Cyclophosphamide, an alkylating agent introduced in the 1950s, has long served as a cornerstone therapy in rheumatology and oncology for its potent cytotoxic and immunosuppressive effects. In dermatology, it has been employed as a rescue agent for severe, refractory autoimmune and inflammatory skin diseases, particularly those associated with systemic connective tissue disorders. Its role spans conditions such as systemic lupus erythematosus, dermatomyositis, systemic sclerosis, ANCA-associated vasculitis, and autoimmune blistering disorders like pemphigus vulgaris and pemphigus foliaceus. Although now often supplanted by safer targeted therapies such as rituximab, mycophenolate, or IVIG, cyclophosphamide remains a valuable option in life-threatening or organ-threatening disease. Clinicians must weigh its efficacy against significant risks, including myelosuppression, hemorrhagic cystitis, infertility, infection, and secondary malignancies. Judicious use with careful monitoring and uroprotective strategies is essential.
We continue our “Therapeutic Cheat Sheet” series with a focused review of cyclophosphamide’s dermatologic applications, safety considerations, and practical prescribing pearls.
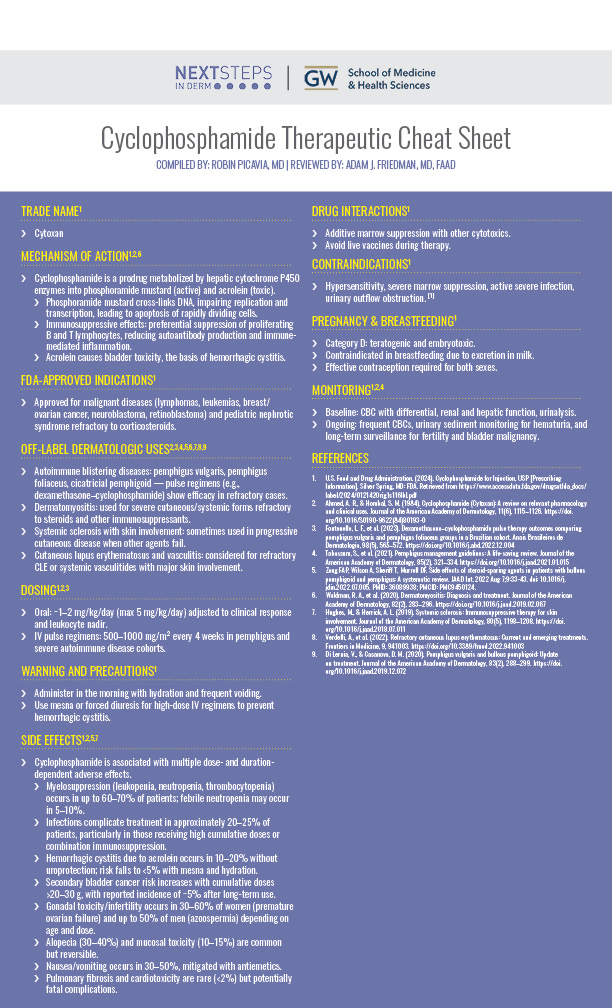
Cyclophosphamide Therapeutic Cheat Sheet
Compiled by: Robin Picavia, MD | Reviewed by: Adam J. Friedman, MD, FAAD
TRADE NAME1
Cytoxan
MECHANISM OF ACTION1,2,6
Cyclophosphamide is a prodrug metabolized by hepatic cytochrome P450 enzymes into phosphoramide mustard (active) and acrolein (toxic).
-
- Phosphoramide mustard cross-links DNA, impairing replication and transcription, leading to apoptosis of rapidly dividing cells.
- Immunosuppressive effects: preferential suppression of proliferating B and T lymphocytes, reducing autoantibody production and immune-mediated inflammation.
- Acrolein causes bladder toxicity, the basis of hemorrhagic cystitis.
