Introduction



The standard treatment for HHD commonly includes antibiotics, such as tetracyclines, to combat the risk of superinfection by Staphylococcus aureus within disease lesions. However, prolonged antibiotic use can contribute to resistance, which exacerbates refractory HHD cases. Ruxolitinib may prevent or minimize recurrence of lesions that allow bacterial colonization.
Ruxolitinib, a topical JAK inhibitor, targets the JAK-1 and JAK- 2 enzymes and downregulates the Th2 inflammatory response by preventing cytokine signaling involving interleukin (IL)-4, IL-13, and IL-31.2 Additionally, topical ruxolitinib inhibits JAKdependent IFN, IL-6, IL-2 and epidermal growth factor receptor signaling, and enhances gene expression linked to wound healing and tissue homeostasis.3 ATP2C1, the gene mutated in HHD, is downregulated by IL-6 in keratinocytes.4 Therefore, inhibition of IL-6 may promote ATP2C1 expression within cells with functional gene copies.
Though approved for mild to moderate eczema and nonsegmental vitiligo, ruxolitinib has not yet been indicated for HHD. Case reports have demonstrated successful management of HHD with oral JAK inhibitors such as upadacitinib and tofacitinib, and dupilumab, a humanized monoclonal antibody.5-8 A separate report discussed dupilumab used in conjunction with topical ruxolitinib.9 However, while one letter to the editor has previously described successful use of only topical ruxolitinib for the treatment of HHD, this is, to our knowledge, the first comprehensive patient presentation of such occurrence.10
Other treatment modalities considered for refractory HHD include laser ablation and radiation therapy. CO2 laser, Er:YAG laser, and Grenz ray therapy are relatively safe and potentially effective options.11-13 However, in the case of our patient, Grenz ray laser eventually became ineffective. Therefore, it must be noted that the efficacy of therapies is heavily patient-dependent.
Oral monoclonal antibodies and certain JAK inhibitors, such as upadacitinib, may lead to a broader possibility of adverse effects due to systemic absorption. Reported effects include headache, nausea, and upper respiratory tract infections (URIs). However, topical ruxolitinib has less reported frequency of nasopharyngitis and URIs due to relatively low bioavailability.14
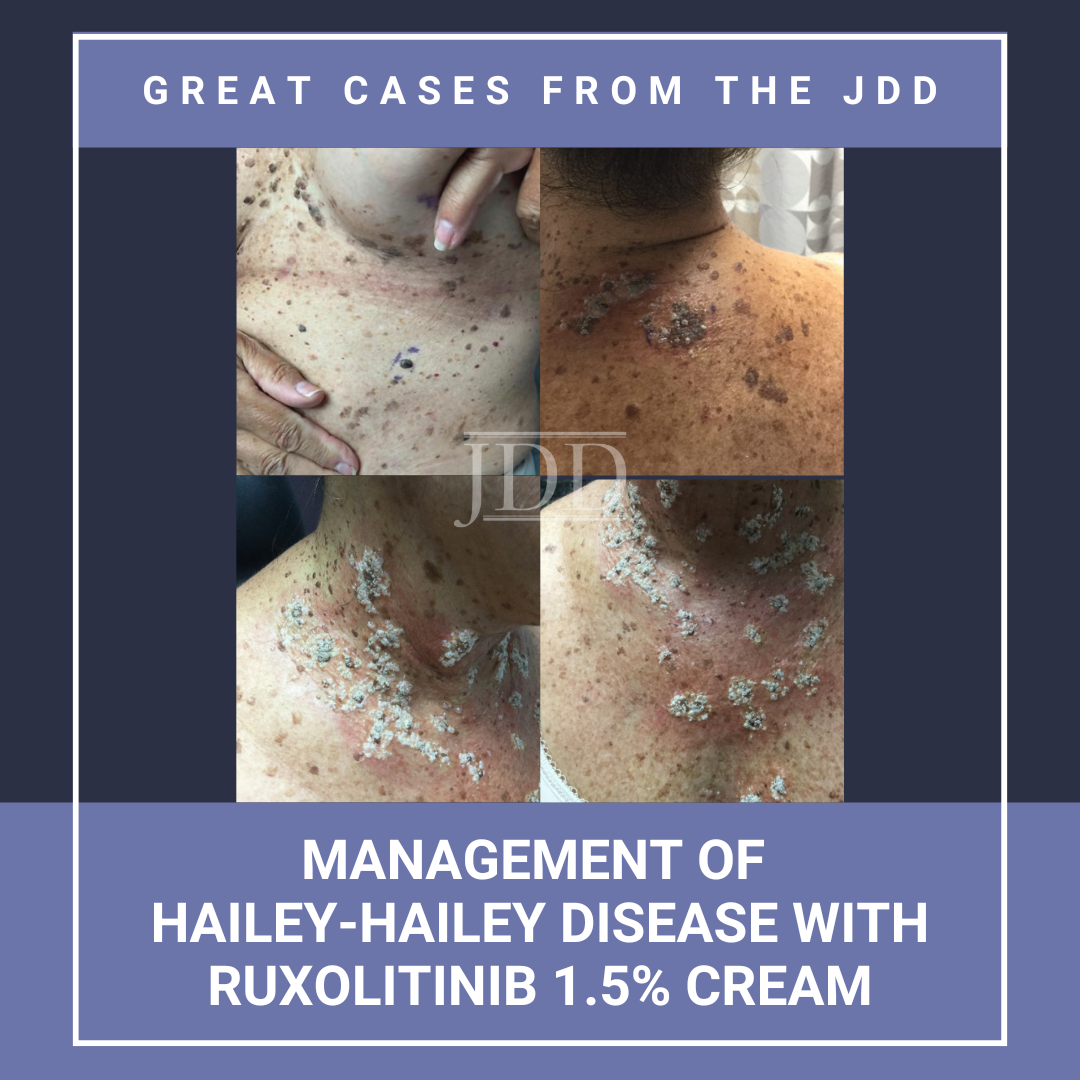
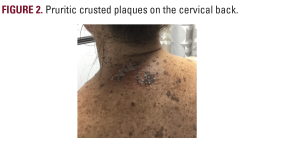
HHD presents with painful fissures within plaques that commonly occur in flexural areas, prone to friction, heat, and sweating that exacerbate the presence of lesions and cause irritation. Therefore, patients with HHD may be limited in physical activity due to pain or avoidance of exacerbation, leading to suboptimal quality of life. Overall, patients with dermatological conditions tend to have lower levels of happiness and increased risk for depression.15 A review of the German national registry revealed that 39.77% of HHD patients view their lives as severely or very severely affected and report overall mediocre satisfaction with life. Additionally, 84.1% of patients with HHD desired pain relief, 76.1% desired a normal daily life, and 67.1% desired engaging in normal leisure activities.16 Overall, the consequences of HHD extend beyond discomfort caused by physical symptoms–patients face a challenge in completing daily activities and responsibilities. Also, psychological impact based on the cosmetic appearance of the skin affects patients’ clothing choices and consciousness of physical appearance.
