INTRODUCTION
Periocular basal cell carcinoma (BCC) is the most common eyelid malignancy concomitant with ocular morbidity and quality of life impact.1,2 Orbital invasion occurs in 2% of cases and poses challenges for management.1,3 JDD authors highlight a multidisciplinary approach to the treatment of advanced periocular BCC.
CASE
JDD authors discuss a 56-year-old male who presented for Mohs consultation with recurrent progressive BCC of the left lower forehead extending to the orbital rim. Fourteen years prior, the patient sustained a bike trauma to the left lateral forehead. Ten years later, he underwent a biopsy and surgical excision of a nodular and infiltrative BCC at the previous trauma site.
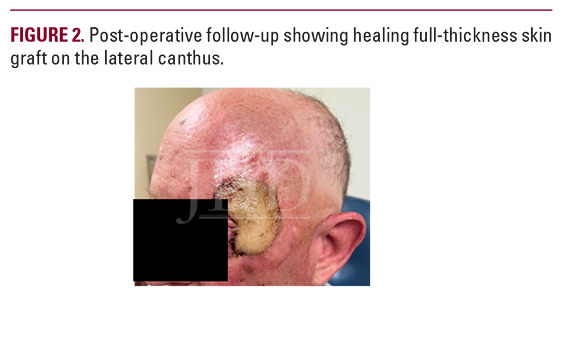
Eight years after surgery, he reported a new ulcerated nodule in the area adjacent to the excised site with involvement of the left temple and upper eyelid causing swelling and inability to fully close the eye (Figure 1A). Symptoms included left-sided blurred vision with disabling headaches. Clinical examination revealed an ulcerating plaque with pink rolled borders on the left forehead extending laterally to the left temple and upper eyelid, with associated eyelid edema and ptosis. Histopathology showed nodular and infiltrative BCC (Figure 2). CT-head with contrast showed an infiltrative soft tissue mass involving lateral aspects of the left periorbital soft tissue with possible involvement of the superior palpebris muscle. There was swelling of the left upper eyelid and a tumor near the globe without involvement of extraocular muscles. CT-chest, abdomen, and pelvis showed no evidence of distant metastasis.
Worsening blurred vision and headaches signified rapid tumor growth. Given the tumor’s effects and location, a multidisciplinary team including dermatologic surgery, ophthalmology, otolaryngology, and oncology was convened to discuss treatment options. Neoadjuvant treatment with vismodegib was initiated, as curative surgical excision at this time could result in eye exenteration and vision loss.4 Within 2 weeks of starting oral vismodegib 150 mg daily, the patient reported resolving cutaneous lesions and complete relief of headaches and blurred vision. Four months after vismodegib initiation, repeat CT-head revealed an interval decrease in the prominence of ill-defined multilobulated pre-septal soft tissue within the left-upper eyelid and periorbital regions, indicating treatment response.
Eight months after vismodegib initiation (Figure 1B), repeat CT-head and MRI of the orbit showed continued tumor resolution. At this time, tumor resection was performed by the dermatologic surgeon, and closure with right radial forearm free flap reconstruction was performed by the otolaryngologist (Figure 2).

 DISCUSSION
DISCUSSION
Locally-advanced periocular BCC is rare and a history of trauma comprises a small proportion of cases. Risk factors for orbital invasion include male sex, advanced age, medial canthal location, previous recurrence, large mass size, aggressive histologic subtype, and perineural invasion.1 Signs suggestive of orbital involvement include mass with bone fixation, impaired ocular mobility, and globe displacement.2 Upregulation and activation of the Hh-signaling pathway are also associated with BCC. A patched homolog (PTCH1) loss-of-function mutation or gain-in-function mutation of smoothened homolog (SMO) genes results in excessive signaling through the Hh-signaling pathway and malignant transformation of basal cells. Vismodegib is a small molecule inhibitor of SMO that blocks the Hh-signaling pathway and leads to tumor shrinkage. Due to its rapidity and high response rates, vismodegib remains suitable for preserving and improving visual function in periocular BCC. In Kahana et al’s study, patients with extensive periocular BCC were treated with vismodegib 150 mg daily and demonstrated investigator-assessed response rates of 60.3% and a median duration of response in 26.2 months.4 Importantly, physical examination and MRI/CT-scan complete responses were noted in 56% and 47% of patients, respectively.4
In conclusion, the authors’ case highlights a multidisciplinary treatment approach for advanced periocular BCC using neoadjuvant vismodegib and surgery without loss of the eye or severe disfigurement.
DISCLOSURES
The authors have no conflicts of interest or funding sources to declare.
REFERENCES
-
- Sun MT, Wu A, Figueira E, et al. Management of periorbital basal cell carcinoma with orbital invasion. Fut Oncol. 2015;11(22):3003-10. doi:10.2217/fon.15.190
- Leibovitch I, McNab A, Sullivan T, et al. Orbital invasion by periocular basal cell carcinoma. Ophthalmology. 2005;112(4):717-23. doi:10.1016/j. ophtha.2004.11.036
- Madge SN, Khine AA, Thaller VT, et al. Globe-sparing surgery for medial canthal basal cell carcinoma with anterior orbital invasion. Ophthalmology. 2010;117(11):2222-8. doi:10.1016/j.ophtha.2010.02.013
- Kahana A, Unsworth SP, Andrews CA, et al. Vismodegib for preservation of visual function in patients with advanced periocular basal cell carcinoma: The VISORB trial. Oncologist. 2021;26(7):e1240-e1249. doi: 10.1002/onco.13820
SOURCE
Aguwa, Chibuzo J., et al. “Multidisciplinary Approach to Treatment of Advanced Basal Cell Carcinoma With Involvement of the Left Orbit.” Journal of Drugs in Dermatology: JDD 23.6 (2024): e142-e143.
Content and images published with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
Did you enjoy this JDD Case Report? You can find more here.