FDA-APPROVED INDICATIONS1
Approved for malignant diseases (lymphomas, leukemias, breast/ovarian cancer, neuroblastoma, retinoblastoma) and pediatric nephrotic syndrome refractory to corticosteroids.
OFF-LABEL DERMATOLOGIC USES2,3,4,5,6,7,8,9
-
- Autoimmune blistering diseases: pemphigus vulgaris, pemphigus foliaceus, cicatricial pemphigoid — pulse regimens (e.g., dexamethasone–cyclophosphamide) show efficacy in refractory cases.
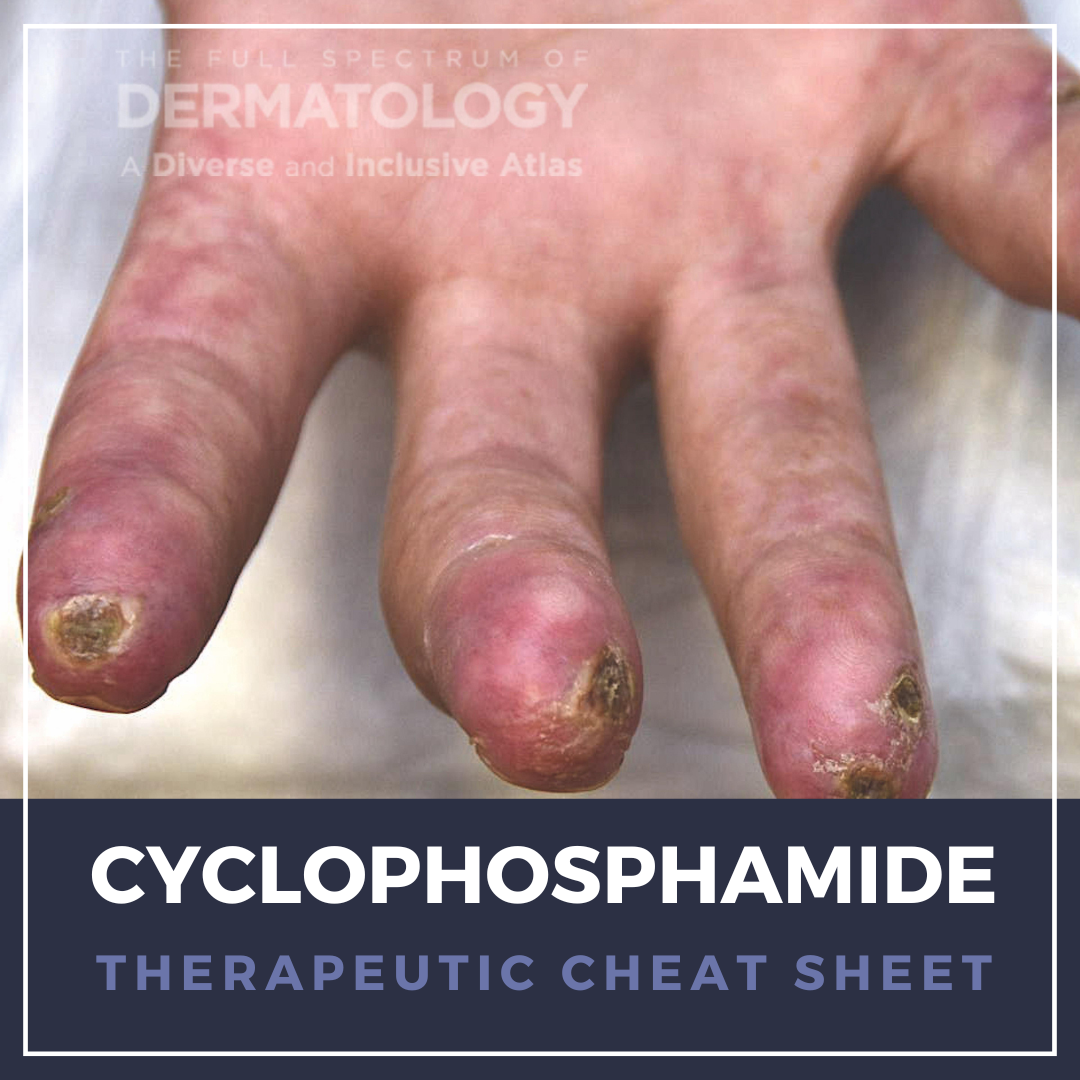
- Dermatomyositis: used for severe cutaneous/systemic forms refractory to steroids and other immunosuppressants.
