Dr. Vishal Patel (Assistant Professor of Dermatology and Director of the Cutaneous Oncology Program at George Washington University School of Medicine and Health Sciences) gave a thought-provoking talk at the 2022 ODAC Dermatology, Aesthetic & Surgical Conference about something we do nearly every day as dermatologists – full body skin exams. He started by reviewing the rising epidemic of skin cancer, followed by population-based data on the effectiveness and value of skin cancer screening.
Statistics on Skin Cancer – A Public Health Crisis:
Skin cancer is very expensive, with an annual cost of more than $8 billion. The cost is on the rise as well, as the incidences of both keratinocyte carcinomas and melanoma are increasing. In 2012, among Medicare patients alone, over 1 million basal cell carcinomas (BCC) and 1 million squamous cell carcinomas (SCC) were diagnosed.1 As for melanoma, roughly 75,000 cases of melanoma and 55,000 cases of melanoma in situ (MIS) were diagnosed in 2013. Over the last decade, the incidence of melanoma increased by about 38% and the incidence of MIS increased even more – by about 80%. Despite this increase, melanoma deaths have decreased, with around 7,100 deaths in 2021 compared to 9,400 in 2013; deaths from SCC may even overtake melanoma this year. Further, a 2021 study in the New England Journal of Medicine showed that the observed incidence of melanoma is much higher than the worst-case expectation estimate.2 Based on the discrepancy between melanoma incidence and mortality, Dr. Patel questioned – is there a diagnostic disconnect? Are we doing too many biopsies?
Regardless of the exact numbers and whether over-diagnosis is contributing, we can all agree that skin cancer is a public health crisis. Dr. Patel estimated that 1-2% of all SCCs and 6.7% of all invasive melanomas will lead to death. In addition to the mortality of skin cancer, the huge cost associated with these cancers is problematic, and estimates do not even include the costs of skin cancer screening and actinic damage treatment.
Cancer Prevention Strategies:
Given this public health crisis, the meat of Dr. Patel’s talk focused on the big question – do skin cancer screenings help identify and prevent deaths from skin cancer? By providing evidence-based care in a more targeted approach, dermatologists can provide high quality care while curtailing population-based costs. Skin cancer screenings are a form of secondary prevention, meaning we are trying to detect a disease early and prevent it from worsening. Essentially, we are trying to diagnose skin cancers when they are easy to treat. Logically, it makes sense that early identification would be useful, but we need to look at the data.
Back to the main question, does skin cancer screening help? Screenings are not recommended for the general population by the United States Preventive Services Taskforce or Australian Department of Health, but we need to dive into the data. Before doing this, Dr. Patel reviewed the anatomy of screening. Sensitivity describes the ability to correctly identity people with the disease and specificity describes the ability to correctly identify people who do not have the disease. A systematic review by Chen et al. reported a sensitivity for skin cancer screenings ranging from 42 to 100% with a specificity of 98%.3 Similarly, an Australian study reported a lower sensitivity of screening (49%) and a higher specificity (98%).4 However, these metrics are difficult to estimate given we cannot determine if a negative screening is truly negative. Further, sensitivity and specificity are characteristics of the test, rather than utilization of the test. Therefore, variability in the performance of a total body skin exam (TBSE) among dermatologists, which we all know is high, alters sensitivity and specificity.5
So, how do we increase the accuracy of our exams? Dermoscopy helps, but Dr. Patel warned that this is only the case if you are an expert. In one meta-analysis on the diagnosis of melanoma, sensitivity increased by 16% and specificity increased by 20% with the use of dermoscopy compared to visual inspection alone. 6
Screening Costs:
Now we know that it is difficult to assess how well TBSEs rule in and rule out skin cancer, but what about the cost? Hartman et al. used modeling to estimate the cost of skin cancer screenings and Dr. Patel highlighted three take home points from the study.7
-
- The number needed to examine to find one skin cancer (melanoma and keratinocyte carcinoma) is 105. This number decreased with increasing age and lighter skin types.
- There was an additional cost of $3,796 per skin cancer detected when performing TBSEs on patients who presented for a focused exam. Similarly, the cost goes down with increasing age and lighter skin types.
- There is a lot of time added to perform skin cancer screening: it takes 38 hours to detect one melanoma and 16 hours to detect one keratinocyte carcinoma.
Evidence for Screening:
Given the high cost and time commitment for screening, we next need to examine whether these exams are beneficial for patients. In one study, patients with thinner melanomas had more skin cancer screenings compared to those with thicker melanoma.8 For instance, for those with a melanoma less than 0.75 mm thick, the reported prevalence of clinical skin exams was 39% compared to 23% for those with a melanoma 3.0 mm or thicker.8 But we cannot be sure whether a delay in diagnosis led to this increased melanoma thickness. Ultimately the question is, does TBSE impact morbidity and mortality from melanoma?
