Authors Julie K. Nguyen MD, Silvia Mancebo MD, Brady Bleicher MD, and Jared Jagdeo MD MS present a case report of a patient with localized porokeratosis lesions on the face and extremities. Brought to you by the Journal of Drugs in Dermatology, a product of SanovaWorks.
Introduction
Porokeratosis is a disorder of epidermal keratinization that encompasses multiple clinical variants based on different patterns of distribution. It classically manifests as one or more erythematous, annular plaques with an atrophic center and hyperkeratotic ridge-like border.1-3 The primary lesion of classic porokeratosis starts as a small, light brown, scaly papule that spreads in a centrifugal manner and may slowly progress and coalesce into a sharply circumscribed plaque of various sizes and forms.4,5 The lesions are often asymptomatic but may be associated with pruritus.1
Porokeratosis lesions may affect any part of the body, including palmoplantar surfaces and mucous membranes, but are more prevalent on the trunk and extremities.1,2Porokeratosis may be classified as classic porokeratosis of Mibelli, linear porokeratosis, disseminated porokeratosis, disseminated superficial actinic porokeratosis, punctuate porokeratosis, or porokeratosis palmaris et plantaris disseminata.1,3 The histopathological hallmark of porokeratosis is the cornoid lamella, characterized by a thin column of parakeratotic corneocytes embedded within the stratum corneum, forming an indentation within the epidermis.1,3,4 While the exact pathogenesis of porokeratosis remains unclear, it may be acquired or hereditary, and is thought to be due to the clonal expansion of abnormal epidermal keratinocytes.1,4 The proliferation of abnormal clones may be triggered by extrinsic factors such as irradiation, infective agents, mechanical trauma, and immunosuppression.1 The differential diagnosis of porokeratosis includes actinic keratosis, seborrheic keratosis, psoriasis, lichen planus, Bowen’s disease, and squamous cell carcinoma.2,4
The overall prognosis of porokeratosis is favorable. However, a potential complication is an increased risk (estimated to be less than 10%) of malignant transformation of a porokeratosis lesion to a basal or squamous cell carcinoma.1,6 Risk factors include large lesion size, localization on the extremities, older age, and a long period of existence.1
There is no definitive or “gold standard” treatment regimen for porokeratosis, and current therapeutic approaches have variable efficacy and durability. Asymptomatic lesions are often managed conservatively with sun protection, emollients, and clinical surveillance for signs of malignant degeneration.1 Current therapeutic modalities used to improve the signs and symptoms of porokeratosis include many topical, systemic, and surgical treatment options such as: 5-fluorouracil cream, topical vitamin D3 analogs, topical and systemic retinoids (eg, acitretin or isotretinoin), cryotherapy, dermabrasion, laser ablation, imiquimod, ingenol mebutate, topical diclofenac, cantharidin, corticosteroids, topical tacrolimus, phototherapy, and surgical excision.3,4 A systematic review found that no randomized controlled trials have been conducted to assess treatments evifor porokeratosis.3 Based on a limited number of case reports and cases series available in the literature, porokeratosis of Mibelli shows the best clinical outcomes after treatment with imiquimod cream.3
Herein, we report a case of a patient who had multiple lesions consistent with porokeratosis of Mibelli that were each successfully treated with a combination of ablative fractional carbon dioxide (CO2) laser and topical application of an antioxidant serum.
