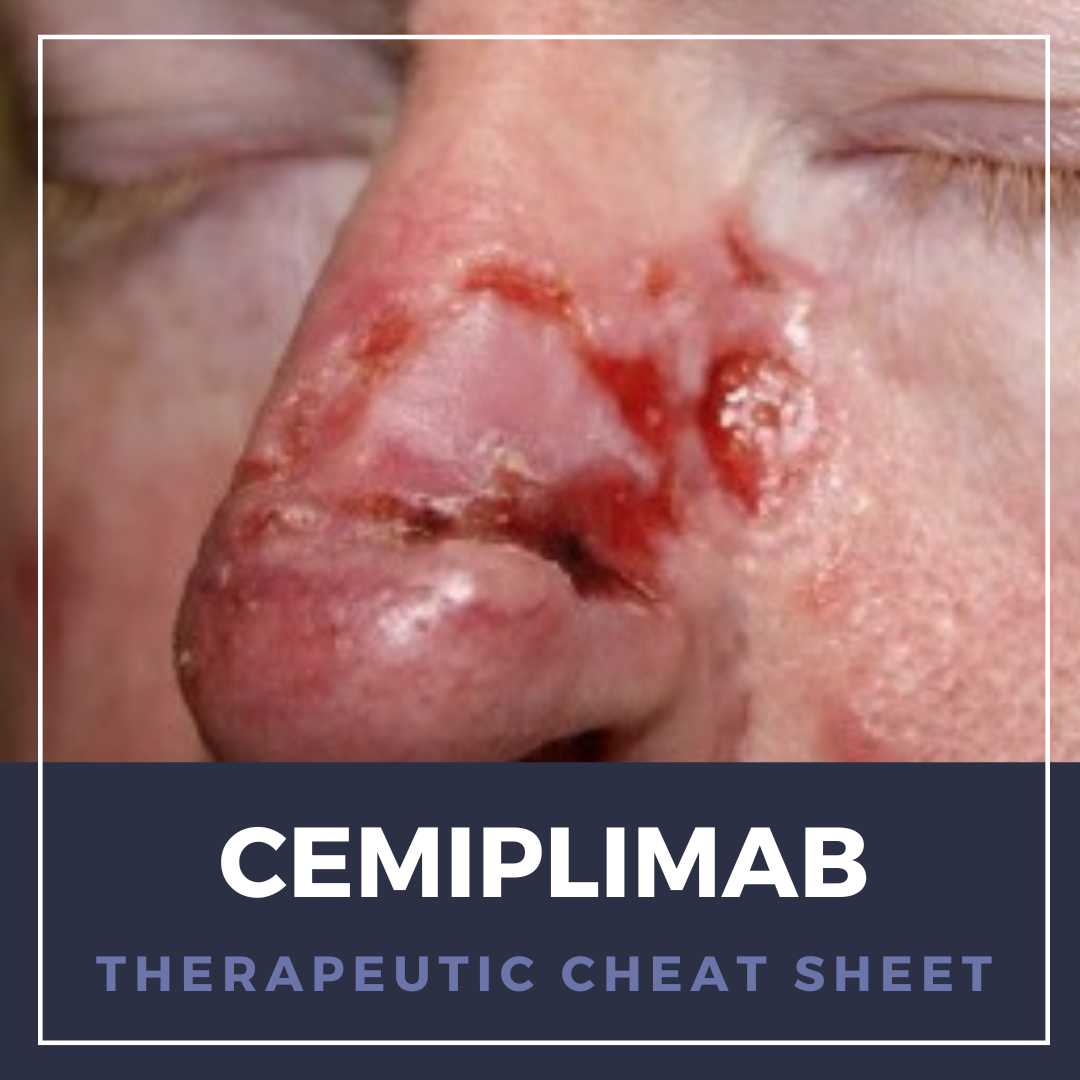
Cemiplimab is a monoclonal antibody therapy that has emerged as a promising treatment option for certain types of advanced skin cancer. Specifically designed to target the programmed cell death protein 1 (PD-1) pathway, cemiplimab works by blocking the interaction between PD-1 and its ligands, PD-L1 and PD-L2, thereby unleashing the body’s immune system to recognize and attack cancer cells. We continue our series, Therapeutic Cheat Sheet, with a closer look at cemiplimab, which is FDA-approved for the treatment of metastatic and locally advanced cutaneous squamous cell and basal cell carcinoma as well as non-small cell lung cancer.