A systematic review of 15 studies, seven being well-designed population-based screening studies from Germany, showed that skin cancer screening increased the detection of melanoma in situ and thin melanoma, as well as keratinocyte carcinomas.9 Further, the study showed that after cessation of screening, invasive melanoma incidence decreased. However, melanoma mortality reduction was only shown in one study.9 In conclusion, there are potential benefits of TBSE, but there is no clear morality benefit.
Yet, we can identify populations where screening is valuable. In one of the referenced studies from Germany, the number needed to screen to detect one melanoma was stratified by age.10 When screening patients 35 years and older, the number needed to screen was 559. When the screening population was restricted to 65 years and older, this number dropped to 178.10
Further, a recent prospective, population-based, cohort study from Australia followed patients diagnosed with melanoma for 12 years.11 Of all the patients, 35% had their melanoma detected in a routine skin cancer screening. Compared to patient-detected melanomas, those with routine skin check-detected melanomas had 59% lower melanoma-specific mortality and 36% lower all-cause mortality. After adjusting for prognostic factors, the all-cause mortality remained significant, but the melanoma-specific mortality did not. Factors associated with higher odds of melanoma detection on routine screenings included being male, being older than 50 years, living in a “non-remote” area, having a previous melanoma, and having many moles. 11
An editorial based on the above article summarized Dr. Patel’s final points well – “the greatest benefit [of melanoma screening] will be derived in high-mortality populations, such as white men older than 50 years, those with a personal or family history of melanoma, and those with a high-risk phenotype (e.g., many moles, atypical moles, and/or severe sun damage).”12 Further, “recognize the potential harm from unnecessary biopsies and overdiagnosis, especially in low-mortality populations.”12
Conclusion:
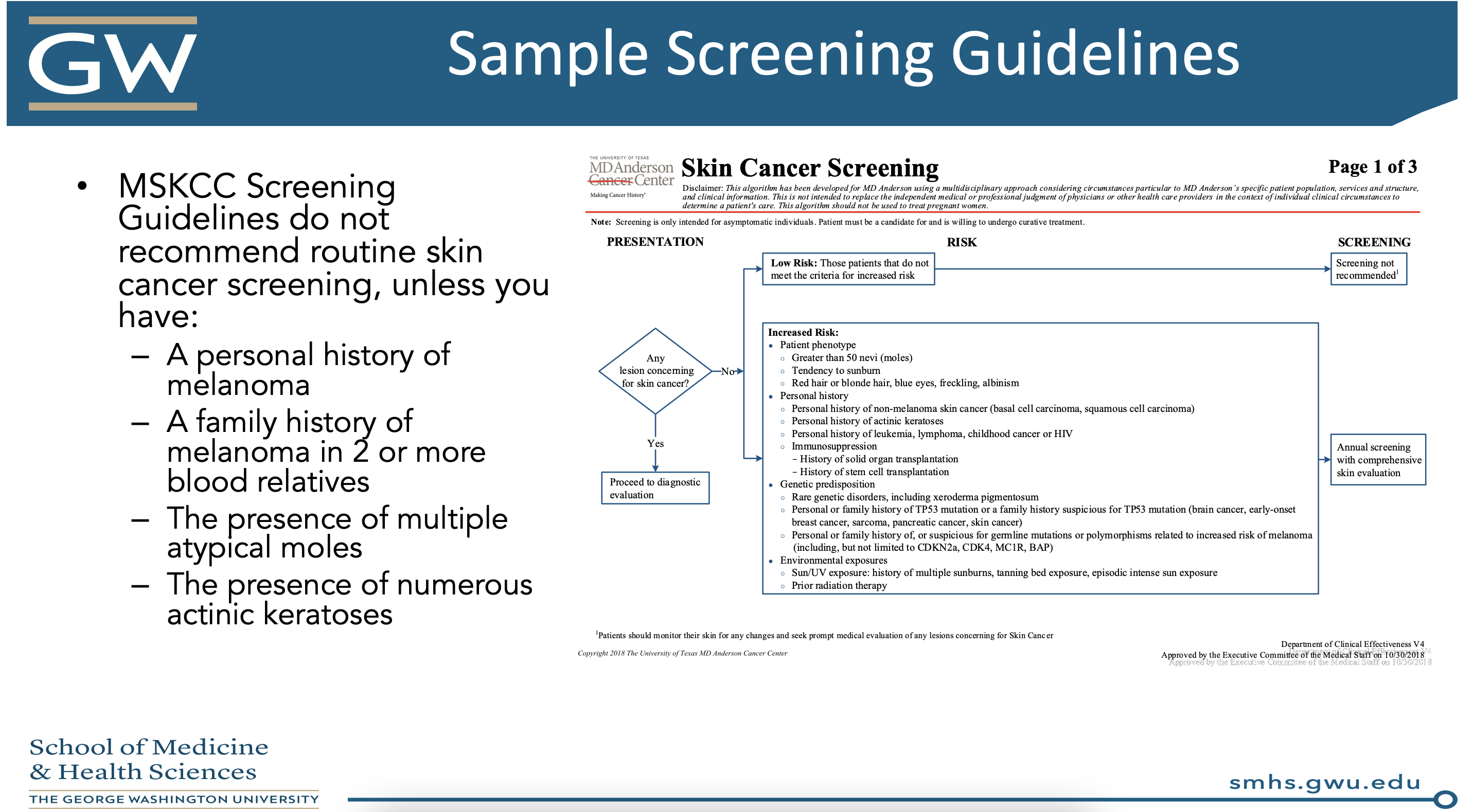
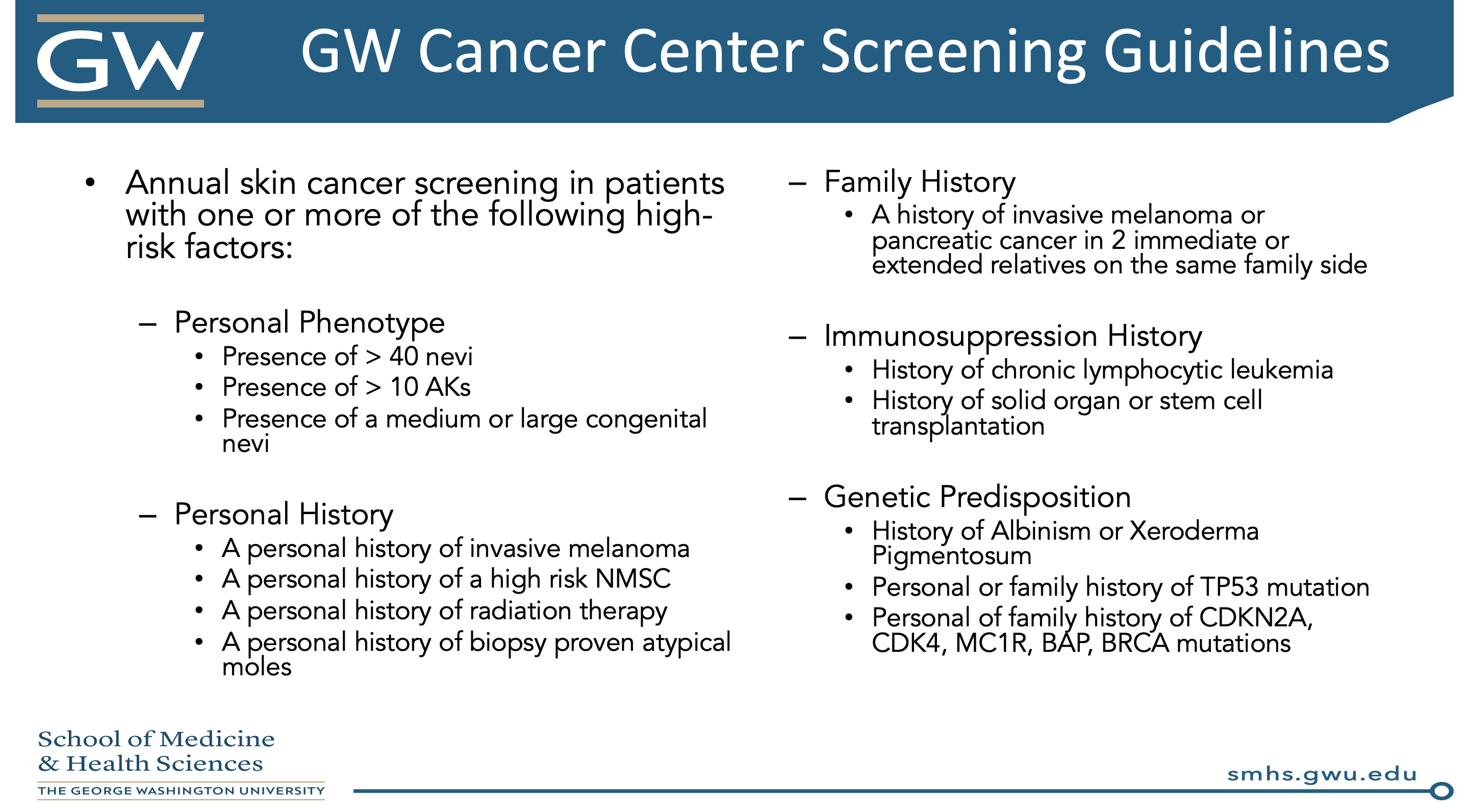
Dr. Patel summarized with a few salient points. First of all, artificial intelligence holds promise for increasing diagnostic accuracy – we need to be the stewards of how to apply this technology to TBSEs (and this will not replace us). We must move away from the phrase, “if you have any concern, biopsy it.” There are physical, psychological, and financial harms for patients in whom a biopsy over diagnoses melanoma. For these patients, consider active surveillance or topical therapy. In order to apply these lessons to your practice, you should develop a set of screening guidelines to follow. Here are two models from Dr. Patel’s presentation:
Given total body skin exams are an everyday practice for us, this lecture certainly provides food for thought about who we should be screening in our clinics and to how to apply these lessons to the entire American population. As future residents, we certainly will have a large role in shaping the future of skin cancer screening in this country!
