The 2023 Skin of Color Update in New York City featured a comprehensive discussion on the evolving landscape of treating acne, with a particular focus on medical and procedural approaches. Attendees had the unique opportunity to hear Dr. Valerie Callendar, professor of dermatology at Howard University College of Medicine in Washington, DC, and Dr. Andrew Alexis, Professor of Clinical Dermatology at Weill Cornell Medical College, highlight the latest developments in laser and light-based therapies, shedding light on the significance of these modalities in managing acne, particularly in patients with skin of color. In case you missed it, this article provides a detailed overview of the main takeaways from this lecture.
Medical Approaches to Acne
Dr. Alexis initiated the session by exploring medical treatments for acne. He emphasized the prevalence of acne among skin of color populations and the unique challenges associated with this condition. Notably, post-inflammatory hyperpigmentation (PIH) often accompanies acne in these patients, demanding a comprehensive approach.
The Burden of Post-Inflammatory Hyperpigmentation:
Dr. Alexis underscored the significance of addressing PIH, as it can be just as distressing to patients as the acne itself. A large international survey confirmed the prevalence of PIH as a common sequela of acne across diverse racial and ethnic backgrounds. Moreover, the development of scarring, especially keloidal and hypertrophic scars on the trunk, poses an additional challenge, occurring more frequently in skin of color populations.
Treatment Goals:
A critical aspect of managing acne in patients with skin of color is setting realistic treatment goals. Dr. Alexis highlighted that patients often expect clearance not only of acne lesions but also of PIH. In fact, Dr. Alexis AND Dr. Callender collaborated on a publication called “Racial Difference in Clinical Characteristics, Perceptions and Behaviors, and Psychosocial Impact of Adult Female Acne” that revealed significant disparities in preferences and treatment goals between White/Caucasian and non-White/Caucasian populations. Notably, Non-White females reported PIH to be most important for outcome. Thus, to achieve patient satisfaction and enable patient trust in their treatment regimen, it is essential to establish a shared decision-making process and provide a roadmap with realistic timelines for expected changes.
Medical treatments
Topical Retinoids: Topical retinoids, known for their effectiveness in acne management, were discussed as foundational therapies. Newer, better-tolerated retinoid formulations, such as Tazarotene and Tretinoin, were presented as promising options for addressing both acne and PIH. Dr. Alexis advocated for their use and stressed the importance of minimizing irritation and improving patient tolerability.
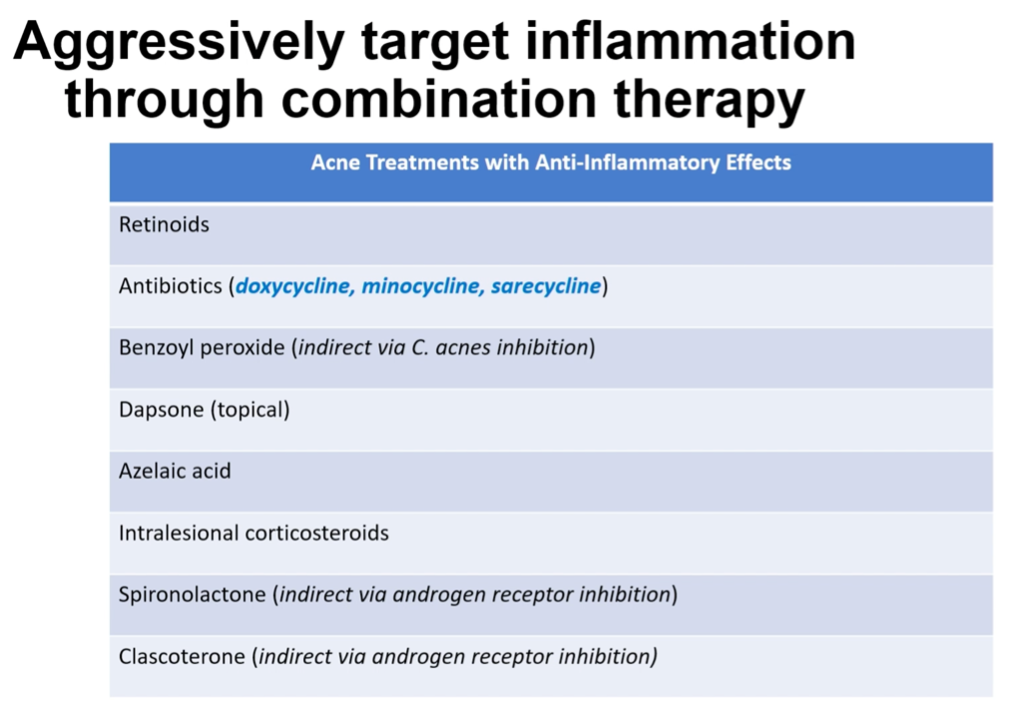
Addressing Inflammation: Subclinical inflammation, which affects both visible and non-visible lesions, was introduced as a key factor in acne. Leveraging agents with anti-inflammatory activity to design comprehensive treatment regimens was a recommended approach. Examples of such agents included Clascoterone, which inhibits androgen receptors, and Tretinoin for comedolysis and anti-inflammatory effects. More anti-inflammatory medication candidates are listed in the Dr. Alexis’ table below.