Cemiplimab Therapeutic Cheat Sheet
Compiled by: Nidhi Shah, MD | Reviewed by: Adam Friedman, MD
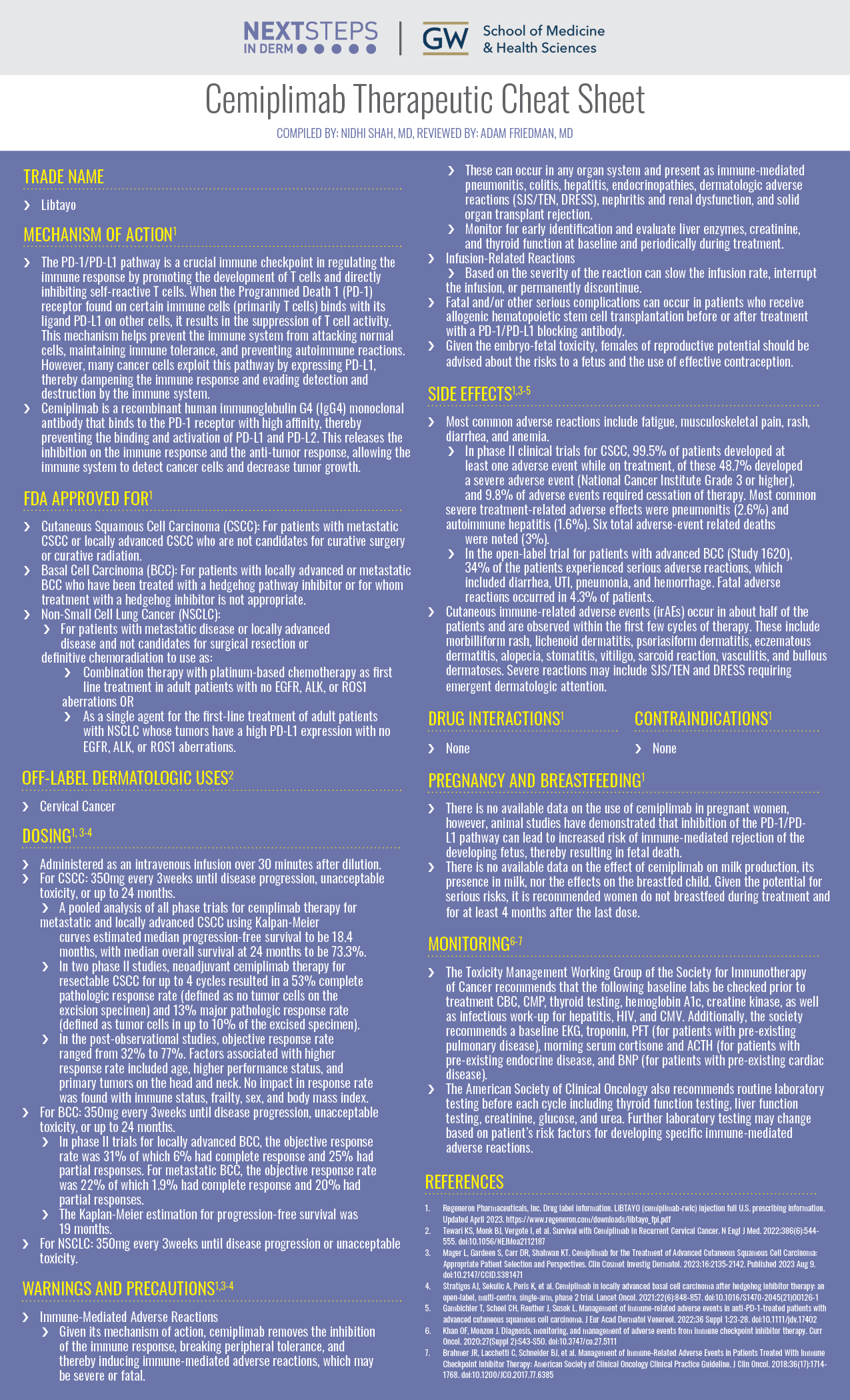
TRADE NAME
-
- Libtayo
MECHANISM OF ACTION1
-
- The PD-1/PD-L1 pathway is a crucial immune checkpoint in regulating the immune response by promoting the development of T cells and directly inhibiting self-reactive T cells. When the Programmed Death 1 (PD-1) receptor found on certain immune cells (primarily T cells) binds with its ligand PD-L1 on other cells, it results in the suppression of T cell activity. This mechanism helps prevent the immune system from attacking normal cells, maintaining immune tolerance, and preventing autoimmune reactions. However, many cancer cells exploit this pathway by expressing PD-L1, thereby dampening the immune response and evading detection and destruction by the immune system.
- Cemiplimab is a recombinant human immunoglobulin G4 (IgG4) monoclonal antibody that binds to the PD-1 receptor with high affinity, thereby preventing the binding and activation of PD-L1 and PD-L2. This releases the inhibition on the immune response and the anti-tumor response, allowing the immune system to detect cancer cells and decrease tumor growth.
FDA APPROVED FOR1
-
- Cutaneous Squamous Cell Carcinoma (CSCC): For patients with metastatic CSCC or locally advanced CSCC who are not candidates for curative surgery or curative radiation.
- Basal Cell Carcinoma (BCC): For patients with locally advanced or metastatic BCC who have been treated with a hedgehog pathway inhibitor or for whom treatment with a hedgehog inhibitor is not appropriate.
- Non-Small Cell Lung Cancer (NSCLC):
- For patients with metastatic disease or locally advanced disease and not candidates for surgical resection or definitive chemoradiation to use as:
- Combination therapy with platinum-based chemotherapy as first line treatment in adult patients with no EGFR, ALK, or ROS1 aberrations OR
- As a single agent for the first-line treatment of adult patients with NSCLC whose tumors have a high PD-L1 expression with no EGFR, ALK, or ROS1 aberrations.
- For patients with metastatic disease or locally advanced disease and not candidates for surgical resection or definitive chemoradiation to use as:
OFF-LABEL DERMATOLOGIC USES2
-
- Cervical Cancer
DOSING1,3-4
-
- Administered as an intravenous infusion over 30 minutes after dilution.
- For CSCC: 350mg every 3weeks until disease progression, unacceptable toxicity, or up to 24 months.
- A pooled analysis of all phase trials for cemplimab therapy for metastatic and locally advanced CSCC using Kalpan-Meier curves estimated median progression-free survival to be 18.4 months, with median overall survival at 24 months to be 73.3%.
- In two phase II studies, neoadjuvant cemiplimab therapy for resectable CSCC for up to 4 cycles resulted in a 53% complete pathologic response rate (defined as no tumor cells on the excision specimen) and 13% major pathologic response rate (defined as tumor cells in up to 10% of the excised specimen).
- In the post-observational studies, objective response rate ranged from 32% to 77%. Factors associated with higher response rate included age, higher performance status, and primary tumors on the head and neck. No impact in response rate was found with immune status, frailty, sex, and body mass index.
- For BCC: 350mg every 3weeks until disease progression, unacceptable toxicity, or up to 24 months.
- In phase II trials for locally advanced BCC, the objective response rate was 31% of which 6% had complete response and 25% had partial responses. For metastatic BCC, the objective response rate was 22% of which 1.9% had complete response and 20% had partial responses.
