 2/3 of patients after just one year. Systemic treatments are usually reserved for recalcitrant skin disease.
PEARL ALERT!!! Treatment options for disseminated, recalcitrant skin disease include:
Retinoids: Acitretin 0.5-0.7 mg/kg until remission, then 0.3-0.5 mg/kg thereafter; Isotretinoin 3-5 mg/kg
Methotrexate: 15-20mg once weekly x 10 weeks
Antimalarials: Hydroxychloroquine 200mg BID (max 6.5 mg/kg ideal);
Dapsone
PEARL ALERT!!!! Treatment options for mucosal LP include:
1st line: Doxycycline 100mg BID x 6mos OR Prednisolone 0.3-0.5mg/kg
2nd line: Methotrexate 7.5-20mg once weekly OR Hydroxychloroquine 200-400mg daily x 6 mos OR Retinoids (better for cutaneous disease)
3rd line: Cyclosporine 1-2.5 mg/kg
Some relatively safe alternatives for children: griseofulvin, itraconazole, or metronidazole.
Lichen planopilaris (aka follicular LP or LP acuminatus) is characterized by multiple, keratotic plugs surrounded by a narrow violaceous rim primarily located on scalp. Cutaneous LP lesions may or may not be present. It is more commonly seen in females during the 5th and 6th decades of life. Alopecia may progress to scarring alopecia, often becoming indistinguishable from other cicatricial alopecias. Frontal fibrosing alopecia, lichen planus follicularis tumidus, popular eruption of the face, and Graham-Little-Piccardi-Lassueur Syndrome (GLPLS) are variants of LPP.
GLPLS is a rare variant of LPP often affecting postmenopausal women. The classic triad is (1) LPP on scalp, (2) non-cicatricial loss of pubic and axillary hairs, and (3) lichenoid spinous follicular papules. LPP is usually the initial presentation. Unfortunately, the etiology is still unknown and there are many hypotheses, such as HLA-DR antigens enhancing a T-cell mediated immune response.
Treatment is often unsuccessful, but options include: cyclosporine A, antimalarials, thalidomide, corticosteroids, retinoids, topical tacrolimus, and PUVA.
Case #4: 80-year-old male with 6-week history of a progressively enlarging rash of the left eye and mid-chest that is mildly painful.
What’s your diagnosis?
- PMLE
- Jessner’s
- Pseudolymphoma
- Tumid lupus
- Lues
- Deep gyrate erythema
Answer: Tumid lupus
Clinically, patients present with “succulent” erythematous, nonscarring plaques in photodistributed areas. Biopsy is truly what will help you to distinguish it from your differential diagnoses, because they can all present in a similar fashion. Antimalarials are very effective treatment options, but topical or intralesional steroids with sun protection is helpful as well. In an open-label, prospective study of 10 patients with histologically confirmed tumid lupus, PDL-treated areas maintained clinical response for a minimum of 6 months post-therapy.4
Case #5: 35-year-old male with generalized rash for several months, previously treated with oral steroids with no improvement. He denies fever, chills, joint pain, cough, weight loss or night sweats. No new medications.
What’s the diagnosis?
- Pityriasis rubra pilaris
- Psoriasis
- CTCL
- Atypical pityriasis rosea
- Eczematous drug eruption
Pityriasis rubra pilaris (PRP) has an onset most commonly occurring in the first 5 years of life and the mid-50s. Patients present with salmon-colored folliculocentric scaly papules coalescing into plaques with islands of sparing starting on the scalp before generalizing. Confluent palmoplantar keratoderma is also present. The etiology is unknown. There are several types of PRP with variable clinical courses. Classic type I and III usually resolve in 3 years.
Treatment options include: systemic retinoids, methotrexate, TNF-alpha inhibitors, PUVA/NB-UVB, cyclosporine, and azathioprine. Apremilast has been indicated as a possible therapy for refractory PRP.
Case 6a: 50 year old female with recurrent tender “bumps” on bilateral lower legs for 1 year, previous one on arm. Lesions resolve after a few weeks. Treatment with clindamycin gel.
Case 6b: 30-year-old female with large, tender erythematous plaques on lower legs for 3 weeks with fever and leukocytosis. Previously had Strep throat treated with amoxicillin and developed red nodules on shins one week later.
What’s your diagnosis?
- Rheumatoid nodules
- Polyarteritis nodosa
- Darier Rousey Sarcoid
- Erythema nodosum
- Erythema induratum
Answer: Septal Panniculitis c/w Erythema Nodosum (EN)
EN is an acute painful panniculitis usually occurring on lower extremities. Lesions resolve over 1-2 weeks and heal without scarring. Fever and malaise often precedes the EN lesions. Females are more commonly affected with peak ages of 18-34 years.
PEARL ALERT!!! The most common cause of EN in both children and adults is… streptococcal infection. Other common causes of EN include: idiopathic, infectious (Yersinia, Salmonella, viral URI, etc), sarcoidosis, IBD (Crohn’s > Ulcerative colitis), and medications (OCPs, penicillin, sulfonamides, etc.).
Erythema nodosum migrans (aka subacute nodular migratory panniculitis) presents as nodules on the lower legs that migrate or undergo centrifugal spread with central clearing. Acute EN can be treated with NSAIDS (Indomethacin 100-150mg/d, Naproxen 250mg BID). Chronic EN is treated with Dapsone 100mg daily or Hydroxychloroquine 200mg BID. Corticosteroids are reserved for severe disease.
Well that does it for this EXHILARATING review of several popular lectures from ODAC 2018. I hope you all enjoyed the reviews and have been able to take away some helpful tips from each of the lectures. If you are able to attend ODAC 2019, I highly encourage you to do so. It is packed with tons and tons of Medical & Cosmetic Dermatology Pearls and includes many opportunities for hands-on learning. For the residents out there, the Board Review is highly attended and full of high yield information. And don’t forget about the networking and opportunities to meet fellow residents from other programs in the country. I hope to see you there!
References
- Wu W, Robinson-Bostom L, Kokkotou E, et al. Dyslipidemia in granuloma annulare: a case-control study. Arch Dermatol. 2012;148(10):1131-1136.
- Marcus DV, Mahmoud BH, and Hamzavi IH. Granuloma annulare treated with rifampin, ofloxacin, and minocycline combination therapy. Arch Dermatol. 2009 Jul;145(7):787-9.
- Schofield JK, Tatnall FM, and Leigh IM. Recurrent EM. Clinical features and treatment in a large series of patients. Br J Dermatol. 1993 May;128(5):542-5.
- Truchuelo MT et al. Pulsed dye laser as an excellent choice of treatment for lupus tumidus: a prospective study. J Eur Acad Dermatol Venereol 2012 Oct;26(10):1272-9.