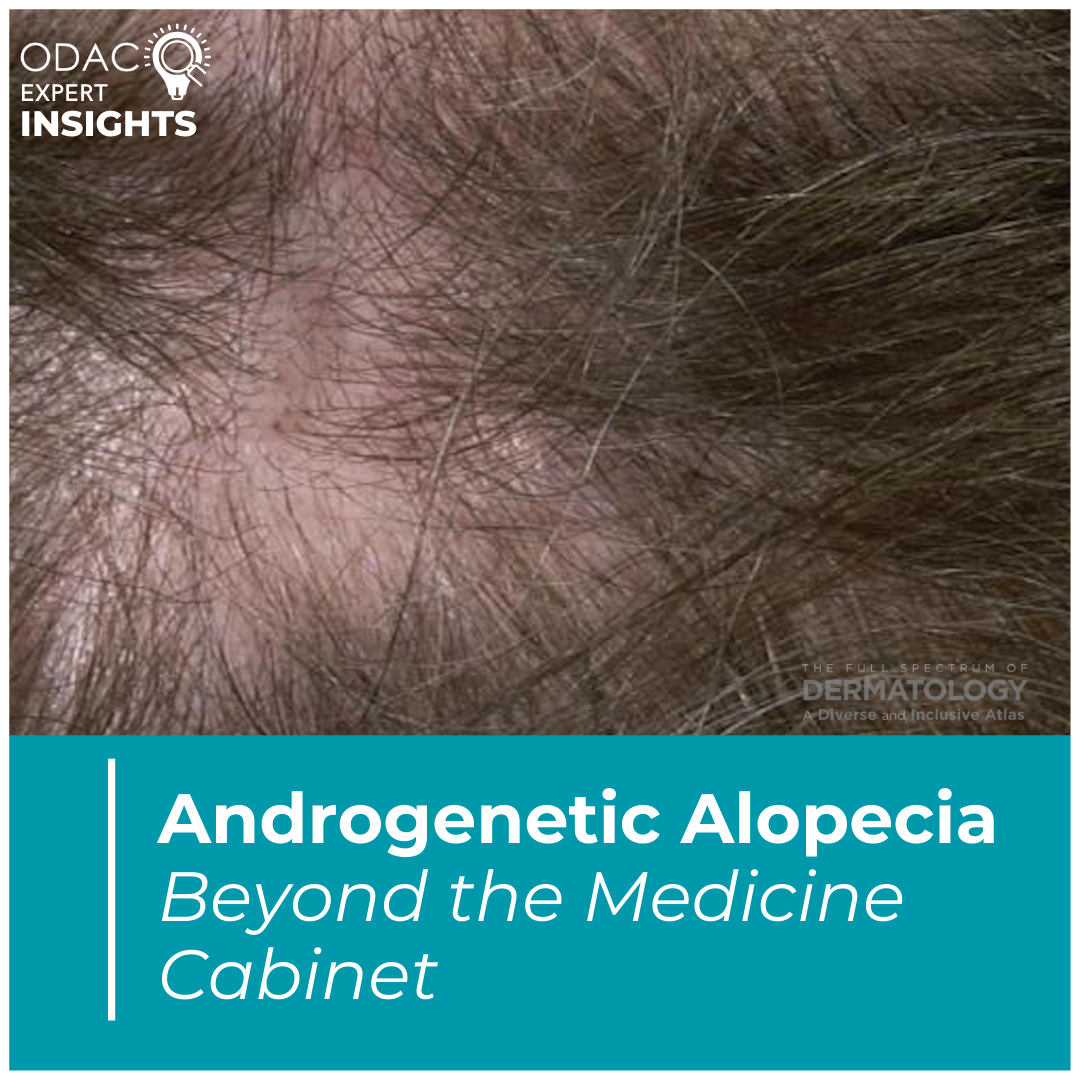
At the 2025 ODAC Dermatology Conference, we were delighted to learn about alternative treatments for androgenetic alopecia (AGA), presented by Dr. Terrence Keaney, Founder and Director of SkinDC and Clinical Associate Professor of Dermatology at The George Washington University School of Medicine and Health Sciences.