Case Report
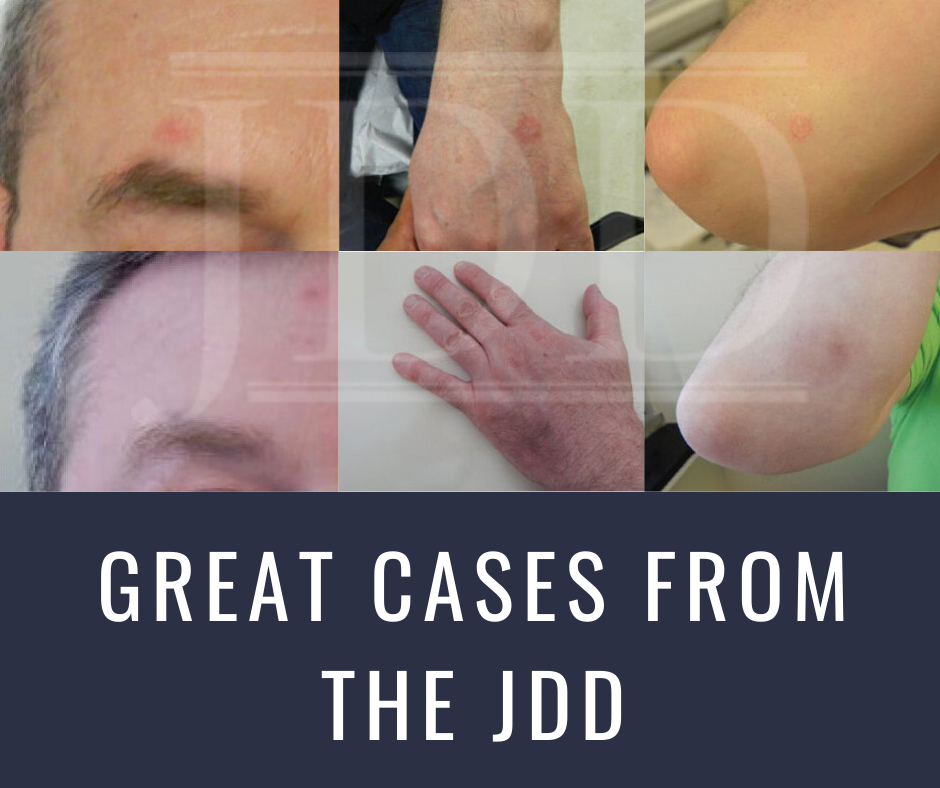
A 51-year-old male with Fitzpatrick skin phototype 2 presented to dermatology clinic for evaluation of a chronic rash. He reported the occurrence of focal, red, scaly lesions on his left hand, face, and right arm. The onset of these lesions was unclear, but they remained unchanged despite the use of topical clobetasol. His past medical history included celiac disease and hyperlipidemia, and medications included gemfibrozil. Physical examination revealed three annular, pink, erythematous plaques (approximately 1.0 x 1.0 cm) with a raised scaly border distributed on the left dorsal hand, right forehead superior to the eyebrow, and right dorsal forearm (Figure 1A-C).
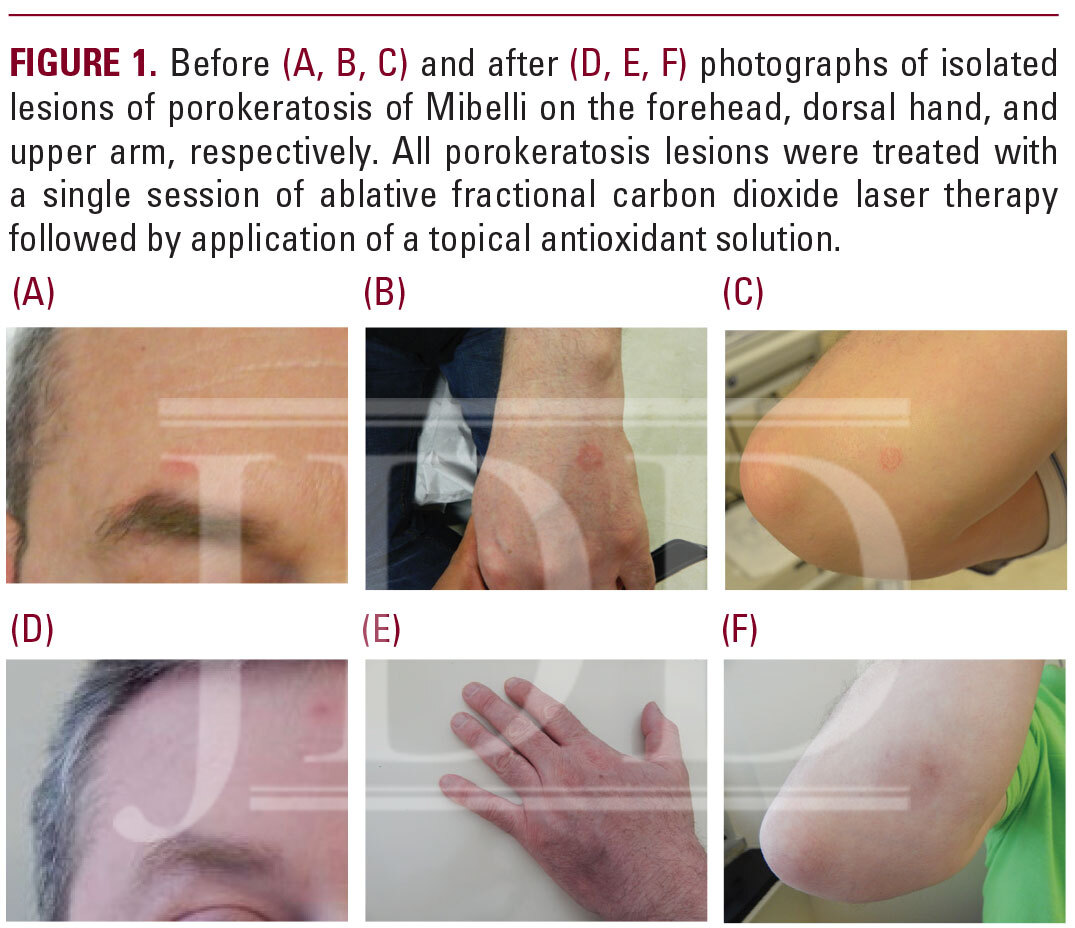
The lesion on the forearm was visualized under dermoscopy, optical coherence tomography (OCT), and reflectance confocal microscopy (RCM). Dermoscopy revealed the presence of a peripheral white rim and multiple dotted vessels over an erythematous center and superficial white scales (Figure 2A). OCT (VivoSight, Michelson Diagnostics Ltd, Kent, UK) showed a cornoid lamella (Figure 2B). RCM (VivaScope 3000, Caliber I.D., Rochester, NY) showed an atypical honeycomb pattern and architectural disarray at the corneal level (Figure 2C). Based on the clinical presentation and morphologic features identified on in vivo skin imaging modalities, the diagnosis of porokeratosis of Mibelli was made. A skin biopsy was deferred. Although the lesions were asymptomatic, the patient was concerned about the aesthetic appearance and requested treatment.
The individual lesions were treated with ablative fractional CO2 laser resurfacing (Fraxel Repair, Solta Medical, Hayward, CA). Two days prior to the procedure, he was started on prophylaxis with valacyclovir (1 g twice daily for 7 days) and cephalexin (500 mg four times daily for 14 days). For each focal site of porokeratosis, the lesion received three passes of the laser at 70 mJ with 35% coverage. An additional pass was performed at 50 mJ with 30% coverage along with feathering at the edges. A topical formulation of 15% L-ascorbic acid, 1% alpha-tocopherol, and 0.5% ferulic acid serum (C E Ferulic, SkinCeuticals Inc, Garland, TX) was applied immediately after the procedure, and the patient was instructed to re-apply it twice daily for two days. At a two months follow-up visit, clinical examination of the affected areas showed complete clearance of the lesions (Figure 1D-F), and repeat in vivo imaging of the lesion on the forearm showed normal skin (images not shown).
