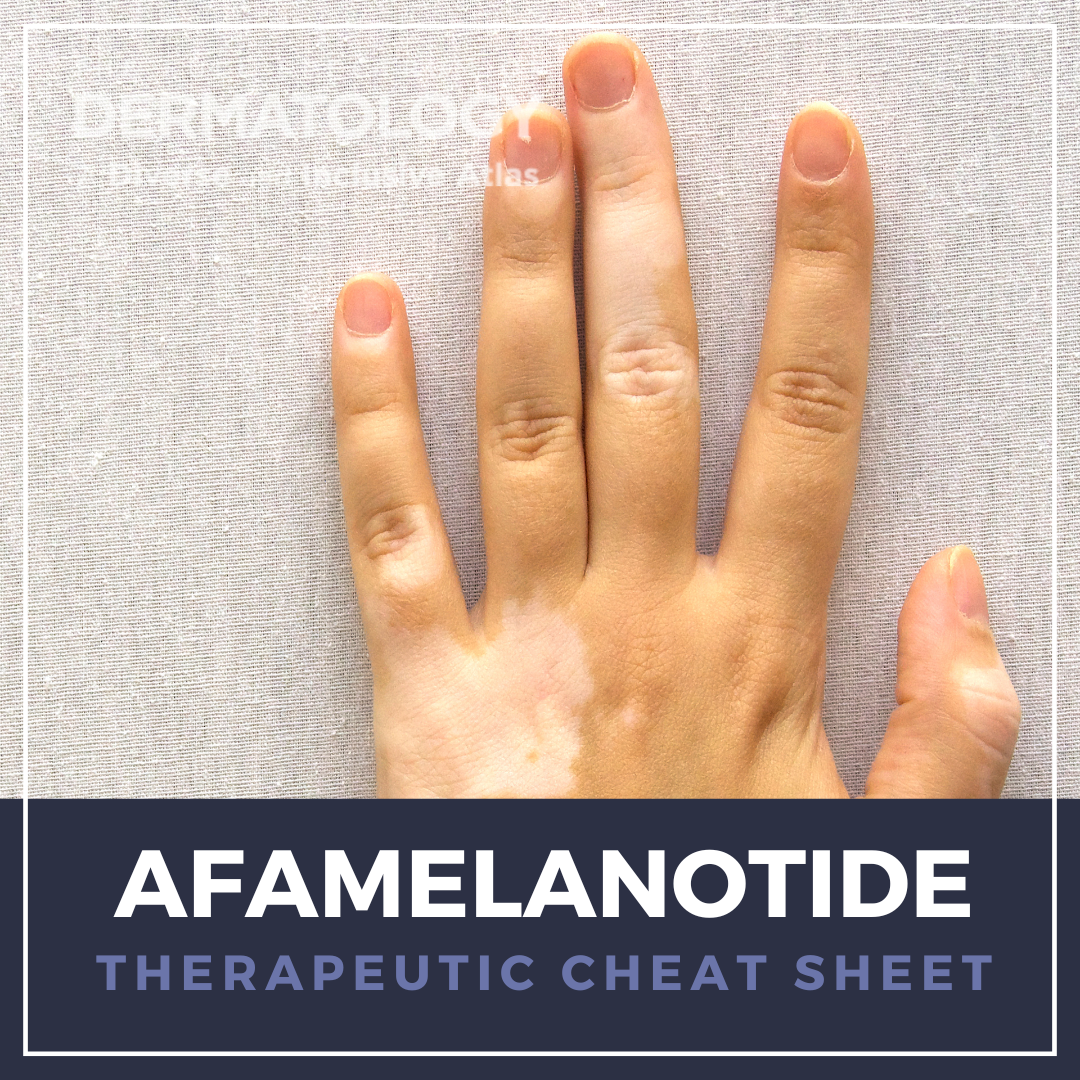
Photosensitive skin conditions can result in cutaneous and systemic symptoms that can have a marked effect on quality of life due to ubiquitous UV exposure. Erythropoietic protoporphyria, for example, can cause severe photodermatitis, excruciating burning and neuropathic pain, nausea, and deep-rooted fear of sunlight that leads to debilitating lifestyle modifications such as remaining indoors. We continue our series, Therapeutic Cheat Sheet, with a closer look at afamelanotide, which is approved by the United States Food and Drug Administration for adults with erythropoietic protoporphyria. Afamelanotide is also used off-label for patients with generalized vitiligo and has potential for utility in other photodermatoses such as polymorphous light eruption and solar urticaria.
