Permethrin is a synthetic neurotoxic pyrethroid derived from chrysanthemums with significant dermatologic value for its powerful insecticide properties when used topically. We continue our series, Therapeutic Cheat Sheet, with a closer look at permethrin, which is FDA-approved for the treatment of scabies and pediculosis capitis infestations.
Permethrin Therapeutic Cheat Sheet
Compiled by: Dillon Nussbaum, MD | Reviewed by: Adam Friedman, MD
TRADE NAME
-
- Elimite
- Acticin
- Nix
MECHANISM OF ACTION4,6
-
- Binds to voltage-gated sodium ion channels in the nerve membranes of arthropods, which disrupts sodium transport by inducing depolarization, delaying repolarization, and ultimately causing respiratory paralysis in affected arthropods.
FDA APPROVED FOR4,6
-
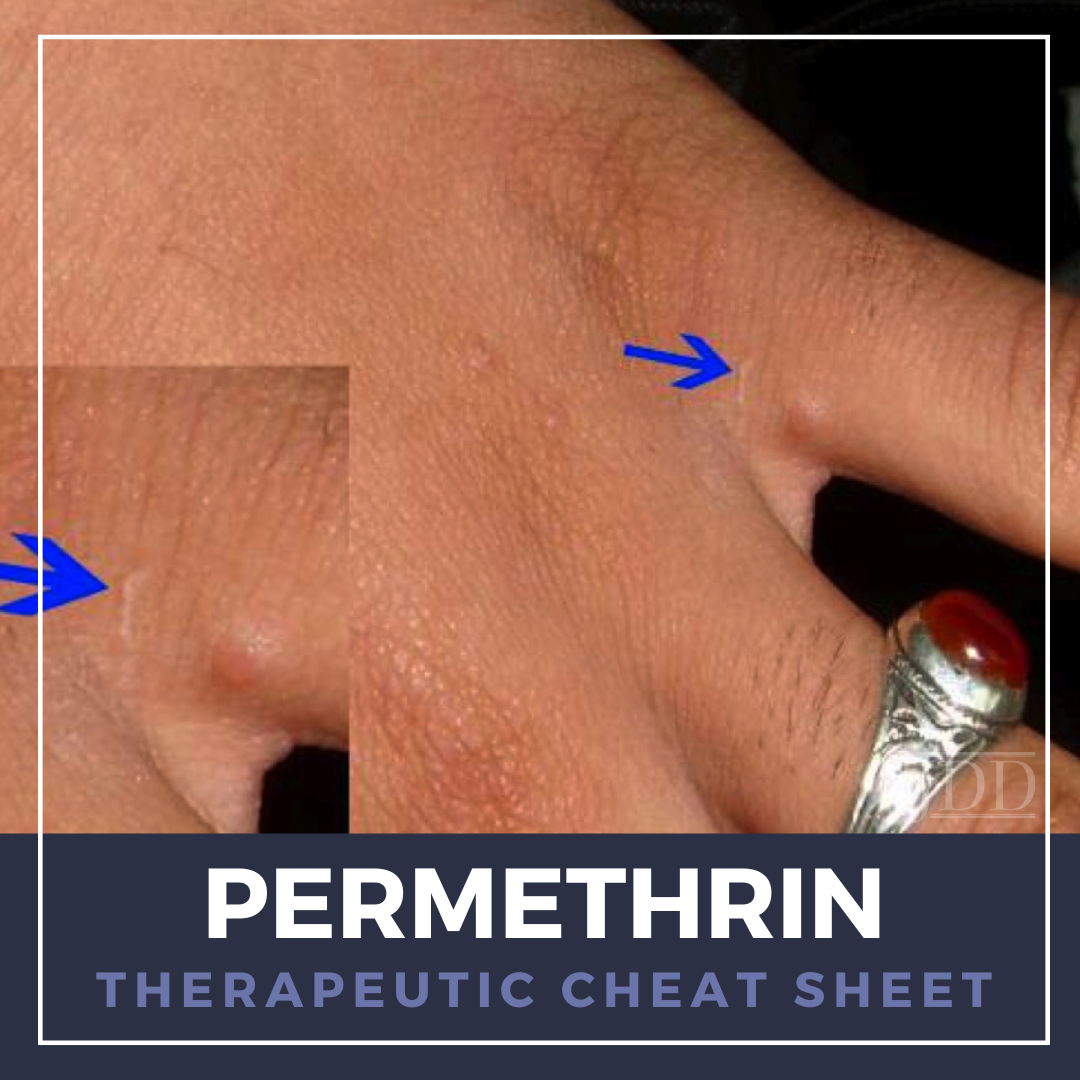
- Scabies
- Pediculosis capitis
OFF-LABEL DERMATOLOGIC USES2,6
-
- Pediculosis pubis
- Pediculosis corporis
- Cutaneous larva migrans
- Demodex infestations
- Periorofacial dermatitis
- Cutaneous myiasis
DOSING4,6,7
-
- Topical 1% cream/lotion (over the counter)
- Pediculosis infestations: for infants ≥ 2 months or adults: wash hair with conditioner free shampoo, rinse and dry, then apply enough cream or lotion to saturate the hair and scalp, including behind the ears and nape of the neck, or other affected areas, leave in hair for 10 minutes, then rinse off with warm water, remove remaining nits with a nit comb. A single application is usually sufficient; however, may repeat regimen 7 days later if nits still present.
- Topical 5% (prescription only)
- Scabies: for infants ≥ 2 months or adults: apply to the entire body neck to soles of the feet, leave on for 8 to 14 hours before removing by washing. In infants or older adults, apply to the hairline, neck, scalp, temple, and forehead. One application is generally curative; however may repeat in 14 days if living mites still present.
- Crusted Scabies: for infants ≥ 2 months: apply to the entire body neck to soles of the feet, leave on for 8 to 14 hours before removing by washing, repeat daily for 7 days and then twice weekly until symptoms have resolved. Use in combination with ivermectin on days 1, 2, 8, 9, and 15 (and potentially on days 22 and 29 for severe cases).
- Topical 1% cream/lotion (over the counter)
SIDE EFFECTS4-6
-
- Ocular: Conjunctival pain, redness, discharge, or chemosis
- Cutaneous: Allergic or irritant contact dermatitis, eczema flares
DRUG INTERACTIONS4,6
-
- Permethrin has no known severe, serious, moderate, or mild interactions with other drugs
CONTRAINDICATIONS4-6
-
- Known hypersensitivity to any of its components, to any synthetic pyrethroid or pyrethrin
- Avoid direct contact with the eyes
- Do not use permethrin on broken or secondarily infected skin
- Reported toxicity in cats
PREGNANCY AND BREASTFEEDING3,6