Discussion
There is a paucity of clinical studies evaluating therapeutic modalities for porokeratosis. The use of CO2 laser ablation for the treatment of porokeratosis has been previously documented in isolated case reports.3 Successful treatment of porokeratosis of Mibelli with the CO2 laser has been reported with good clinical and aesthetic outcomes, including histological confirmation of complete resolution of porokeratosis features and no evidence of recurrence at follow-up.7,8 CO2 laser treatment has also been used successfully in other types of porokeratosis, including linear porokeratosis.9,10 Besides the CO2 laser, the 585 nm pulsed-dye laser and Nd:YAG laser have been reported to be effective for various forms of porokeratosis.1
The use of ablative fractional CO2 laser for the treatment of porokeratosis of Mibelli has several advantages compared to other therapeutic options such as systemic agents or surgical excision, as it is minimally invasive, can be used to treat areas of extensive involvement, and lacks significant side effects. Furthermore, a single treatment session may be sufficient to achieve complete clearance and the potential for post-laser scarring can be minimized as the laser parameters can be customized.7 Postoperative application of vitamin C, E, and ferulic acid serum has been shown to promote more rapid wound healing after fractional ablative laser treatment.11
This case report highlights the clinical utility of using real-time, high-resolution, non-invasive imaging techniques to establish a diagnosis of porokeratosis. In this case, by using OCT to identify the cornoid lamella and using RCM to examine the distinct morphologic features of porokeratosis, we were able to confirm a diagnosis of porokeratosis, avoiding the need for an invasive biopsy for histopathological examination. The hallmark of dermoscopy diagnosis of porokeratosis is the presence of a peripheral white rim, corresponding to the cornoid lamella, which can also be identified on OCT.1,5 On RCM imaging of porokeratosis, the presence of sharp demarcation and hyper-refractile border at the level of the corneal layer corresponds in histopathology to the presence of the cornoid lamella.5
In conclusion, the use of the CO2 laser in porokeratosis of Mibelli is a therapeutic modality that is minimally invasive, offers fast and durable results, delivers clinical results, and is associated with patient satisfaction. Clinicians should consider the use of ablative fractional CO2 laser to treat focal porokeratosis lesions with consideration of the size of the lesion, anatomical location, and risk of malignant transformation. To date, there are no treatment guidelines or universal consensus on the optimal treatment for porokeratosis, with the therapeutic armamentarium consisting of a variety of topical agents, systemic medications, and surgical modalities. The approach to treatment for porokeratosis should be individualized with consideration of the functional and aesthetic impact and patient preferences.
References
- Sertznig P, Von Felbert V, Megahed M. Porokeratosis: present concepts. J Eur Acad Dermatology Venereol. 2012;26(4):404-412.
- Ferreira FR, Santos LDN, Tagliarini FANM, Lira ML de A. Porokeratosis of Mibelli–literature review and a case report. An Bras Dermatol. 2017;88(6 Suppl 1):179-182.
- Weidner T, Illing T, Miguel D, Elsner P. Treatment of porokeratosis: a systematic review. Am J Clin Dermatol. 2017;18(4):435-449.
- Kanitakis J. Porokeratoses: An update of clinical, aetiopathogenic and therapeutic features. Eur J Dermatology. 2014;24(5):533-544.
- González S, ed. Reflectance Confocal Microscopy of Cutaneous Tumors. 2nd ed. Boca Raton, FL: CRC Press; 2017.
- Sasson M, Krain AD. Porokeratosis and cutaneous malignancy: A review. Dermatologic Surg. 1996;22(4):339-342.
- Groot DW, Johnston PA. Carbon dioxide laser treatment of porokeratosis of mibelli. Lasers Surg Med. 1985;5(6):603-606.
- Rabbin P, Baldwin H. Treatment of Porokeratosis of Mibelli with CO2 laser vaporization versus surgical excision with split-thickness skin graft. J Dermatol Surg Oncol. 1993;19(3):199-202.
- Hunziker T, Bayard W. Carbon dioxide laser in the treatment of porokeratosis. J Am Acad Dermatol. 1987;16(3 Pt 1):625.
- Barnett JH. Linear porokeratosis: Treatment with the carbon dioxide laser. J Am Acad Dermatol. 1986;14(5):902-904.
- Waibel JS, Mi QS, Ozog D, et al. Laser-assisted delivery of vitamin c, vitamin e, and ferulic acid formula serum decreases fractional laser postoperative recovery by increased beta fibroblast growth factor expression. Lasers Surg Med. 2016;48(3):238-244.
Source:
J. K. Nguyen MD, S. Mancebo MD, B. Bleicher MD, J. Jagdeo MD MS (2019). Successful Treatment of Porokeratosis With Ablative Fractional Carbon Dioxide Laser and Vitamin C, E, and Ferulic Acid Serum. Journal of Drugs in Dermatology, 18(11), 1174-1176. https://jddonline.com/articles/dermatology/S1545961619P0940X/1/
Content and images used with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
Did you enjoy this case report? Find more here.