Verrucous psoriasis (VP) is a rare histologic variant of psoriasis. To date, fewer than 40 cases have been reported, with pediatric cases representing an exceedingly small fraction. Treatment options are limited, and the disease is often refractory to conventional methods. Herein, JDD authors Samantha Sherkin OMS-IV, Christian Summa OMS-IV, David Crasto DO, Zackary Whitney DO, Lazlo Karai MD PhD, and Stanley Skopit DO, MSE FAICD FAAD report a case of VP in an adolescent male which previously failed biologic and systemic therapy with adalimumab and acitretin, respectively, ultimately responding with great success to ixekizumab in combination with topical corticosteroids.
INTRODUCTION
Psoriasis is a multisystem, chronic inflammatory disease identified by a variety of presentations and clinical features that manifest primarily on the skin, as well as in the joints and appendages. In its most common presentation, the skin is affected by scaling erythematous plaques. Several subtypes of psoriasis exist, including plaque psoriasis, psoriatic arthritis, and guttate psoriasis, among others. Verrucous psoriasis (VP) is a particularly rare variant of the disease, with less than 40 cases reported along with an atypical presentation and, as a result, it can prove to be difficult both in diagnosis and treatment.1
VP is characterized clinically by verrucous erythematous plaques that most commonly present along the trunk and extremities.2 VP occurs more frequently in males, with a ratio of 1.6 and a mean age of 53 years old at presentation.3 Although the etiology remains unclear, associations with lymphatic obstruction, microangiopathy, diabetes, and obesity have been proposed.3 Other theories suspect that it is associated with repeated trauma to the skin in individuals with a pre-existing diagnosis of psoriasis.3-4
VP is often resistant to therapy and its response may be multifactorial, with variable response to treatments. Treatment options are limited and based on anecdotal case reports which include topical and systemic agents.4 Our case is unique because this involves presentation of VP in an adolescent male involving over 50% of the body surface area responding in a robust fashion to biologic therapy with ixekizumab.
CASE REPORT
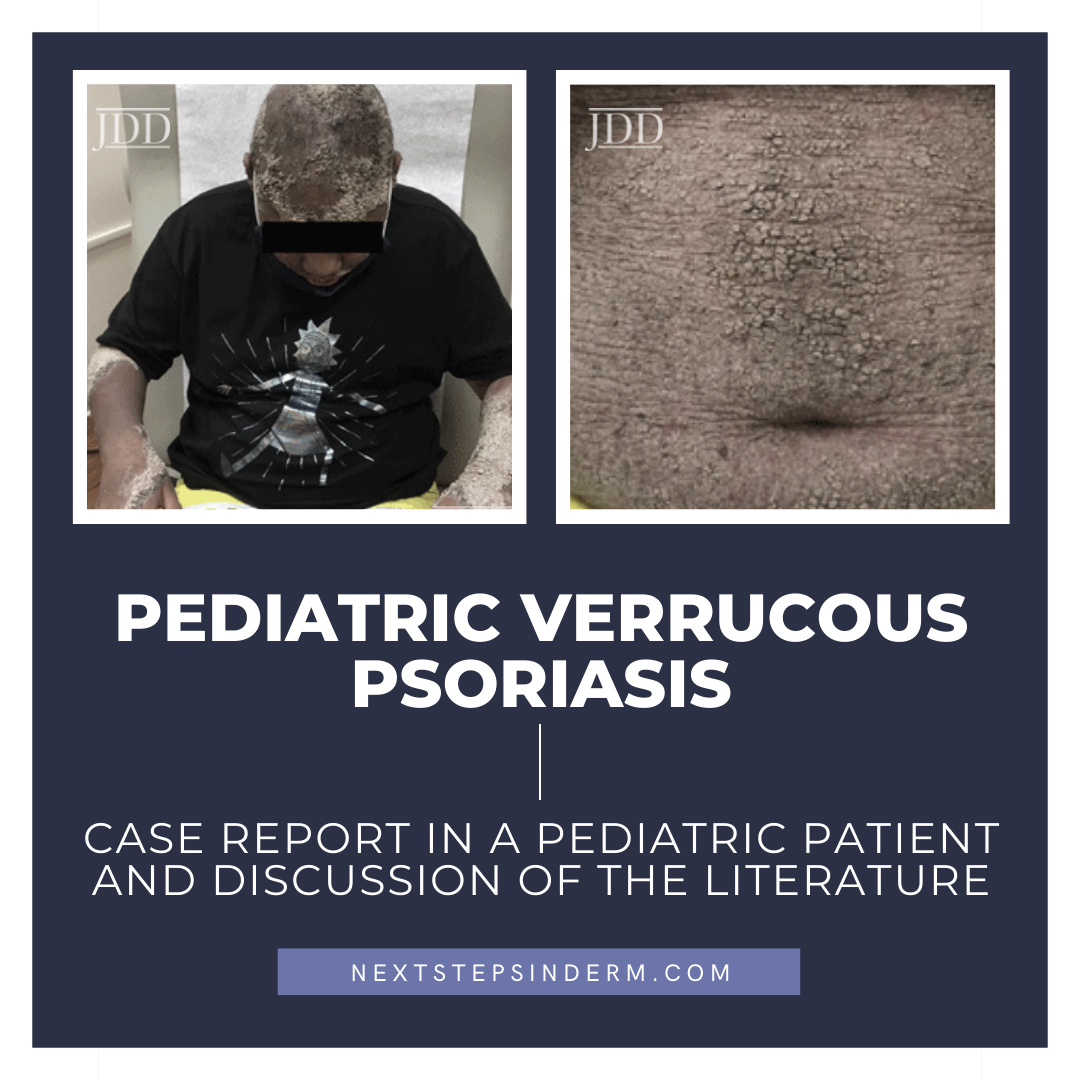
A 14-year-old African American male with comorbid obesity presented to the dermatology clinic with a 6-year history of skin lesions and associated alopecia causing a debilitating psychosocial impairment. He was previously diagnosed with ichthyosis vulgaris and treated with systemic and biologic therapy with adalimumab and acitretin, respectively, which provided minimal relief and he was lost to follow-up thereafter. Five years later, and without treatment during this time, he presented with coalescent linear verruciform plaques extending across >50% of his body surface area (BSA) with a predominance on extensor surfaces (Figures 1,2).


