The association between vitiligo and melanoma is complex. While the incidence of vitiligo in patients with melanoma is higher, the risk for the reverse, ie, the development of melanoma in a patient with vitiligo, is thought to be decreased. This report presents a case of melanoma developing on a non-sun-exposed site in a patient with skin of color and untreated vitiligo. It emphasizes the need to think critically about vitiligo and melanoma pathogenesis.
CASE
A 63-year-old female patient with skin of color (Fitzpatrick skin type IV) and prior medical history of a cerebrovascular event, hypertension, hypercholesterolemia, and anxiety/depression presented to the dermatology office for “dark spots” on her trunk. She had no personal or family history of skin cancer. The patient reported having scalp hair loss that began approximately 10 years prior with associated areas of depigmentation noticed by her hairdresser. She had not started treatment for any skin or hair problems and had no prior autoimmune diagnoses.
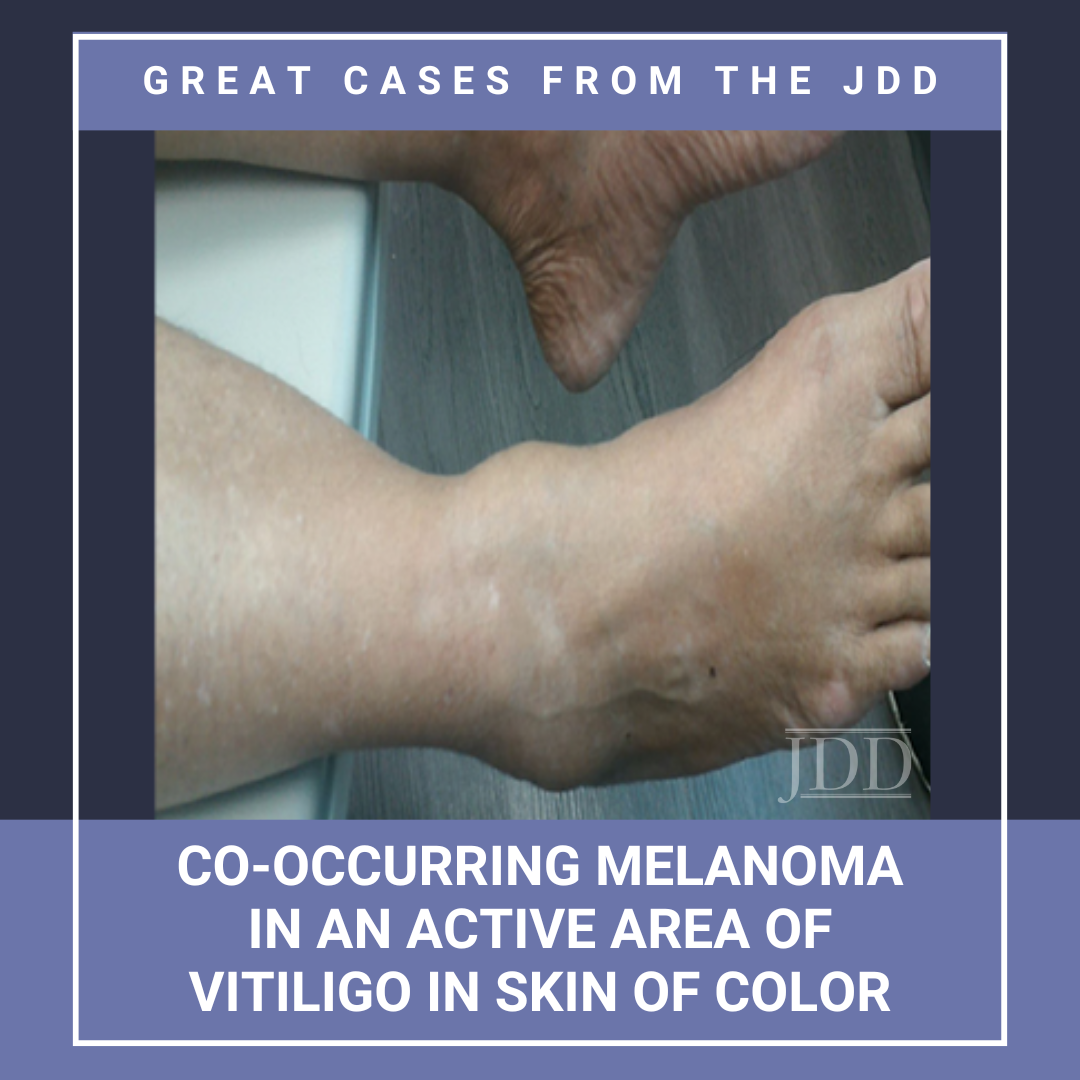
The lesions on her trunk relating to her chief complaint were consistent with seborrheic keratoses and solar lentigines. Her full body skin exam was otherwise significant for exclamation point hairs on the scalp consistent with alopecia areata, as well as depigmentation of the left frontoparietal scalp and right dorsal foot and ankle, consisting of <5% body surface area. At the edge of the depigmented patch on her dorsal foot, she had a <4 mm dark brown macule shown below (Figure 1). She reported wearing closed-toed shoes that covered the dorsal surfaces of her feet on a daily basis.