Combination Regimens:
Dr. Alexis emphasized the importance of targeting multiple etiologic factors in acne such as comedones, inflammation, C. acnes bacteria, and sebum production. Combination regimens were highlighted as an effective strategy for achieving optimal results. He brought attention to a recently studied combination of microencapsulated benzoyl peroxide and microencapsulated tretinoin for the treatment of acne vulgaris, and a triple therapy with clindamycin phosphate 1.2%/adapalene 0.15%/ benzoyl peroxide 3.1% gel that can serve to help improve treatment adherence in patients due to greater simplicity of use.1,2
Addressing Acne Disparities:
Dr. Alexis addressed disparities in the use of acne therapies for skin of color patients in real-world settings. He cited studies that demonstrated the underuse of topical retinoids, isotretinoin, oral antibiotics, and spironolactone in non-Hispanic blacks vs non-Hispanic white patients.3,4 He stressed the benefits of oral agents like Sarecycline, which have demonstrated significant efficacy, safety, and improved quality of life across diverse populations.5 It is important to appropriately counsel patients to ensure treatment adherence, improve tolerability, and minimize side effects.6
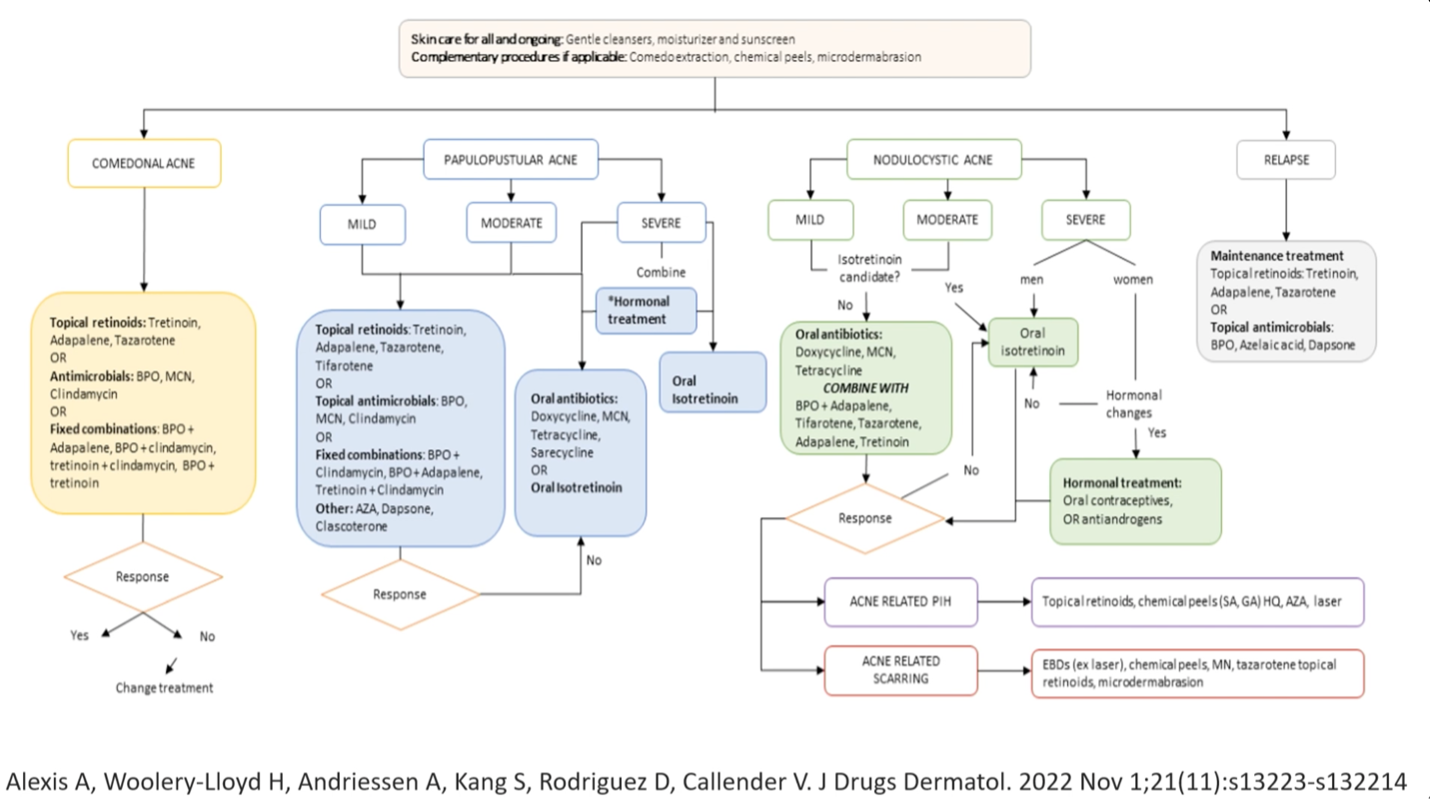
Dr. Alexis concluded his presentation by providing an algorithm for treating acne in patients with skin of color, encompassing the management of associated PIH and the utilization of procedures to address both acne and its sequelae.