-
- There is no evidence that permethrin poses an increased risk to the fetus, and animal studies have not shown impaired fertility or harm to the fetus
- Permethrin is safe to use in breastfeeding women as follows: The nipple area should be cleaned of any topical products before a baby attaches to the breast to feed. Reapply the product to the washed area after feeding
- Because less than 2% is absorbed after topical application, rapid metabolism to inactive metabolites and safe application directly on infants’ skin, topical permethrin products are acceptable in nursing mothers
MONITORING6
-
- Per European guidelines, patients with scabies should return for a follow-up 2 weeks after treatment has ended to assess resolution

FURTHER READING
If you would like to learn more about permethrin, check out the following articles published in the Journal of Drugs in Dermatology:
Treatment of Scabies Using 8% and 10% Topical Sulfur Ointment in Different Regimens of Application
Sharquie ,J. Al-Rawi, A. Noaimi, and H. Hassany
Abstract:
Many therapeutic modalities for scabies were available, topical sulfur ointment is a cost-effective and safe therapeutic agent. It is often applied for the whole body for three successive days. To evaluate their therapeutic regimen of 8% and 10% topical precipitated sulfur in petrolatum ointment for single day, three successive nights or three successive days in management of scabies. This single-blinded, comparative study was conducted in the Department of Dermatology-Baghdad Teaching Hospital from April 2008 through October 2009. A total of 97 patients with scabies were enrolled in this study. The diagnosis was established on clinical basis. The patients treated with 8% and 10% topical sulfur in petrolatum ointment were divided randomly into three groups: Group A: 33 patients treated for single day (24 hours); Group B: 32 patients treated for three successive nights (from 6 p.m. to 8 p.m. to 6 a.m. to 8 a.m. and bathing every day); and Group C: 32 patients treated for three successive days (bathing every 24 hours). The patients were seen regularly every two weeks for the duration of four weeks. Study included 58 (59.8%) males and 39 (40.2%) females, with a male to female ratio 1.4:1. The age range of males at presentation from 3 to 64 (26.74±15.98) years, while the females age ranged at presentation from 3 to 60 (24.05±14.53) years of age. At the end of the study, the response to treatment was: Group A, response in 14 (42.4%) patients and no response in 19 (57.6%); Group B, response in 29 (90.6%) patients and no response in 3 (9.4%); and Group C, response in 31 (96.9%) patients and no response in 1 (3.1%). There is significant statistical difference among the response of 3 groups with (P=0.00000011), but no statistically significant difference between the response