- Systemic sclerosis with skin involvement: sometimes used in progressive cutaneous disease when other agents fail.
- Cutaneous lupus erythematosus and vasculitis: considered for refractory CLE or systemic vasculitides with major skin involvement.
DOSING1,2,3
-
- Oral: ~1–2 mg/kg/day (max 5 mg/kg/day) adjusted to clinical response and leukocyte nadir.
- IV pulse regimens: 500–1000 mg/m² every 4 weeks in pemphigus and severe autoimmune disease cohorts.
WARNING AND PRECAUTIONS1
-
- Administer in the morning with hydration and frequent voiding.
- Use mesna or forced diuresis for high-dose IV regimens to prevent hemorrhagic cystitis.
SIDE EFFECTS1,2,5,7
Cyclophosphamide is associated with multiple dose- and duration-dependent adverse effects.
-
- Myelosuppression (leukopenia, neutropenia, thrombocytopenia) occurs in up to 60–70% of patients; febrile neutropenia may occur in 5–10%.
- Infections complicate treatment in approximately 20–25% of patients, particularly in those receiving high cumulative doses or combination immunosuppression.
- Hemorrhagic cystitis due to acrolein occurs in 10–20% without uroprotection; risk falls to <5% with mesna and hydration.
- Secondary bladder cancer risk increases with cumulative doses >20–30 g, with reported incidence of ~5% after long-term use.
- Gonadal toxicity/infertility occurs in 30–60% of women (premature ovarian failure) and up to 50% of men (azoospermia) depending on age and dose.
- Alopecia (30–40%) and mucosal toxicity (10–15%) are common but reversible.
- Nausea/vomiting occurs in 30–50%, mitigated with antiemetics.
- Pulmonary fibrosis and cardiotoxicity are rare (<2%) but potentially fatal complications.
DRUG INTERACTIONS1
-
- Additive marrow suppression with other cytotoxics.
- Avoid live vaccines during therapy.
CONTRAINDICATIONS1
-
- Hypersensitivity, severe marrow suppression, active severe infection, urinary outflow obstruction. [1]
PREGNANCY & BREASTFEEDING1
-
- Category D: teratogenic and embryotoxic.
- Contraindicated in breastfeeding due to excretion in milk.
- Effective contraception required for both sexes.
MONITORING1,2,4
-
- Baseline: CBC with differential, renal and hepatic function, urinalysis.
- Ongoing: frequent CBCs, urinary sediment monitoring for hematuria, and long-term surveillance for fertility and bladder malignancy.
FURTHER READING
If you would like to read more about Cyclophosphamide, check out the following articles in the Journal of Drugs in Dermatology:
A brief primer on treatments of cutaneous T cell lymphoma, newly approved or late in development
Scheinfeld N. A brief primer on treatments of cutaneous T cell lymphoma, newly approved or late in development. J Drugs Dermatol. 2007 Jul;6(7):757-60. PMID: 17763605.