Procedural Approaches to Treating Acne
Following Dr. Alexis’ insightful talk, Dr. Valerie Callender took the stage to discuss the use of light-based devices and lasers for treating acne, particularly their relevance in patients with skin of color.
She notes that the guidelines for the treatment of acne in 2016 stated limited evidence to recommend pulse dye laser, glycolic acid peels and salicylic acid peels for the routine treatment of acne. At this point, PDT had the most existing evidence for treating acne out of all lasers and light devices.7 Fast forward to 2022, and you see all the modalities recommended for the treatment of acne in the table below. The problem is that you get dyschromia in skin of color.8
The 650 Microsecond 1064 Nd:YAG Laser
Dr. Callender introduced the 650-microsecond 1064 Nd:YAG laser as an effective tool for targeting inflammation, the vessels that feed sebum production, and C. acnes bacteria. This laser was noted for its suitability in managing mild to moderate acne, and it exhibited excellent safety profiles for patients with skin of color.
She presented compelling case studies showcasing the effectiveness of the 650-microsecond laser in reducing inflammatory lesions, improving post-inflammatory erythema, and The treatment’s compatibility with patients on isotretinoin was also highlighted, revealing significant improvements in both acne severity and quality of life.10 In summary, this laser system boasts the following key attributes:
-
- Selective targeting of hemoglobin and water, optimizing treatment precision.
- FDA clearance for addressing mild to moderate inflammatory acne, attesting to its safety and efficacy.
- Profound reduction of inflammation and induction of sebaceous gland damage via bulk heating, thus curbing sebum production.
- Induction of coagulation within dermal blood vessels, contributing to improved acne outcomes.
- Minimal discomfort during treatment so no anesthetic is needed.
- Recommended treatment regimen comprising 3 to 6 sessions, spaced 1 to 2 weeks apart, and extending to 4-week intervals in individuals with skin of color.
- Only minutes of transient erythema, ensuring minimal downtime.
- Improvement in PIH in SOC patients, addressing a frequently encountered concern in pigmented skin.


