Dermatologists play a crucial role in the care of patients with sexually transmitted diseases (STDs), as many STDs manifest on the skin. At the 2024 Skin of Color Update, Dr. Theodore Rosen, Professor of Dermatology at Baylor College of Medicine, shared valuable insights on diagnosing and managing STDs in patients with skin of color. This article reviews the prevalence of STDs, their distinctive presentations, screening methods, and treatment strategies in these populations.
STD Statistics in Patients with Skin of Color
Each year, approximately 2.5 million STD cases are diagnosed in the United States. In 2022, Hispanic Black or African American patients—who make up just 13% of the U.S. population—accounted for 31.1% of all cases of chlamydia, gonorrhea, and primary and secondary syphilis.1 Additionally, STD rates among Alaska Natives and Native American people have risen, likely resulting from limited access to and knowledge of STD care.
Syphilis Trends by Ethnicity
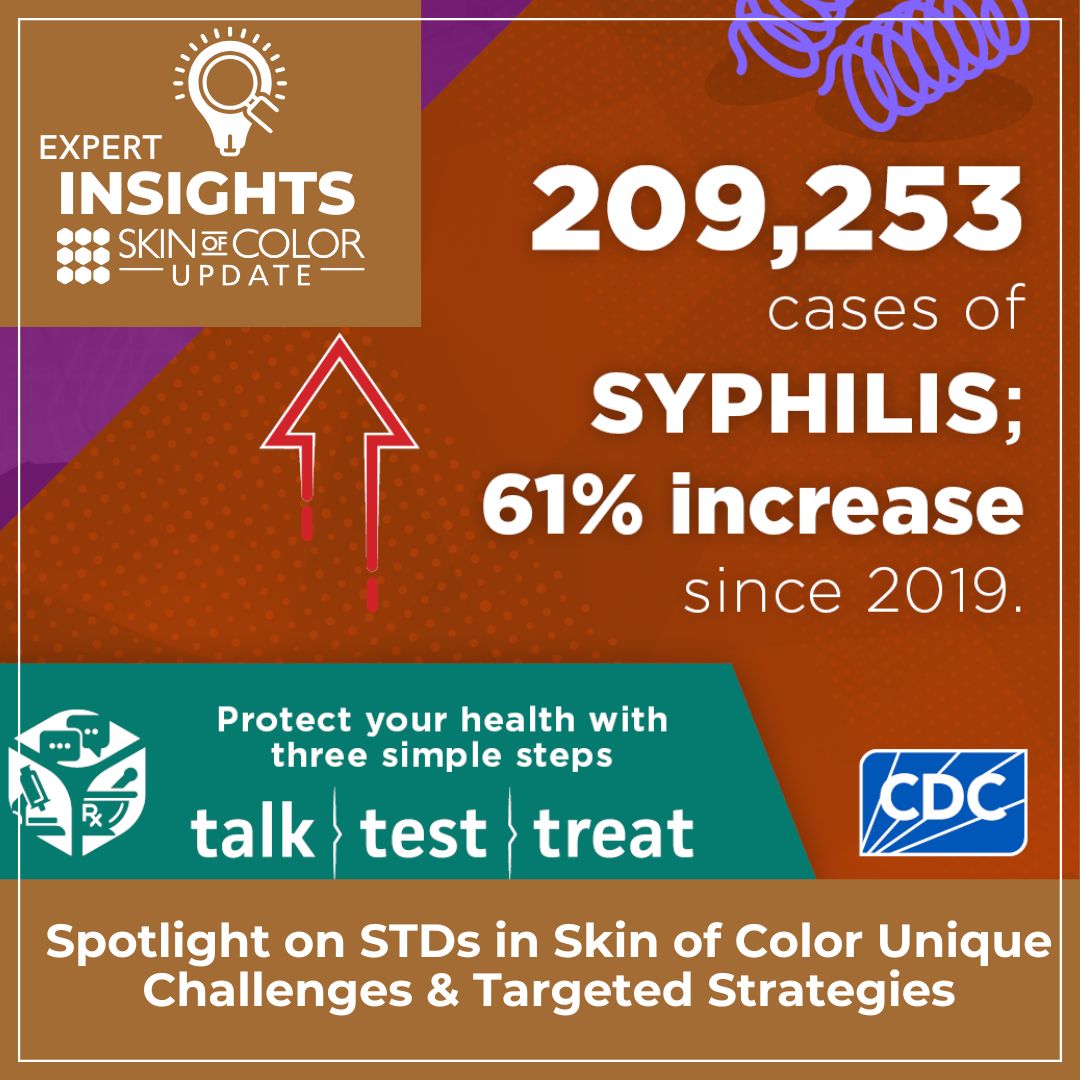
Dr. Rosen emphasized the alarming rise in syphilis rates across the U.S. Between 2021 and 2022, new cases of primary, secondary, and congenital syphilis increased by 17%. In 2022 alone, a record high of 3,769 congenital syphilis cases was reported nationwide. ²
States with the highest numbers of new syphilis cases annually include California, Florida, Texas, and New York. Notably, states with large populations of federally recognized American Indian and Alaska Native tribes—such as South Dakota, New Mexico, Arkansas, and Oklahoma—report higher syphilis rates per 100,000 adults compared to other states.³ These findings highlight the disproportionate impact of syphilis among patients with skin of color, many of whom face barriers to accessing STD care.