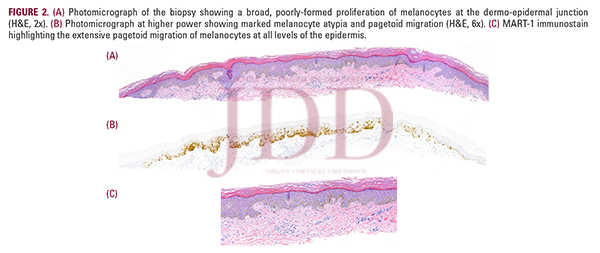
The macule of interest had an irregular rim on the lateral border with strikingly dark pigmentation, concerning for a melanocytic neoplasm. Shave biopsy of the macule was performed. Histopathologic examination showed poorly-formed proliferation of melanocytes at the dermo-epidermal junction and melanocyte atypia with pagetoid migration consistent with an early, evolving melanoma in situ (Figure 2).
DISCUSSION
The association between vitiligo and melanoma has been a subject of clinical and scientific interest. Vitiligo is a chronic disease characterized by depigmented patches on the skin due to the autoimmune destruction of melanocytes. Vitiligo is associated with other autoimmune diseases, including thyroid disease and alopecia areata, both of which were present in the patient.1 While patients with vitiligo are at higher risk of sunburns, they do not appear to be at increased risk for skin cancers. In fact, studies have reported a decreased risk of melanoma and non-melanoma skin cancers in patients with vitiligo.2-4 In contrast, patients with albinism, who have normal numbers of melanocytes but lack melanosomes, have a pronounced risk of skin cancer. The decreased susceptibility to skin cancers in vitiligo patients may be explained by the protective effects of genetic alterations found in some vitiligo patients.5
The incidence of vitiligo in melanoma patients has also been studied and appears to be much higher than the general population, up to 25.7%.6 “Melanoma-associated vitiligo,” “leukoderma in melanoma,” and “vitiligo-like depigmentation” all refer to the consequences of an antitumoral CD8+ T-cell response to melanoma that causes collateral destruction of normal melanocytes.7 These areas can present as halos in the area of the regressed primary melanoma, halos surrounding the primary tumor, halos around coexisting nevi, or widespread hypomelanosis at distant sites.8 Vitiligo incidence is especially elevated in those who have undergone immune checkpoint inhibition treatment for melanoma. The development of vitiligo is considered a good prognostic sign in melanoma patients.6Meanwhile, this is a unique report of the reverse: a patient developing melanoma in an area of active vitiligo. Vitiligo causes the immune system to target normal melanocyte differentiation antigens; thus, it is plausible that this could occasionally create a selective pressure to allow abnormal melanocytes to proliferate.8 This patient case raises the question of whether all vitiligo patients are genetically protected from skin cancers. Until we can distinguish patients at risk from those that are protected, regular skin cancer screening should be continued in all vitiligo patients.
REFERENCES
-
- Lee JH, Ju HJ, Seo JM, et al. Comorbidities in patients with vitiligo: a systematic review and meta-analysis. J Invest Dermatol. 2023;143(5):777-789 e776.
- Ferguson J, Eleftheriadou V, Nesnas J. Risk of melanoma and nonmelanoma skin cancer in people with vitiligo: United Kingdom population-based cohort study. J Invest Dermatol. 2023.
- Weng YC, Ho HJ, Chang YL, Chang YT, Wu CY, Chen YJ. Reduced risk of skin cancer and internal malignancies in vitiligo patients: a retrospective population-based cohort study in Taiwan. Sci Rep. 2021;11(1):20195.
- Teulings HE, Overkamp M, Ceylan E, et al. Decreased risk of melanoma and nonmelanoma skin cancer in patients with vitiligo: a survey among 1307 patients and their partners. Brit J Dermatol. 2013;168(1):162-171.
- Spritz RA. The genetics of generalized vitiligo: autoimmune pathways and an inverse relationship with malignant melanoma. Genome Med. 2010;2(10):78.
- Dousset L, Pacaud A, Barnetche T, et al. Analysis of tumor response and clinical factors associated with vitiligo in patients receiving anti-programmed cell death-1 therapies for melanoma: A cross-sectional study. JAAD Int. 2021;5:112-120.
- Le Gal FA, Avril MF, Bosq J, et al. Direct evidence to support the role of antigen-specific CD8(+) T cells in melanoma-associated vitiligo. J Invest Dermatol. 2001;117(6):1464-1470.
- Becker JC, Guldberg P, Zeuthen J, Brocker EB, Straten PT. Accumulation of identical T cells in melanoma and vitiligo-like leukoderma. J Invest Dermatol. 1999;113(6):1033-1038.
Source
Kim, Juliana H., et al. “Co-occurring Melanoma in an Active Area of Vitiligo in Skin of Color.” Journal of Drugs in Dermatology, vol. 24, no. 2, 2025, pp. 205-206. JDDonline, doi:10.36849/JDD.8115. Accessed 28 Jan. 2025.
Content and images used with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
Did you enjoy this JDD case report? You can find more here.