of Group C and Group B, (P=0.6055). Mild burning sensation and irritating (sulfur) dermatitis were the only side effects of 8% and 10% sulfur. Pruritic rash occurred in Group C mainly, in 11 (34.4%) patients, 8 (25%) in Group B and 4 (12.1%) in Group A, with no significance (P=0.1058). Recurrence or relapse occurred in Group A mainly, with 4 (12.1%) patients, and in Group B, 1 patient, (3.1%), with no recurrence in group C, with significance (P=0.0060). Three successive days and three successive nights of 8% and 10% sulfur ointment were effective regimens with no statistical difference in favor of three successive days, while single-day application was much less effective but with fewer side effects.
J Drugs Dermatol. 2012;11(3):357-364.
Malathion for Head Lice and Scabies: Treatment and Safety Considerations
Idriss and J. Levitt
Abstract:
Malathion is an under-recognized and under-utilized therapy for head lice and scabies largely due to misperceptions about its safety profile. Specifically, its pure form as it exists in pharmaceutical preparations is non-toxic to humans in the low doses available. While labeled for ages six and up, recent studies showed no cholinesterase inhibition in head lice patients aged two-to-six treated with malathion. Flammability of malathion in isopropyl alcohol has reportedly resulted in human injury once in over one million prescriptions filled. Recent efficacy studies of malathion in United States (U.S.) head lice demonstrate efficacy rates of 97 to 98%. In the present era of permethrin and lindane resistance to head lice, malathion is a first-line option. For scabies, it is a reasonable alternative to permethrin 5% cream, especially when treatment of the scalp or hairy areas is desired.
J Drugs Dermatol. 2009;8(8):715-720.
References
-
- Boland, L. A., & Angles, J. M. (2010). Feline permethrin toxicity: retrospective study of 42 cases. Journal of feline medicine and surgery, 12(2), 61–71.
- Cardoso, A. E. C., Cardoso, A. E. O., Talhari, C., & Santos, M. (2020). Update on parasitic dermatoses. Anais brasileiros de dermatologia, 95(1), 1–14.
- Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-. Permethrin. [Updated 2024 Nov 15].
- Nanda, J., Patel, P., & Juergens , A. L. (2024). Permethrin. In StatPearls. StatPearls Publishing.
- National Research Council (US) Subcommittee to Review Permethrin Toxicity from Military Uniforms. Health Effects of Permethrin-Impregnated Army Battle-Dress Uniforms. Washington (DC): National Academies Press (US); 1994. 6 Neurotoxicity of Permethrin.
- In: UpToDate, Connor RF (Ed), Wolters Kluwer.
- Rosumeck, S., Nast, A., & Dressler, C. (2018). Ivermectin and permethrin for treating scabies. The Cochrane database of systematic reviews, 4(4), CD012994.
Did you enjoy this Therapeutic Cheat Sheet? You can find more here.