ABSTRACT
INTRODUCTION
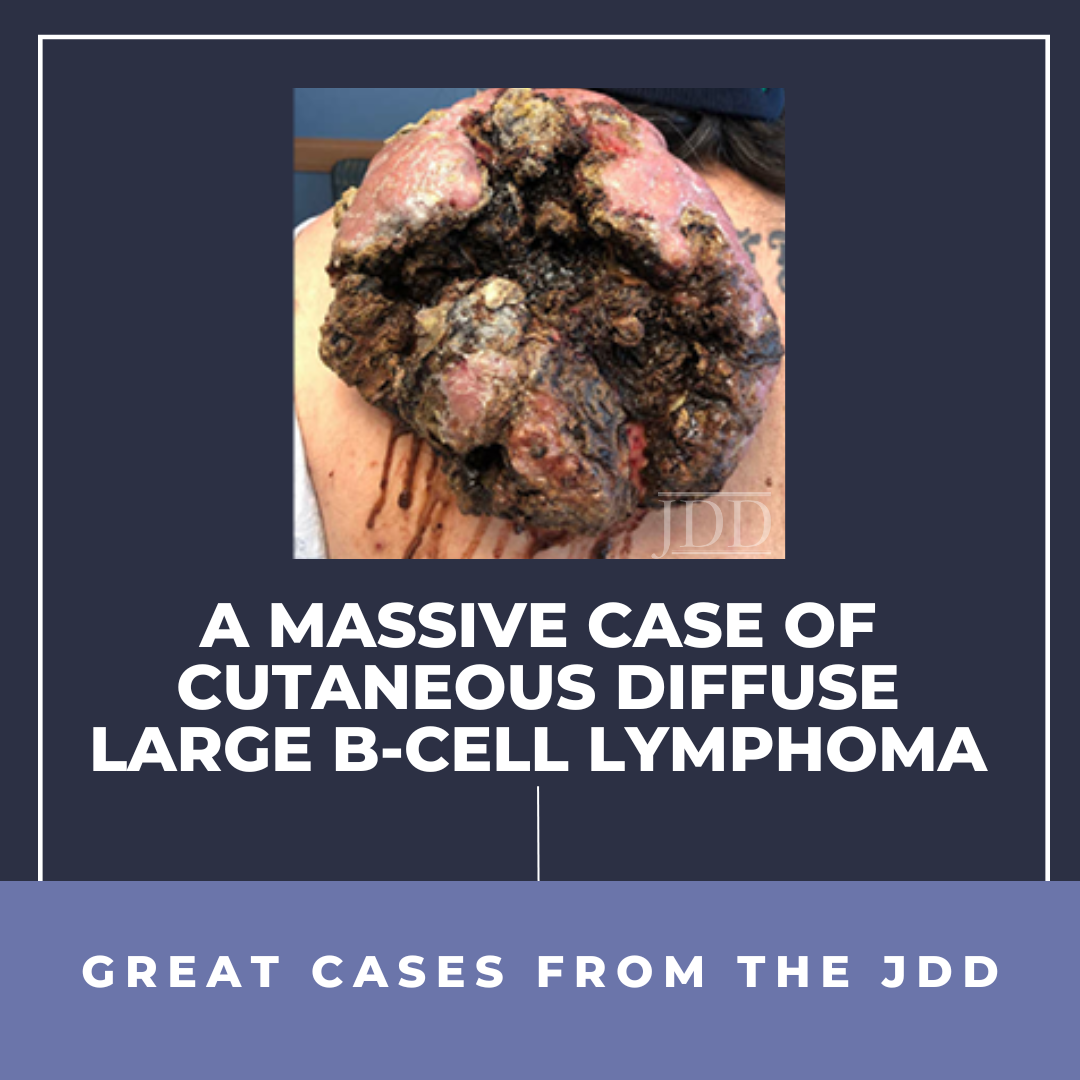
CASE REPORT

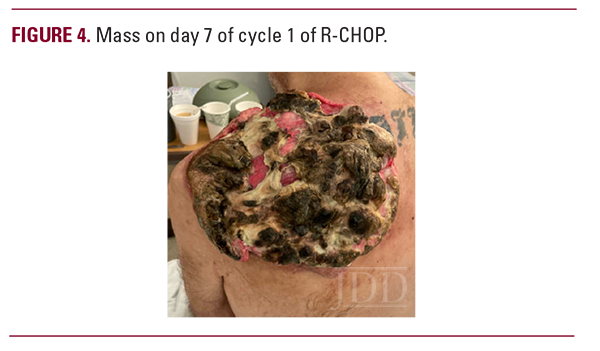
 Seven months later, he was admitted to the intensive care unit. The mass was necrotic, fungating, and infested with maggots (Figure 3). Computed tomography showed significant growth of the shoulder mass with worsening subcutaneous and muscular invasion of the left shoulder, re-demonstration of the supraclavicular and axillary lymphadenopathy, and new upper abdominal and retroperitoneal lymphadenopathy. His hemoglobin on admission was 2.9g/dL from chronic blood loss from the mass resulting in hemorrhagic shock. Surgery was consulted for de-bulking of the tumor and removal of the maggots, but the bleeding risk was felt to be too high. Two days after admission and stabilization with multiple packed red blood cell transfusions, he began R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone). The lesion on day 7 of cycle 1 of R-CHOP is shown in Figure 4. The wound and necrotic sloughing were successfully managed with saline wound wash and Kerlix dampened with Dakin solution. No debridement was required.
