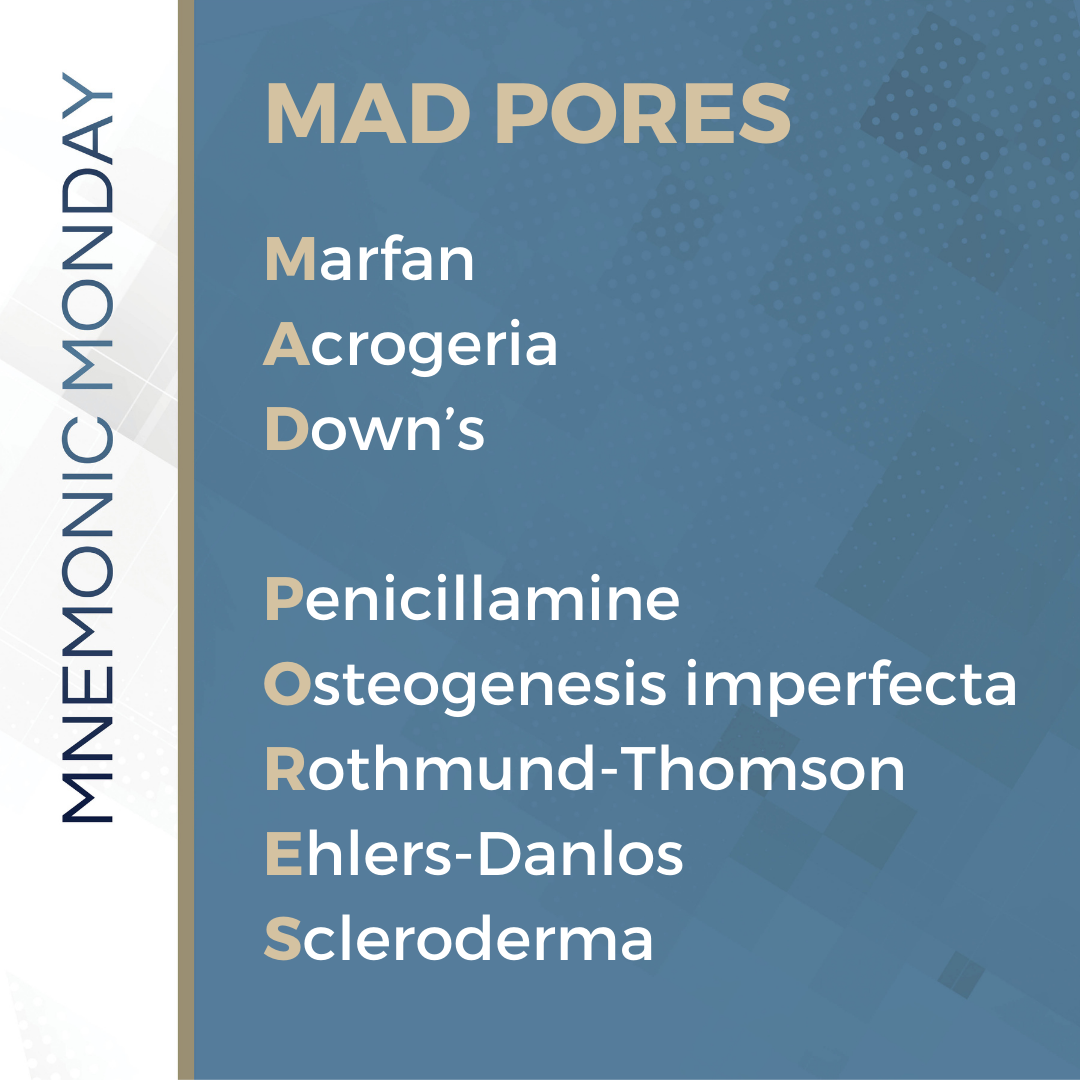
On this Mnemonic Monday, we challenge you to remember diseases or medication exposures associated with Elastosis Perforans Serpiginosa (EPS) with the following mnemonic:
MAD PORES
Marfan
Acrogeria
Down’s
Penicillamine
Osteogenesis imperfecta
Rothmund-Thomson
Ehlers-Danlos
Scleroderma
Click HERE to print your mnemonic card.