References:
-
- Rogers HW, Weinstock MA, Feldman SR, Coldiron BM. Incidence Estimate of Nonmelanoma Skin Cancer (Keratinocyte Carcinomas) in the U.S. Population, 2012. JAMA Dermatol. 2015;151(10):1081-1086. doi:10.1001/jamadermatol.2015.1187
- Welch HG, Mazer BL, Adamson AS. The Rapid Rise in Cutaneous Melanoma Diagnoses. N Engl J Med. 2021;384(1):72-79. doi:10.1056/NEJMsb2019760
- Chen SC, Bravata DM, Weil E, Olkin I. A comparison of dermatologists’ and primary care physicians’ accuracy in diagnosing melanoma: a systematic review. Arch Dermatol. 2001;137(12):1627-1634. doi:10.1001/archderm.137.12.1627
- Fritschi L, Dye SA, Katris P. Validity of melanoma diagnosis in a community-based screening program. Am J Epidemiol. 2006;164(4):385-390. doi:10.1093/aje/kwj204
- Helm MF, Hallock KK, Bisbee E, Miller JJ. Optimizing the total-body skin exam: An observational cohort study. J Am Acad Dermatol. 2019;81(5):1115-1119. doi:10.1016/j.jaad.2019.02.028
- Dinnes J, Deeks JJ, Chuchu N, et al. Dermoscopy, with and without visual inspection, for diagnosing melanoma in adults. Cochrane Database Syst Rev. 2018;12:CD011902. doi:10.1002/14651858.CD011902.pub2
- Hartman RI, Xue Y, Singer S, Markossian TW, Joyce C, Mostaghimi A. Modelling the value of risk-stratified skin cancer screening of asymptomatic patients by dermatologists. Br J Dermatol. 2020;183(3):509-515. doi:10.1111/bjd.18816
- Aitken JF, Elwood M, Baade PD, Youl P, English D. Clinical whole-body skin examination reduces the incidence of thick melanomas. Int J Cancer. 2010;126(2):450-458. doi:10.1002/ijc.24747
- Brunssen A, Waldmann A, Eisemann N, Katalinic A. Impact of skin cancer screening and secondary prevention campaigns on skin cancer incidence and mortality: A systematic review. J Am Acad Dermatol. 2017;76(1):129-139.e10. doi:10.1016/j.jaad.2016.07.045
- Hübner J, Waldmann A, Eisemann N, et al. Association between risk factors and detection of cutaneous melanoma in the setting of a population-based skin cancer screening. Eur J Cancer Prev. 2018;27(6):563-569. doi:10.1097/CEJ.0000000000000392
- Watts CG, McLoughlin K, Goumas C, et al. Association Between Melanoma Detected During Routine Skin Checks and Mortality. JAMA Dermatol. 2021;157(12):1425-1436. doi:10.1001/jamadermatol.2021.3884
- Halpern AC, Marchetti MA. Melanoma Screening-Time for a Reset? JAMA Dermatol. 2021;157(12):1409-1411. doi:10.1001/jamadermatol.2021.3883
This information was presented by Dr. Vishal A. Patel at the 2022 ODAC Dermatology, Aesthetic and Surgical Conference held January 14-17, 2022. The above highlights from her lecture were written and compiled by Dr. Emily Murphy.
Did you enjoy this article? You can find more on Medical Dermatology here.

