Health recently posted an article on the causes of melanonychia. While a black line on a patient’s nail is a common presentation, melanonychia may have a harmless cause or it may be a sign of a more serious health condition. How should a dermatology clinician conduct a workup for melanonychia, and when is a biopsy necessary?
For an expert’s take, I reached out to Molly Hinshaw, MD, professor of dermatology, section chief of dermatopathology and director of the nail clinic at the University of Wisconsin School of Medicine and Public Health. Dr. Hinshaw will lecture on melanonychia at the ODAC Dermatology Conference to be held January 17-20, 2025, in Orlando.
How commonly do you see melanonychia in your nail clinic?
Melanonychia is a very common presentation to the nail clinic and dermatology in general. Patients often notice it, become alarmed by it, and seek our care.
What are some of the many causes of melanonychia?
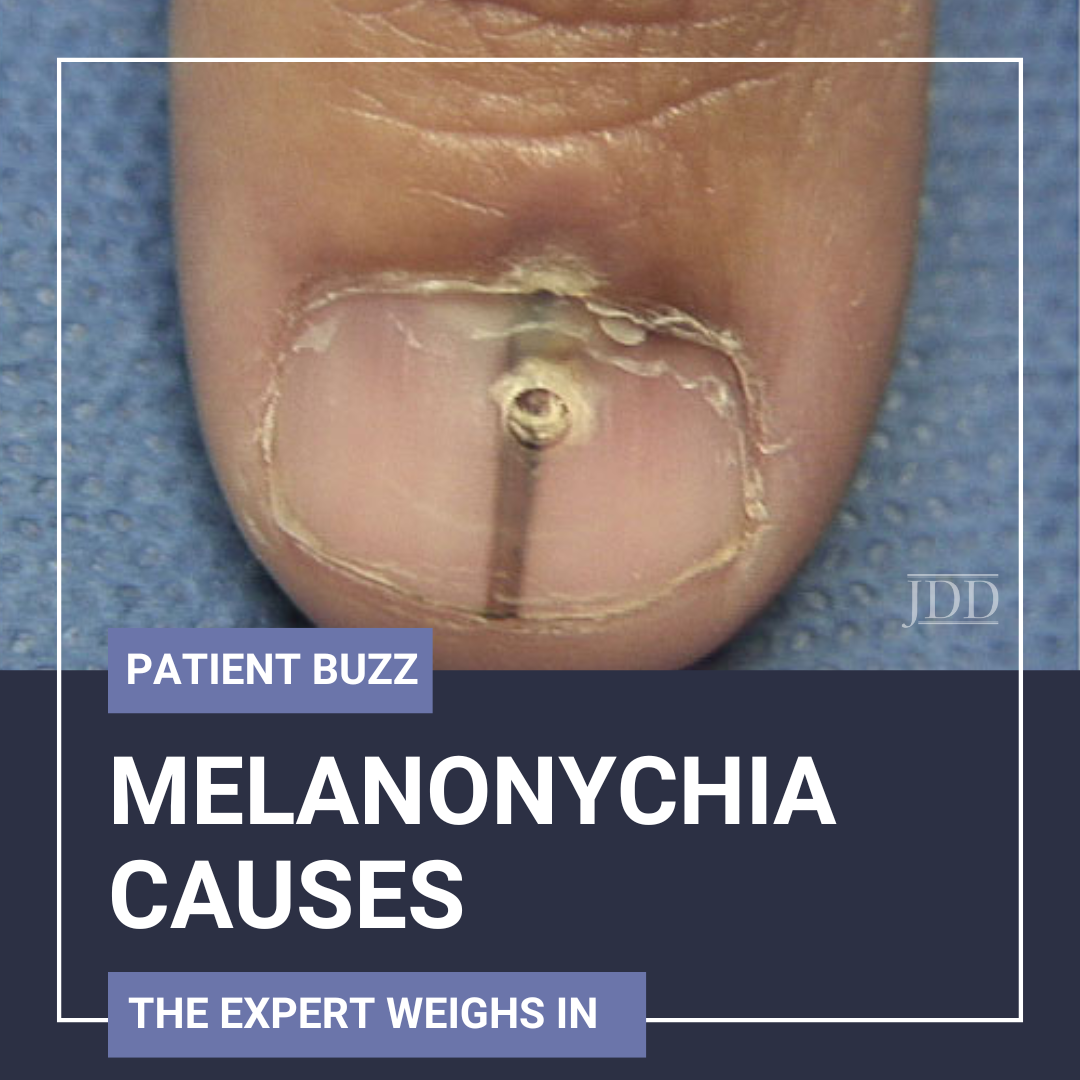
Melanonychia is caused by two primary factors: increased melanin pigment in the nail matrix (melanocyte activation) or an increase in the number of melanocytes in the nail matrix (e.g. melanoma, melanocytic nevus, lentigo). Melanocyte activation may affect one or multiple digits and is caused by triggers. Melanocyte activation can be identified by a thorough history and review of systems, and by its usual grey/brown color, uniformity and lack of individual pigmented bands on dermoscopy within the broader melanonychia.
Melanocytic lesions usually present as one nail affected by a pigmented band that has within it individual pigmented bands. Depending on a variety of other factors, melanocytic lesions can usually be anticipated to be benign (<3mm broad or <40% the breadth of the nail, no extension of pigment onto the skin surrounding the nail, etc.) or malignant. Two large caveats to this include patients with skin of color in whom melanonychia affecting multiple digits can be clinically different (darker, broader, etc.) than in Caucasians yet still benign and pediatric patients in whom melanonychia of a single digit due to a melanocytic lesion is usually benign even when it has worrisome features. Clearly we have more work to do to clinically (without a biopsy) to diagnose the cause of melanonychia particularly in these groups. There are other reasons for the nails to discolor (e.g. pigment producing fungi, hemorrhage) but these are not caused by melanin pigment as melanonychia is and can be distinguished from melanonychia on dermoscopy.
What lab tests should dermatology clinicians consider when a patient presents with melanonychia?
If melanonychia has atypical features (currently we still primarily consider atypical features to be the ABCDEFs), then a tangential shave biopsy of the matrix is warranted to exclude melanoma.
What else is important for dermatology clinicians to know about melanonychia?
Most studies of nail unit melanoma show that even when a clinician biopsies melanonychia due to a clinical concern for melanoma, about 70% of these lesions are benign and therefore it is important that we use good surgical technique to obtain these specimens and give patients the best chance of healing with a highly functional nail afterward. It is better to schedule the patient within a couple weeks to return to clinic for tangential shave biopsy than, for example, to do a punch biopsy through the proximal nail fold to the matrix because this latter approach lacks visualization of the matrix lesion and will lead to a permanent split in the nail for a lesion that may be benign.
Did you enjoy this Patient Buzz Expert Commentary? You can find more here.