In recent times, there has been an exponential growth of interest from the patient perspective of potential treatments beyond medical management for AGA and an increase in curiosity regarding biomodulation and regenerative medicine. Dr. Keaney discussed several alternatives to first line therapies for the treatment of AGA, reviewing clinical trial data and real-world applications.
Platelet-Rich Plasma (PRP)
Dr. Keaney first discusses PRP, a treatment that he has employed in his practice for the past 8 years. Despite its longstanding presence, in a recent meta-analysis, only 10 clinical trials with quantifiable outcomes have been conducted to date, encompassing 555 treatment units in total. These studies have demonstrated increased hair density in patients with AGA with a stronger effect in male patients.1 He mentions that it is important to note that there are difficulties with standardization due to inherent variations in study design and PRP preparation systems.
Understanding PRP
Dr. Keaney goes on to further describe how PRP, as the name suggests, is characterized by obtaining a blood sample and concentrating platelets into a small amount of plasma, which appears deceivingly simple and uniform. These platelets contain alpha granules filled with growth factors, which are released upon activation. Additionally, PRP includes cell adhesion molecules, exosomes, cytokines, and other bioactive molecules, making it a complex and multifaceted treatment. Dr. Keaney likened PRP to a “growth factor cytokine cocktail,” emphasizing the lack of standardization in its preparation—akin to the difference between taste and preparation of cocktails at a college bar versus an upscale hotel.
With different PRP systems, there are variations in drawing of volume of blood, system, centrifugation, delivery volume, which is further explored in a systematic review looking at PRP protocol variations across studies. All studies differed in what system they used, length of centrifugation, quantity of blood volume obtained, quantity injected, making the comparison and standardization difficult given the number of variables.2
Optimizing PRP Treatment
While variations exist, Dr. Keaney focuses on simplifying key takeaways from research:
Frequency: Dr Keaney references a study that demonstrated monthly subdermal depot injections are better at increasing shaft thickness and hair density compared to quarterly.3 This supports the regimen of monthly loading doses for 3-4 months/injections Thereafter, he would recommend maintenance every 3-6 months depending on patient response.
Dosing: When considering dosing, we do not currently have in vivo studies, but a split scalp study of lower concentration of 5x versus higher concentration of 10x demonstrated improvement in hair growth on both sides, however, the higher concentration of 10x demonstrated greater effect on hair density, terminal hair density, and follicle diameter.4
Limitations: It is important to know that PRP is used off label for hair loss, and while there is a significant trend that PRP can help with AGA as well as a scientific rationale, clinical data remains limited and there are inconsistencies with study design. Dr. Keaney emphasizes the importance of discussing the risk benefit profile with the patient.
Determining Clinical Response
Regarding clinical response, Dr. Keaney stressed the importance of trichoscopy and photography in monitoring clinical response. There are systems that can obtain quantitative measures of hair counts and hair diameter. At his practice, this information is printed and given to patients. This allows for objective measurement and standardization, which may further help determine treatment adjustments if needed.
Platelet-Rich Fibrin (PRF)
PRF has also grown in popularity recently, as Dr. Keaney mentions. Unlike PRP, a blood specimen is drawn into a tube without anticoagulant and spun on a low centrifuge speed, leading to clot formation, increase in viscosity, and inclusion of leukocytes. Though PRF may have its advantages such as lower cost, this may not be a preferred option for follicular stimulation because of the surface area covered and desire for diffusion of growth factors. In addition, there is a paucity of data regarding the benefit of PRF for hair loss.
Exosomes
Exosomes are extracellular vesicles that contain protein, DNA, and RNA of their parent cells. They are taken up by distant cells, where they can affect cell function and behavior. He describes emerging lab evidence suggesting exosomes may augment the hair inductive capacity of the dermal papillae however he cautions their use as there is no FDA-approved exosome products and their clinical use remains experimental.5
Microneedling
Dr. Keaney highlights the potential utility of microneedling as a means of delivery of topical minoxidil/PRP as well as its potential to endogenously increase platelet degranulation when used in combination with PRP. Additionally, it could be used as a standalone therapy for AGA given release of growth factors and revascularize the skin.6
Photobiomodulation
Dr. Keaney briefly touches on photobiomodulation for AGA, which has also grown public interest as of recent. Patient adherence is a significant limitation. In the largest low level light therapy study to date, more than half of the study participants were excluded due to major protocol deviations and primarily, poor treatment compliance.7 This recommendation should be reserved for the highly motivated patient as a 3rd or 4th line therapy.