Abstract
Dermatologists use a variety of treatments for cutaneous T cell lymphoma (CTCL) or mycosis fungoides, in particular topical corticosteroids, psoralen and ultraviolet A phototherapy (PUVA) or ultraviolet B (UVB) phototherapy. Metastatic disease has been treated with radiotherapy, extracorporeal photophoresis, and old line chemotherapy agents such as methotrexate, chlorambucil, purine analogues, cyclophosphamide, hydroxydoxorubicin, oncovin, prednisone (CHOP), and interferon-alpha-2a. This feature will review these new agents including zanolimumab, denileukin diftitox, bexarotene, and vorinostat. Zanolimumab is a human monoclonal antibody that acts as a CD4 antagonist and has been granted orphan drug status in the US and Europe. Vorinostat (suberoylanilide hydroxamic acid) is a histone deacetylases inhibitor that has recently been approved by the FDA for the treatment of progressive, persistent, or recurrent CTCL on or after 2 systemic therapies have failed. Bexarotene is indicated in CTCL patients who are refractory to at least one prior systemic therapy. Denileukin diftitox is indicated for the treatment of patients with persistent or recurrent CTCL whose malignant cells express the CD25 component of the interleukin-2 receptor.
Pemphigus Vulgaris Successfully Treated With Bromocriptine
J Drugs Dermatol. 2024;23(3):e83-e85. doi:10.36849/JDD.7720e
Abstract
Pemphigus vulgaris (PV) is an autoimmune blistering skin condition primarily treated with immunosuppressive agents. We describe a case of PV successfully treated with nonconventional treatment, bromocriptine mesylate. Bromocriptine has been used in human trials showing beneficial therapeutic effects in managing autoimmune conditions. The results from experimental trials and the low toxicity of bromocriptine in comparison with immunosuppressive agents form a solid rationale for investigating its role in controlling PV.
REFERENCES
-
- S. Food and Drug Administration. (2024). Cyclophosphamide for Injection, USP [Prescribing Information]. Silver Spring, MD: FDA. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/012142Orig1s116lbl.pdf
- Ahmed, A. R., & Hombal, S. M. (1984). Cyclophosphamide (Cytoxan): A review on relevant pharmacology and clinical uses. Journal of the American Academy of Dermatology, 11(6), 1115–1126. https://doi.org/10.1016/S0190-9622(84)80193-0
- Fontenelle, L. F., et al. (2023). Dexamethasone–cyclophosphamide pulse therapy outcomes comparing pemphigus vulgaris and pemphigus foliaceus groups in a Brazilian cohort. Anais Brasileiros de Dermatologia, 98(5), 565–572. https://doi.org/10.1016/j.abd.2022.12.004
- Tabassum, S., et al. (2021). Pemphigus management guidelines: A life-saving review. Journal of the American Academy of Dermatology, 85(2), 321–334. https://doi.org/10.1016/j.jaad.2021.01.015
- Zeng FAP, Wilson A, Sheriff T, Murrell DF. Side effects of steroid-sparing agents in patients with bullous pemphigoid and pemphigus: A systematic review. JAAD Int. 2022 Aug 7;9:33-43. doi: 10.1016/j.jdin.2022.07.005. PMID: 36089938; PMCID: PMC9450124.
- Waldman, R. A., et al. (2020). Dermatomyositis: Diagnosis and treatment. Journal of the American Academy of Dermatology, 82(2), 283–296. https://doi.org/10.1016/j.jaad.2019.02.067
- Hughes, M., & Herrick, A. L. (2019). Systemic sclerosis: Immunosuppressive therapy for skin involvement. Journal of the American Academy of Dermatology, 80(5), 1198–1208. https://doi.org/10.1016/j.jaad.2018.07.011
- Verdelli, A., et al. (2022). Refractory cutaneous lupus erythematosus: Current and emerging treatments. Frontiers in Medicine, 9, 941003. https://doi.org/10.3389/fmed.2022.941003
- Di Lernia, V., & Casanova, D. M. (2020). Pemphigus vulgaris and bullous pemphigoid: Update on treatment. Journal of the American Academy of Dermatology, 83(2), 288–299. https://doi.org/10.1016/j.jaad.2019.12.072
Did you enjoy this Therapeutic Cheat Sheet? You can find more here.