American Indians and Alaska Natives were at the highest risk for primary and secondary syphilis in 2022, followed by African Americans and Hispanics. These disparities underscore the need for targeted interventions to improve STD care and prevention in skin of color communities.
Primary and Secondary Syphilis Presentation in Skin of Color
The typical primary lesion of syphilis manifests as a solitary, painless, indurated, and clean ulcer. However, both primary and secondary syphilis can present with atypical lesions, particularly in patients with skin of color. In these populations, secondary syphilis may mimic other skin conditions, such as psoriasis, and can also appear as nodular lesions. Annular secondary syphilis is a unique presentation seen in Black and Hispanic patients, characterized by lesions around the eyes, nose, and mouth.
Additionally, 2% to 5% of secondary syphilis cases involve alopecia,4 and approximately 5% of primary chancres are extragenital,5 often appearing on the lips or tongue. Recognizing these atypical presentations is critical for accurate diagnosis and timely treatment.
Congenital Syphilis
In 2022, there were 3755 cases of congenital syphilis leading to 231 stillbirths and 51 perinatal deaths. (Graph). States with higher proportions of Black, Hispanic, and skin-of-color patients in the Southwestern United States—such as California, Arizona, Oklahoma, Louisiana, Georgia, and Florida—had the greatest incidence of congenital syphilis. Early diagnosis of syphilis is important in this patient population to reduce rates of congenital syphilis.
Monkeypox
The rate of this sexually transmitted disease has greatly decreased since December 2022; however, there are still 6-12 new cases daily in the U.S. The antiviral tecovirimat is used off-label to treat monkeypox, but there is developing resistance to this therapy. Monkeypox disproportionately affects Black and Hispanic men who have sex with men. ⁶ Full vaccination requires a two-dose regimen and is unfortunately not readily available. Education of patients of color who are at highest risk is imperative. 1.6% of cases are seen in women, presenting as a pustule that becomes crusted and can be very uncomfortable.
HSV
Overall, seropositivity of HSV has decreased from about 20% to 12% in recent years. Similar to other conditions mentioned, non-Hispanic Black individuals are disproportionately affected compared to other ethnic groups. Seropositivity indicates genital herpes but does not dictate how often a patient sheds the virus. Patients can still shed the virus in the absence of lesions or symptoms.
Hypertrophic or Vegetative Genital Herpes (HSV-2)
This presentation of HSV-2 is often seen in immunocompromised patients, such as those with HIV or individuals on immunosuppressive therapy. It is more likely to be seen in patients with skin of color, particularly Black individuals. Differential diagnoses include condyloma lata, condyloma acuminata, and malignancies. A biopsy, appropriate immunostaining, or viral culture (PCR) is necessary to establish the diagnosis. Treatment requires multimodal therapy. Often, the diagnosis of hypertrophic genital herpes leads to a retrospective diagnosis of HIV.
Minor STDs
The Department of Health and Human Services removed three diseases from the list of communicable diseases of significant public health concern:
-
- Chancroid: <20 cases annually since 2011, seen primarily in individuals from Africa, the Caribbean, or visitors from the U.S. to these regions.
- Donovansis/granuloma inguinale: <100 cases annually since 2011, with fewer than 10 cases reported in the U.S. since 2018. Seen in individuals who have visited Africa, India, or Papua New Guinea. The lesions are destructive yet painless.
- Lymphogranuloma venereum: <20 cases annually since 2018, most commonly seen in men who have sex with men (MSM). Lesions resemble syphilis and should be suspected in patients who present with negative syphilis serology.
STD Testing
Patients can be referred to https://gettested.cdc.gov to locate clinic facilities for free testing for syphilis, gonorrhea, chlamydia, HSV, and hepatitis C. For those who do not want to go to a clinic or prefer at-home testing, there are multiple options to secure commercial kits. They are confidential, and only a fingerstick blood sample, urine sample, and vaginal swab (if appropriate) are needed.
In summary, Dr. Rosen emphasized the rising prevalence of STDs in patients with skin of color, underscoring the need for targeted care and improved access to resources. Early detection plays a crucial role in preventing congenital syphilis, while education on prevention and vaccination is vital for managing diseases like monkeypox and HSV.
References
-
- https://www.cdc.gov/sti-statistics/media/pdfs/2024/11/2022-STI-Surveillance-Report-PDF.pdf
- https://www.cdc.gov/sti-statistics/data-vis/table-trends.html
- https://www.cdc.gov/sti-statistics/data-vis/table-syph-total-state-abc.html
- Vafaie J, Weinberg JM, Smith B, Mizuguchi RS. Alopecia in association with sexually transmitted disease: a review. Cutis. 2005;76(6):361-366.
- Dourmishev LA, Dourmishev AL. Syphilis: uncommon presentations in adults. Clin Dermatol. 2005;23(6):555-564.
- Kota KK, Hong J, Zelaya C, et al. Racial and ethnic disparities in mpox cases and vaccination among adult males – united states, may-december 2022. MMWR Morb Mortal Wkly Rep. 2023;72(15):398-403.
This information was presented by Dr Theodore Rosen at the 2024 Skin of Color Update Conference, held September 13-15, 2024. The above highlights from his lecture were written and compiled by Dr. Osuoji.
Did you enjoy this article? You can find more on Skin of Color Dermatology here.