Surgical Hair Restoration
Dr. Keaney lastly discusses surgical hair restoration which is certainly something that we should consider if the patient is an appropriate candidate. Different techniques highlighted include the strip excision and follicular unit extraction. Recently, the follicular unit extraction technique seems to be in favor due to reduction in linear occipital scars, reduced technical support, and improved postoperative healing and pain.
References
-
- Li M, Qu K, Lei Q, Chen M, Bian D. Effectiveness of Platelet-Rich Plasma in the Treatment of Androgenic Alopecia: A Meta-Analysis. Aesthetic Plast Surg. 2024 Mar;48(5):977-984. doi: 10.1007/s00266-023-03603-9. Epub 2023 Aug 29. PMID: 37644190; PMCID: PMC10980625.
- Kramer ME, Keaney TC. Systematic review of platelet-rich plasma (PRP) preparation and composition for the treatment of androgenetic alopecia. J Cosmet Dermatol. 2018 Oct;17(5):666-671. doi: 10.1111/jocd.12679. Epub 2018 May 22. PMID: 29790267.
- Hausauer AK, Jones DH. Evaluating the Efficacy of Different Platelet-Rich Plasma Regimens for Management of Androgenetic Alopecia: A Single-Center, Blinded, Randomized Clinical Trial. Dermatol Surg. 2018 Sep;44(9):1191-1200. doi: 10.1097/DSS.0000000000001567. PMID: 30141776.
- Sasaki GH. The Effects of Lower vs Higher Cell Number of Platelet-Rich Plasma (PRP) on Hair Density and Diameter in Androgenetic Alopecia (AGA): A Randomized, Double-Blinded, Placebo, Parallel-Group Half-Scalp IRB-Approved Study. Aesthet Surg J. 2021 Oct 15;41(11):NP1659-NP1672. doi: 10.1093/asj/sjab236. Erratum in: Aesthet Surg J. 2022 Dec 14;42(12):NP811-NP812. doi: 10.1093/asj/sjac237. PMID: 34050738
- Yan H, Gao Y, Ding Q, Liu J, Li Y, Jin M, Xu H, Ma S, Wang X, Zeng W, Chen Y. Exosomal Micro RNAs Derived from Dermal Papilla Cells Mediate Hair Follicle Stem Cell Proliferation and Differentiation. Int J Biol Sci. 2019 May 20;15(7):1368-1382. doi: 10.7150/ijbs.33233. PMID: 31337968; PMCID: PMC6643152.
- Fertig RM, Gamret AC, Cervantes J, Tosti A. Microneedling for the treatment of hair loss? J Eur Acad Dermatol Venereol. 2018 Apr;32(4):564-569. doi: 10.1111/jdv.14722. Epub 2017 Dec 21. PMID: 29194786.
- Thomas M, Stockslager M, Oakley J, Womble TM, Sinclair R. Clinical Safety and Efficacy of Dual Wavelength Low-Level Light Therapy in Androgenetic Alopecia: A Double-Blind Randomized Controlled Study. Dermatol Surg. 2024 Dec 16. doi: 10.1097/DSS.0000000000004509. Epub ahead of print. PMID: 39679573.
This information was presented by Dr. Terrence Keaney at the 2025 Annual ODAC Dermatology Conference held January 17–20, 2025 in Orlando, FL. The above highlights from his lecture were written and compiled by Dr. Natalya Gallaga, Chief Resident in Dermatology at Tulane University. Dr. Gallaga was one of the five residents selected to participate in the Young Dermatology Leader Mentorship Program sponsored by Sun Pharma and organized by Derm In-Review.