The 1726-Nanometer Laser
The 1726-nanometer laser, another valuable tool in acne management, demonstrated the ability to target sebocytes and reduce inflammation without affecting epidermis or dermis. Long-term studies suggested sustained benefits with an exceptional safety profile. Dr. Callender presented photographs illustrating substantial improvements in acne and post-inflammatory 11
An advanced version of the 1726-nanometer laser featuring real-time temperature monitoring was also briefly introduced. This innovation enhances safety and comfort by ensuring precise temperature control during treatments, providing cooling whenever the temperature elevation is sensed. The device exhibited impressive long-term results, with sustained reductions in inflammatory lesions over a year after the last treatment and with similar therapeutic outcomes across all skin types.12
Progress of acne condition at six months, one year, and two years after three-session 1726 nm laser treatment of a male subject, Asian, age 25, at the baseline visit, with a Fitzpatrick skin type III and moderate acne severity (IGA score =3). Photo from Goldberg et al. 2023.11
Photo-Pneumatic Device with Broadband Light Source
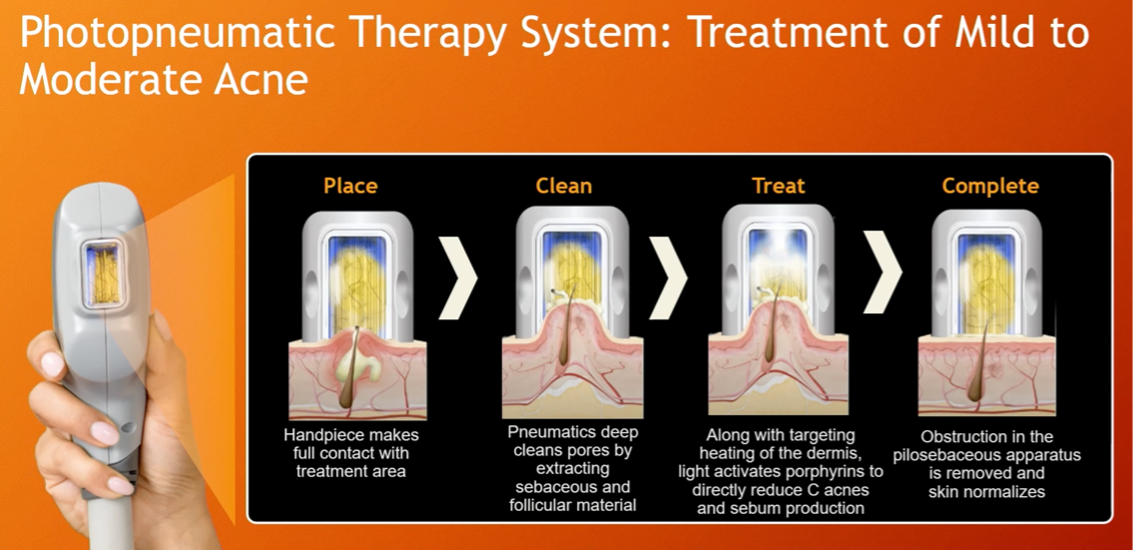
Dr. Callender ended with the discussion of a photo-pneumatic device that combines vacuum technology with broadband light energy. This handheld device was found effective in treating both comedonal and inflammatory mild to moderate acne. Specifications regarding this device are the following:
-
- Wavelength: 500-1200 m
- Pulse Length: up to 25 m/s (minimum of 2 m/s)
-
-
Slide courtesy of Dr. Valerie Callender Spot Size: 12.7mm x 25.4mm and 10mm X 12mm
- Repetition Rate:
- Single Pulse: One pulse every 2 seconds
- Double Pulse: One pulse every 2.5 seconds
- Triple Pulse: One pulse every 3 seconds
- Dimensions: 13 in x 16.5 in x 15 in
-
Photopneumatic technology that combines vacuum with pulsed broadband light delivered through a liquid-cooled handheld delivery system.13 Its mechanism of action relies on the following two aspects:
-
- Vacuum: Helps open the follicular openings to clear bacteria and follicular contents from pilosebaceous unit.
- Pulsed Broadband Light: This energy destroys C. acnes AND reduces sebum production.
The whole procedure takes a maximum of 15 minutes, performed every 1-2 weeks for 4-6 sessions.
Photos demonstrated its capacity to clear comedones (without requiring a comedone extractor!) and inflammatory papules effectively, contributing to overall patient satisfaction.
In conclusion, the integration of laser and light-based devices into acne management provides dermatologists with powerful tools for enhancing treatment outcomes, particularly in patients with skin of color. Such procedures may serve as an alternative to isotretinoin and can be used in combination with acne mediations for enhanced, faster results.
These procedures offer effective ways to target inflammation, sebum production, and bacterial overgrowth while minimizing the risk of post-inflammatory hyperpigmentation. The safety and efficacy of these technologies make them invaluable additions to the dermatologist’s toolkit in the quest for clearer, healthier skin for all patients, regardless of their skin type or color.
References:
-
- Del Rosso, J., Sugarman, J., Green, L., Lain, T., Levy-Hacham, O., Mizrahi, R., & Gold, L. S. (2023). Efficacy and safety of microencapsulated benzoyl peroxide and microencapsulated tretinoin for the treatment of acne vulgaris: Results from two phase 3 double-blind, randomized, vehicle-controlled studies. Journal of the American Academy of Dermatology, 89(4), 719–727. https://doi.org/10.1016/j.jaad.2023.05.093
- Stein Gold L, Kircik LH, Tanghetti, Baldwin H, Draelos Z, Gold M, Lain E, Pariser DM, Sadick N, Pillai R, and Bhatt V. Efficacy and safety of a fixed-dose clindamycin phosphate 1.2%, benzoyl peroxide 3.1%, and adapalene 0.15% gel for moderate-to-severe acne: Randomized Phase 2 and Phase 3 studies of the first triplecombination drug. J Clin Aesthet Dermatol 2023; 16(4):S6.