- The Kaplan-Meier estimation for progression-free survival was 19 months.
- For NSCLC: 350mg every 3weeks until disease progression or unacceptable toxicity.
WARNINGS AND PRECAUTIONS1,3-4
-
- Immune-Mediated Adverse Reactions
- Given its mechanism of action, cemiplimab removes the inhibition of the immune response, breaking peripheral tolerance, and thereby inducing immune-mediated adverse reactions, which may be severe or fatal.
- These can occur in any organ system and present as immune-mediated pneumonitis, colitis, hepatitis, endocrinopathies, dermatologic adverse reactions (SJS/TEN, DRESS), nephritis and renal dysfunction, and solid organ transplant rejection.
- Monitor for early identification and evaluate liver enzymes, creatinine, and thyroid function at baseline and periodically during treatment.
- Infusion-Related Reactions
- Based on the severity of the reaction can slow the infusion rate, interrupt the infusion, or permanently discontinue.
- Fatal and/or other serious complications can occur in patients who receive allogenic hematopoietic stem cell transplantation before or after treatment with a PD-1/PD-L1 blocking antibody.
- Given the embryo-fetal toxicity, females of reproductive potential should be advised about the risks to a fetus and the use of effective contraception.
- Immune-Mediated Adverse Reactions
SIDE EFFECTS1,3-5
-
- Most common adverse reactions include fatigue, musculoskeletal pain, rash, diarrhea, and anemia.
- In phase II clinical trials for CSCC, 99.5% of patients developed at least one adverse event while on treatment, of these 48.7% developed a severe adverse event (National Cancer Institute Grade 3 or higher), and 9.8% of adverse events required cessation of therapy. Most common severe treatment-related adverse effects were pneumonitis (2.6%) and autoimmune hepatitis (1.6%). Six total adverse-event related deaths were noted (3%).
- In the open-label trial for patients with advanced BCC (Study 1620), 34% of the patients experienced serious adverse reactions, which included diarrhea, UTI, pneumonia, and hemorrhage. Fatal adverse reactions occurred in 4.3% of patients.
- Cutaneous immune-related adverse events (irAEs) occur in about half of the patients and are observed within the first few cycles of therapy. These include morbilliform rash, lichenoid dermatitis, psoriasiform dermatitis, eczematous dermatitis, alopecia, stomatitis, vitiligo, sarcoid reaction, vasculitis, and bullous dermatoses. Severe reactions may include SJS/TEN and DRESS requiring emergent dermatologic attention.
- Most common adverse reactions include fatigue, musculoskeletal pain, rash, diarrhea, and anemia.
DRUG INTERACTIONS1
-
- None
CONTRAINDICATIONS1
-
- None
PREGNANCY AND BREASTFEEDING1
-
- There is no available data on the use of cemiplimab in pregnant women, however, animal studies have demonstrated that inhibition of the PD-1/PD-L1 pathway can lead to increased risk of immune-mediated rejection of the developing fetus, thereby resulting in fetal death.
- There is no available data on the effect of cemiplimab on milk production, its presence in milk, nor the effects on the breastfed child. Given the potential for serious risks, it is recommended women do not breastfeed during treatment and for at least 4 months after the last dose.
MONITORING6-7
-
- The Toxicity Management Working Group of the Society for Immunotherapy of Cancer recommends that the following baseline labs be checked prior to treatment CBC, CMP, thyroid testing, hemoglobin A1c, creatine kinase, as well as infectious work-up for hepatitis, HIV, and CMV. Additionally, the society recommends a baseline EKG, troponin, PFT (for patients with pre-existing pulmonary disease), morning serum cortisone and ACTH (for patients with pre-existing endocrine disease, and BNP (for patients with pre-existing cardiac disease).