Conclusion
HHD is a chronic condition that can be detrimental to quality of life, especially in cases refractory to standard treatment. Topical JAK inhibitors have been a treatment of interest for such cases. The localized anti-inflammatory effects of these medications, such as ruxolitinib 1.5% cream, may provide an effective, alternative option for patients to effectively treat the disease. As HHD is an incurable, relapsing/remitting condition in which treatment response may be heavily patient-dependent, there is a need for further studies to explore the potential of including novel, effective therapies into the standard of care.
-
- Waldman RA, Grant-Kels JM. Groin and inframammary dermatitis. Dermatology for the Primary Care Provider. Elsevier. 2021:119-133.
- Hoy SM. Ruxolitinib Cream 1.5%: A review in mild to moderate atopic dermatitis. Am J Clin Dermatol. 2022;24(1):143-151.
- Schell SL , Sennett ML , Feehan RP, et al. Pilot study of topical ruxolitinib demonstrates efficacy and blunting of heterogeneous inflammatory processes in mild hidradenitis suppurativa. Br J Dermatol. 2025;192(5):845- 856.
- Yamamoto T, Aoyama Y. Role of pro-inflammatory cytokines in the pathophysiology of herpes simplex virus superinfection in Darier’s disease. J Dermatol. 2021;48(10):1607-1611.
- Murphy L, Ch’en P, Song EJ. Refractory Hailey–Hailey disease cleared with upadacitinib. JAAD Case Rep. 2023;41:64-67.
- Bao H, Yu K, An F, et al. Tofacitinib as a promising treatment for refractory erythroderma-like Hailey–Hailey disease. J Dermatol Treat. 2025;36(1).
- Kichena S, Carnicle J, Haseltine M. Improvement of Hailey-Hailey Disease following administration of dupilumab. J Drugs Dermatol. 2025;24(4):410- 412.
- Sulich-Moore C, Altman D, Gildenberg S. Treatment of recalcitrant Hailey- Hailey Disease with dupilumab: a case report. J Clin Aesthet Dermatol. 2025;18(4):18-20.
- Khang J, Yardman-Frank JM, Chen L, et al. Recalcitrant Hailey-Hailey Disease successfully treated with topical ruxolitinib cream and dupilumab. JAAD Case Rep. 2023;42:56-58.
- Ly S, Beylot-Barry M, Seneschal J. Refractory anogenital Hailey-Hailey. Disease successfully treated with topical ruxolitinib [Letter]. J Eur Acad Dermatol Venereol. 2025; 39(9):e786-e787.
- Farahnik B, Blattner CM, Mortazie MB, et al. Interventional treatments for Hailey-Hailey Disease. J Am Acad Dermatol. 2017;76(3):551-558.
- Debeuf MEPH, Knoops K, López-Iglesias C, et al. Long-term remission of Hailey-Hailey Disease by Er:YAG ablative laser therapy. J Eur Acad Dermatol Venereol. 2025;39(5):1038-1045.
- Larney C, Jobson D, Webster M. Grenz Ray Therapy for Darier Disease and Hailey-Hailey Disease: a case series of three patients [Letter]. Australas J Dermatol. 2025;66(1):e28-e31.
- Samuel C, Cornman H, Kambala A, et al. A review on the safety of using JAK inhibitors in dermatology: clinical and laboratory monitoring. Dermatol Ther. 2023;13(3):729-749.
- Schuster B, Ziehfreund S, Albrecht H, et al. Happiness in dermatology: a holistic evaluation of the mental burden of skin diseases. J Eur Acad Dermatol Venereol. 2019;34(6):1331-1339.
- Rogner D, Heimerl L, Heyer S, et al. Patients’ perspective, quality of life, and treatment goals in Hailey-Hailey Disease: lessons learned from the German National Registry. J Eur Acad Dermatol Venereol. 2024;38(2):419-429.
Source
Mendez, Hannah, Mounika Vattigunta, and Jacob Beer. “Management of Hailey-Hailey Disease With Ruxolitinib 1.5% Cream.” Journal of drugs in dermatology: JDD 24.11 (2025): 1141-1143.
Content and images used with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
Did you enjoy this JDD case report? You can find more here.