- Bell, M. A., Whang, K. A., Thomas, J., Aguh, C., & Kwatra, S. G. (2020). Racial and Ethnic Disparities in Access to Emerging and Frontline Therapies in Common Dermatological Conditions: A Cross-Sectional Study. Journal of the National Medical Association, 112(6), 650–653. https://doi.org/10.1016/j.jnma.2020.06.009
- Barbieri, J. S., Shin, D. B., Wang, S., Margolis, D. J., & Takeshita, J. (2020). Association of Race/Ethnicity and Sex With Differences in Health Care Use and Treatment for Acne. JAMA dermatology, 156(3), 312–319. https://doi.org/10.1001/jamadermatol.2019.4818
- Graber, E., Baldwin, H., Harper, J., Stein Gold, L., Alexis, A., Fried, R., Rieder, E., Del Rosso, J., Kircik, L., Narayanan, S., Koscielny, V., Kasujee, I., & Hebert, A. (2023). Investigator global assessment (IGA) of Acne Vulgaris and IGA Success among patients with moderate to severe non-nodular Acne Vulgaris (AV) administered sarecycline in community practices across the U.S: PROSES study analysis by gender and age. SKIN The Journal of Cutaneous Medicine, 7(2), s156. https://doi.org/10.25251/skin.7.supp.156
- Alexis, A. F., Woolery-Lloyd, H., Williams, K., Andriessen, A., Callender, V. D., Kang, S., Rodriquez, D., & Tan, J. (2021). Racial/Ethnic Variations in Acne: Implications for Treatment and Skin Care Recommendations for Acne Patients With Skin of Color. Journal of drugs in dermatology : JDD, 20(7), 716–725. https://doi.org/10.36849/JDD.6169
- Zaenglein, A. L., Pathy, A. L., Schlosser, B. J., Alikhan, A., Baldwin, H. E., Berson, D. S., Bowe, W. P., Graber, E. M., Harper, J. C., Kang, S., Keri, J. E., Leyden, J. J., Reynolds, R. V., Silverberg, N. B., Stein Gold, L. F., Tollefson, M. M., Weiss, J. S., Dolan, N. C., Sagan, A. A., Stern, M., … Bhushan, R. (2016). Guidelines of care for the management of acne vulgaris. Journal of the American Academy of Dermatology, 74(5), 945–73.e33. https://doi.org/10.1016/j.jaad.2015.12.037
- Tong, L. X., & Brauer, J. A. (2017). Lasers, Light, and the Treatment of Acne: A Comprehensive Review of the Literature. Journal of drugs in dermatology : JDD, 16(11), 1095–1102.
- Kesty K, Goldberg DJ. 650 use 1064m Nd: YAG laser treatment of acne: A double-blind randomized control study. J Cosmet Dermatol. 2020 Sep; 19(9):2295-2300.
- Gold, M. H., Manturova, N. E., Kruglova, L. S., & Ikonnikova, E. V. (2020). Treatment of Moderate to Severe Acne and Scars With a 650-Microsecond 1064-nm Laser and Isotretinoin. Journal of drugs in dermatology : JDD, 19(6), 646–651. https://doi.org/10.36849/JDD.2020.M5108
- Goldberg, D., Kothare, A., Doucette, M., Kaur, A., Ronan, S., Fromowitz, J., & Hamidi-Sakr, A. (2023). Selective photothermolysis with a novel 1726 nm laser beam: A safe and effective solution for acne vulgaris. Journal of cosmetic dermatology, 22(2), 486–496. https://doi.org/10.1111/jocd.15602
- Alexiades, M., Kothare, A., Goldberg, D., & Dover, J. S. (2023). Novel 1726 nm laser demonstrates durable therapeutic outcomes and tolerability for moderate-to-severe acne across skin types. Journal of the American Academy of Dermatology, 89(4), 703–710. https://doi.org/10.1016/j.jaad.2023.05.085
- Dagnelie MA et al. Int J Dermatol. 2022 May 6. doi: 10.1111 / ijd. 16220. Online ahead of print. 2 Siddiqui Ret al. Foli Microbiol. 2022 Jun 16; doi: 10.1007/s12223-022-00982-5.
This information was presented by Drs. Andrew Alexis and Valerie Callender during the 2023 Skin of Color Update conference. The above highlights from their lecture were written and compiled by Dr. Sarah Millan.
Did you enjoy this article? You can find more on Medical Dermatology here.