- The American Society of Clinical Oncology also recommends routine laboratory testing before each cycle including thyroid function testing, liver function testing, creatinine, glucose, and urea. Further laboratory testing may change based on patient’s risk factors for developing specific immune-mediated adverse reactions.
FURTHER READING
If you would like to learn more about Cemiplimab, check out the following article in the Journal of Drugs in Dermatology:
Ravipati A, Pradeep T, and Nouri K.
Abstract
With immunotherapy historically focused on cutaneous melanoma, there has been a new wave of systemic medications available for treating non-melanoma skin cancers including basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and Merkel cell carcinoma (MCC). The immune checkpoint inhibitors approved by the FDA target programmed cell death protein 1 (PD-1) and the Hedgehog (Hh) signaling pathway. These medications have expanded treatment options; however, side effects are an important consideration. We used the FDA Adverse Events Reporting System (FAERS) to characterize the most prevalent, real-world side effects experienced by patients on these agents. Muscle spasms (23.45%), alopecia (16.06%), ageusia (12.02%), taste disorder (11.91%), and fatigue (11.67%) were the five most common side effects reported with medications used for BCC treatment. Logistic regression analysis showed males on vismodegib for BCC having greater odds of experiencing muscle spasms (aOR 1.33, P<0.001) and ageusia (aOR 1.34, P<0.001) versus females, who were more likely to exhibit alopecia (aOR 1.82, P<0.001) and nausea (aOR 1.96, P<0.001). With SCC treatment, the 5 most reported adverse events were fatigue (5.58%), rash (3.59%), asthenia (3.59%), pruritus (3.19%), and pyrexia (2.79%). Patients taking cemiplimab-rwlc for BCC compared to SCC were more likely to experience disease progression (aOR 10.98, P=0.02). With medication labels providing an excessively daunting list of side effects, we characterize practical side effects seen in patients receiving systemic treatments for non-melanoma skin cancers.
J Drugs Dermatol. 2024;23(5):301-305. doi:10.36849/JDD.7968
REFERENCES
-
- Regeneron Pharmaceuticals, Inc. Drug label information. LIBTAYO (cemiplimab-rwlc) injection full U.S. prescribing information. Updated April 2023. https://www.regeneron.com/downloads/libtayo_fpi.pdf
- Tewari KS, Monk BJ, Vergote I, et al. Survival with Cemiplimab in Recurrent Cervical Cancer. N Engl J Med. 2022;386(6):544-555. doi:10.1056/NEJMoa2112187
- Mager L, Gardeen S, Carr DR, Shahwan KT. Cemiplimab for the Treatment of Advanced Cutaneous Squamous Cell Carcinoma: Appropriate Patient Selection and Perspectives. Clin Cosmet Investig Dermatol. 2023;16:2135-2142. Published 2023 Aug 9. doi:10.2147/CCID.S381471
- Stratigos AJ, Sekulic A, Peris K, et al. Cemiplimab in locally advanced basal cell carcinoma after hedgehog inhibitor therapy: an open-label, multi-centre, single-arm, phase 2 trial. Lancet Oncol. 2021;22(6):848-857. doi:10.1016/S1470-2045(21)00126-1
- Gambichler T, Scheel CH, Reuther J, Susok L. Management of immune-related adverse events in anti-PD-1-treated patients with advanced cutaneous squamous cell carcinoma. J Eur Acad Dermatol Venereol. 2022;36 Suppl 1:23-28. doi:10.1111/jdv.17402
- Khan OF, Monzon J. Diagnosis, monitoring, and management of adverse events from immune checkpoint inhibitor therapy. Curr Oncol. 2020;27(Suppl 2):S43-S50. doi:10.3747/co.27.5111
- Brahmer JR, Lacchetti C, Schneider BJ, et al. Management of Immune-Related Adverse Events in Patients Treated With Immune Checkpoint Inhibitor Therapy: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2018;36(17):1714-1768. doi:10.1200/JCO.2017.77.6385
Did you enjoy this Therapeutic Cheat Sheet? You can find more here.