DISCUSSION
Psoriasis is a complex cell-mediated immunologic disease. Its various forms, including plaque, guttate, inverse, pustular, and erythrodermic, are all examples of the ways in which psoriasis can present, with VP now accepted as an infrequent clinical variant. VP is classically characterized by its unique histological features and manifests as symmetric hypertrophic verrucous plaques, most commonly involving the legs, arms, trunk, and dorsal aspect of the hands.5 Characteristic histologic features of VP include psoriasiform epidermal hyperplasia, papillomatosis, parakeratosis, and dilated vessels in the papillae.6 Additionally, bowing and elongation of the rete ridges with thickening and thinning of the suprapapillary epidermal plates may be seen, as well as Munro microabscesses, which are common in psoriasis but are absent in up to 35% of VP cases.7 Such as in our case, histopathological findings revealed psoriasiform acanthosis with intense parakeratosis and verrucous epidermal hyperkeratosis. Interestingly, features of follicular psoriasis were present as well.
VP should be suspected in a patient with history of plaque psoriasis and new development of hyperkeratotic, papillomatous plaques, with no koilocytic changes and no evidence of infection.3,7 While the etiology remains unclear, due to the limited number of cases, there are some theories which suggest that lymphatic obstruction, microangiopathy, diabetes, and obesity may play a role in the development of VP.2-7 Additionally, some postulate that the development of verrucous lesions may be secondary to keupnerization.2,4-6
There are several common histological features of VP, with most reports to date demonstrating papillomatous epidermal hyperplasia with broad parakeratosis on punch biopsy. However, the circumstances upon which the diagnosis is made vary from case to case. One can presume that this is due to the lack of information surrounding VP, leading to other, more common diagnoses being considered. An example of this is reported in a case of an 81-year-old man with a history of mild plaque psoriasis evaluated for an enlarging lesion on the foot. A diagnosis of verrucous carcinoma was made and the lesion was subsequently excised. However, a few months following excision, more verrucous plaques arose across the lower legs, forearms, and feet, and biopsy determined this to be VP, with the excised lesion believed to be the first manifestation of this disease.7 Other cases of VP arise in patients with weakened immune responses, such as in the case of a 44-year-old white male who developed VP while receiving IFN treatment for chronic Hepatitis C.8
Though only a few cases of VP have been reported thus far, many similarities, as well as differences, exist between those reported and our case. Two overarching differences between our own and others’ cases are the age of the patient at presentation and the diffuse spread of the verrucous plaques. Currently, only 1 other case involving a pediatric patient has been documented in a 14-year-old female with disease limited to her scalp and treated successfully with topical agents.4 Additionally, many cases report relatively localized lesions, whereas our patient had lesions over 50% of his body surface.
CONCLUSION
DISCLOSURES
ACKNOWLEDGMENTS
REFERENCES
2. Kawtar I, Mariame M, Siham L, et al. Verrucous psoriasis and verrucous lichen associated with an autoimmune hepatitis. J Clin Diag Res. 2014;2(1);107. doi: 10.4172/2376-0311.1000107.
3. Ben Rejeb S, Dhaoui A, Ben Ghachem D, et al. Psoriasis with verrucous appearance: A case report. Our Dermatol Online. 2017;8(1):63-65.
4. Moesch J, Mercer J, Sissom J, Weiss J. A rare case of verrucous psoriasis in young female: A case report and review of clinicohistologic presentation and variable therapeutic response. J Am Osteopath Coll Dermatol. 2016;34:56- 58.
5. Shivers L, Montanez-Wiscovich, ME. Verrucous psoriasis treated with methotrexate and acitretin combination therapy. Cutis. 2019;104(6):E10-E12.
6. Curtis AR, Yosipovitch G. Erythrodermic verrucous psoriasis. J Dermatolog Treat. 2012;23(3):215-218.
7. Garvie K, McGinley Simpson M, Logemann N, Lackey J. Verrucous psoriasis: a rare variant of psoriasis masquerading as verrucous carcinoma. JAAD Case Rep. 2019;5(8):723-725.
8. Scavo S, Gurrera A, Mazzaglia C, et al. Verrucous psoriasis in a patient with chronic C hepatitis treated with interferon. Clin Drug Investig. 2004;24(7):427- 429.
9. Monroe HR, Hillman JD, Chiu MW. A case of verrucous psoriasis. Dermatol Online J. 2011;17(5):10.
10. Ghoneim S, Ramos-Rodriguez AJ, Vazquez de Lara F, Bonomo L. The Successful Treatment of a Case of Linear Psoriasis with ixekizumab. Case Rep Dermatol Med. 2017;2017:3280215. doi: 10.1155/2017/3280215
SOURCE
Sherkin, Samantha, et al. “Pediatric Verrucous Psoriasis: A Case Report in a Pediatric Patient and Discussion of the Literature.” Journal of Drugs in Dermatology: JDD 21.8 (2022): 891-893.
Content and images used with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.