Seven months later, he was admitted to the intensive care unit. The mass was necrotic, fungating, and infested with maggots (Figure 3). Computed tomography showed significant growth of the shoulder mass with worsening subcutaneous and muscular invasion of the left shoulder, re-demonstration of the supraclavicular and axillary lymphadenopathy, and new upper abdominal and retroperitoneal lymphadenopathy. His hemoglobin on admission was 2.9g/dL from chronic blood loss from the mass resulting in hemorrhagic shock. Surgery was consulted for de-bulking of the tumor and removal of the maggots, but the bleeding risk was felt to be too high. Two days after admission and stabilization with multiple packed red blood cell transfusions, he began R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone). The lesion on day 7 of cycle 1 of R-CHOP is shown in Figure 4. The wound and necrotic sloughing were successfully managed with saline wound wash and Kerlix dampened with Dakin solution. No debridement was required.

 He has completed 6 cycles to date and is now in remission. The mass two months after cycle 6 is shown in Figure 5. He is currently undergoing evaluation for a skin graft to complete the wound healing.
He has completed 6 cycles to date and is now in remission. The mass two months after cycle 6 is shown in Figure 5. He is currently undergoing evaluation for a skin graft to complete the wound healing.
 DISCUSSION
DISCUSSION
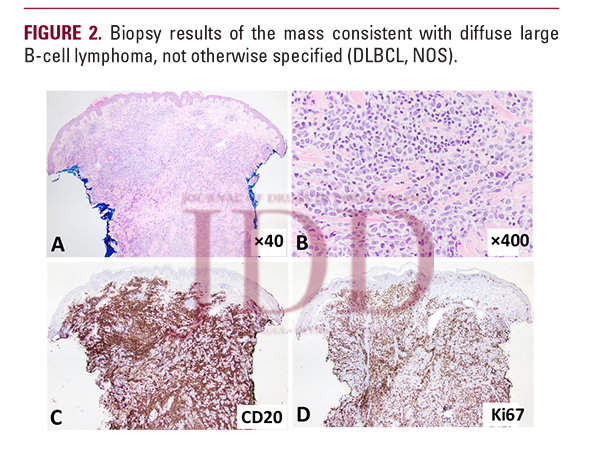
This patient’s presentation of a large cutaneous mass was initially concerning for primary cutaneous malignancy such as a baso-squamous carcinoma. However, biopsy was consistent with DLBCL and imaging revealed involvement of lymph nodes which is consistent with DLBCL, NOS rather than primary cutaneous diffuse large B-cell lymphoma (PCDLBCL) which does not typically have nodal involvement.3 Aggressive B cell lymphomas can manifest as exophytic skin lesions at first presentation and may mimic carcinoma or other solid tumors. The rapid growth of aggressive lymphoma underscores the need for urgent histologic diagnosis in these cases to guide treatment without delay. Additionally, extranodal involvement of DLBCL is rare and a poor prognostic factor.4 In fact, only 1.1% of patients with DLBCL have skin involvement and only 4.8% have soft tissue involvement.4
DLBCL is typically treated with R-CHOP.5 Surgery is not a typical management strategy in DLBCL but can be used for palliation. Conversely, surgical resection with wide margins is the treatment of choice for most cutaneous malignancies such as basal cell carcinoma or squamous cell carcinoma. This patient’s large cutaneous mass was exquisitely sensitive to chemotherapy alone, and the mass has resolved without any surgical intervention to date. With appropriate chemotherapeutics, even large, exophytic lymphomatous masses can be managed without surgical intervention. Given the potential bleeding complications and risks associated with surgery, this carries direct implications for the management of these patients. DLBCL can present as a large cutaneous mass that resolves with chemotherapy alone and does not require surgical excision or debridement.
DISCLOSURES
REFERENCES
-
- Boussios S, Zerdes I, Vassou A, et al. Extranodal diffuse large B-cell lymphomas: A retrospective case series and review of the literature. Hematol Rep. 2018;10(1):7070-7070.
- Kilaru S, Panda SS, Mishra S, et al. Cutaneous involvement in diffuse large B cell lymphoma at presentation: report of two rare cases and literature review. Journal of the Egyptian National Cancer Institute. 2021;33(1):25.
- Paulli M, Lucioni M, Maffi A, et al. Primary cutaneous diffuse large B-cell lymphoma (PCDLBCL), leg-type and other: an update on morphology and treatment. Giornale italiano di dermatologia e venereologia : organo ufficiale, Societa italiana di dermatologia e sifilografia. 2012;147(6):589-602.
- Takahashi H, Tomita N, Yokoyama M, et al. Prognostic impact of extranodal involvement in diffuse large B-cell lymphoma in the rituximab era. Cancer. 2012;118(17):4166-4172.
- Susanibar-Adaniya S, Barta SK. 2021 Update on Diffuse large B cell lymphoma: A review of current data and potential applications on risk stratification and management. American Journal of Hematology. 2021;96(5):617-629
SOURCE
Merz, L. E., Hergott, C. B., & Zon, R. (2023). A Massive Case of Cutaneous Diffuse Large B-Cell Lymphoma. Journal of drugs in dermatology: JDD, 22(12), 1223-1224.
Adapted from original article for length and style.