Study More!
Need a refresher on Perforating Disorders and
Elastosis Perforans Serpiginosa (EPS)? Check out the following pages of your 2019 Derm In-Review Study Guide:
Perforating disorders/Elastosis perforans serpiginosa: 89
Don’t have a copy? Sign up for Derm In-Review and download the digital version here.
Further Reading
Check out the following case report published in the Journal of Drugs in Dermatology (JDD):
A Case of Perforating Dermatosis in a Patient With Primary Sclerosing Cholangitis
Introduction
An African-American female, aged 27 years, presented to the dermatology clinic for a follow-up evaluation of multiple pruritic, darkly pigmented papules on the face, ears, chest, abdomen, back, upper extremities, and lower extremities. She was referred from the gastroenterology clinic where she was receiving treatment for primary sclerosing cholangitis (PSC).
The patient had been seen approximately eight months previously by dermatology as an in-patient consult for this same complaint. At that time, the patient was admitted to the hospital for acute pancreatitis, cholecystitis, and eosinophilia due to underlying PSC. A shave biopsy of one of the characteristic skin lesions was read as lichen spinulosis. Phyrynoderma was also entertained due to a low serum level of vitamin A (15 μg per dL). After a cholecystectomy, the patient was discharged from the hospital on a treatment regimen of ursodiol, lansoprazole, vitamin A supplementation, topical keratolytics, and oral antihistamines.
When the patient was seen several months later, her physical exam revealed over 100, 1 mm to 8mm hyperpigmented, round, perifollicular, and parafollicular papules with some coalescence into plaques. Many papules contained a central keratotic plug. The lesions were most prominent on the extensor surfaces of the legs, but also on the arms, chest, back, abdomen, and a few lesions on the face and ears (Figures 1 and 2). There was no involvement of the palms, soles, or mucous membranes. Icterus of the sclera and of the oral mucosa, especially the sublingual mucosa, was noted. Besides a personal history of PSC, past medical history and family history were non-contributory.


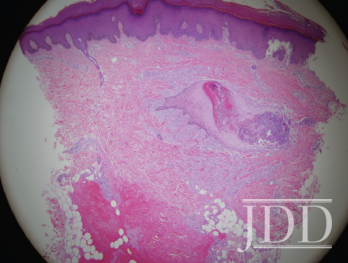
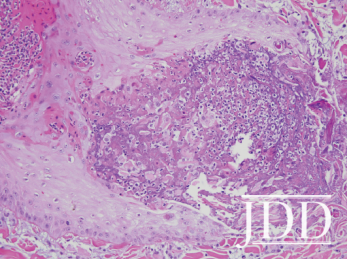
Punch biopsies were taken from two separate lesions on her bilateral lower extremities. The histology of a papule on the right thigh showed a dilated follicular infundibulum with a central keratotic plug. The papule on the left thigh revealed a transepithelial channel lined by an acanthotic and hyperkeratotic epidermis with degenerated follicular contents, elastin, collagen and a granulomatous reaction at the base (Figures 3 and 4). Her clinical lesion distribution, known medical history of PSC, lack of improvement with vitamin A supplementation, and histological analysis favored the diagnosis of a perforating dermatosis.
Discussion
The disorders of perforation are unique as they represent examples of transepithelial elimination in which altered dermal substances are extruded through epidermal channels. The 4 classically described perforating disorders include elastosis perforans serpiginosa (EPS), reactive perforating collagenosis (RPC), perforating folliculitis (PF), and Kyrle’s disease (KD). In EPS, the extruded substance is elastin. In RPC, the substance is collagen. In PF, it is degenerated follicular contents, which may contain elastic fibers or collagen. Lastly, in KD, the substance is basophilic debris, which is generally negative for elastic stains.¹
Since 1916, when Kyrle first described the disorder that now bears his name, physician awareness of these entities has increased. More and more cases have been reported and an apparent trend in the secondary development of these lesions has been documented in patients with renal disease and diabetes mellitus.
Clinically, the lesions of “acquired perforating dermatosis” have been described as hyperkeratotic papules, often with a hyperkeratotic plug occurring mainly on the lower extremities but also on the trunk and face. Koebner’s phenomenon may occur and severe pruritus and rubbing may lead to a coalescence of the papules into plaques.² The clinical differential diagnosis for these patients would also include lichen spinulosis, phyrynoderma, keratosis pilaris, hypertrophic lichen planus, prurigo nodularis, eruptive keratoacanthomas, and Darier’s disease.1,2 The distinguishing features of the major perforating diseases are listed in Table 1.³ It is interesting to note that PF may sometimes be found in lesions of lichen spinulosus.4
Conclusion
The pathogenesis of acquired perforating disorders in association with liver disease is unclear at this time. However, some feel cholestatic induced pruritus may be a contributing and perpetuating factor and that the course of skin findings may parallel the course of liver disease.5 Patients often seek treatment of acquired perforating diseases due to extreme pruritus and cosmetic concerns. However, treating these patients is frustrating, as current medical therapies have not proven to be very effective. A list of treatments that have been used include antihistamines, hydroxyzine, local and systemic antibiotics, oral vitamin A, keratolytics, cryotherapy, and topical steroids.6 Additionally, one small study suggests that narrow-band UVB phototherapy may be helpful and alleviate symptoms of pruritus.³
The patient above was followed in Dermatology and successfully treated with phototherapy using narrow-band UVB for symptomatic relief of her pruritus while awaiting liver transplantation for treatment of her PSC.
References
-
- Patterson JW. The perforating disorders. J Am Acad Dermatol. 1984;10(4):561-581.
- Rapini RP, Herbert AA, Drucker CR. Acquired perforating dermatosis. Evidence for combined transepidermal elimination of both collagen and elastic fibers. Arch Dermatol. 1989;125(8):1074-1078.
- Bolognia J, Jorizzo J, Rapini R. Dermatology. 2nd ed. Ch 95;1461-1467. Mosby. 2008.
- Patterson JW, Eubanks SW, May DL. Lichen spinulosus with perforating folliculitis. J Assoc Mil Dermatol. 1983;9(22).
- Mahajan S, Koranne RV, Sardana K, Mendiratta V, Damani A. Perforating folliculitis with jaundice in an Indian male: a rare case with sclerosing cholangitis. Br J Dermatol. 2004;150(3):614-616.
- Ohe S, Danno K, Sasaki H, Isei T, Okamoto H, Horio T. Treatment of acquired perforating dermatosis with narrowband ultraviolet B. J Am Acad Dermatol. 2004;50(6):892-894.
Thomas Beachkofsky MD and W. Chad Cragun MD FAAD (2012). A Case of Perforating Dermatosis in a Patient With Primary Sclerosing Cholangitis
11(7).
https://jddonline.com/articles/dermatology/S1545961618P0582X
Content and images used with permission from the Journal of Drugs in Dermatology.
Test your knowledge!
A patient has multiple erythematous papules with central keratotic plug with many annular or serpiginous patterns on the neck. This condition is associated with all the following except for:
A. Marfan’s syndrome
B. Down’s syndrome
C. Osteogenesis imperfecta
D. Ehlers-Danlos syndrome
E. Buschke Ollendorf
To find out the correct answer and read the explanation, click here.
Did you enjoy this mnemonic? You can find more here.
Brought to you by our brand partner Derm In-Review. A product of SanovaWorks.