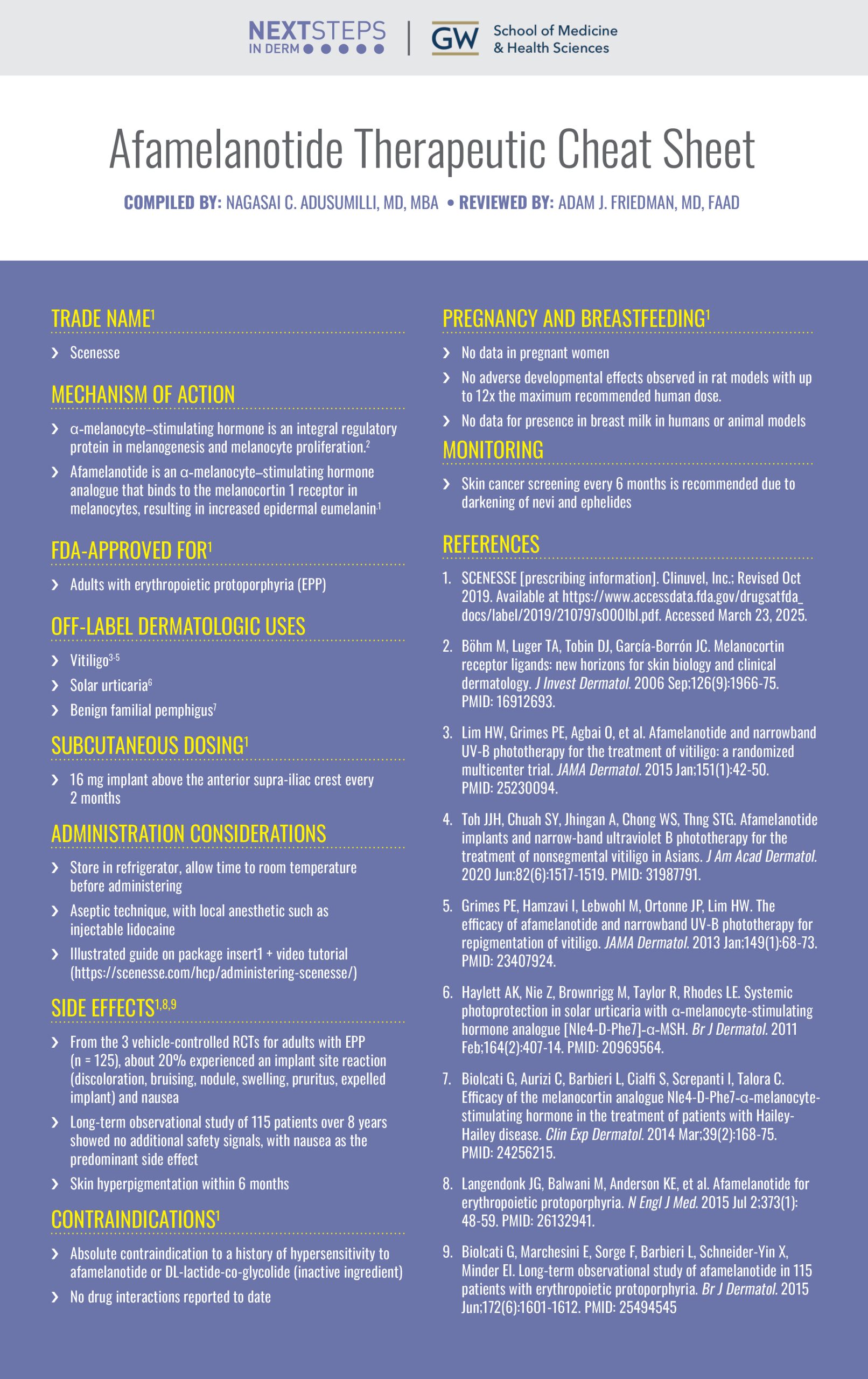
Afamelanotide Therapeutic Cheat Sheet
Compiled by: Nagasai C. Adusumilli, MD, MBA | Reviewed by: Adam J. Friedman, MD, FAAD
TRADE NAME1
-
- Scenesse
MECHANISM OF ACTION
-
- α-melanocyte–stimulating hormone is an integral regulatory protein in melanogenesis and melanocyte proliferation.2
- Afamelanotide is an α-melanocyte–stimulating hormone analogue that binds to the melanocortin 1 receptor in melanocytes, resulting in increased epidermal eumelanin.1
FDA-APPROVED FOR1
-
- Adults with erythropoietic protoporphyria (EPP)
OFF-LABEL DERMATOLOGIC USES
-
- Vitiligo3-5
- Solar urticaria6
- Benign familial pemphigus7
SUBCUTANEOUS DOSING1
-
- 16 mg implant above the anterior supra-iliac crest every 2 months
ADMINISTRATION CONSIDERATIONS
-
- Store in refrigerator, allow time to room temperature before administering
- Aseptic technique, with local anesthetic such as injectable lidocaine
- Illustrated guide on package insert1 + video tutorial (https://scenesse.com/hcp/administering-scenesse/)
SIDE EFFECTS1,8,9
-
- From the 3 vehicle-controlled RCTs for adults with EPP (n = 125), about 20% experienced an implant site reaction (discoloration, bruising, nodule, swelling, pruritus, expelled implant) and nausea.
- Long-term observational study of 115 patients over 8 years showed no additional safety signals, with nausea as the predominant side effect.
- Skin hyperpigmentation within 6 months
CONTRAINDICATIONS1
-
- Absolute contraindication to a history of hypersensitivity to afamelanotide or DL-lactide-co-glycolide (inactive ingredient)
- No drug interactions reported to date
PREGNANCY AND BREASTFEEDING1
-
- No data in pregnant women
- No adverse developmental effects observed in rat models with up to 12x the maximum recommended human dose.
- No data for presence in breast milk in humans or animal models
MONITORING
-
- Skin cancer screening every 6 months is recommended due to darkening of nevi and ephelides.
FURTHER READING
If you would like to learn more about afamelanotide, check out the following articles in the Journal of Drugs in Dermatology:
Afamelanotide: An Orphan Drug with Potential for Broad Dermatologic Applications
Wu, R. Cotliar
Abstract
Afamelanotide (SCENESSE®) is a synthetic analogue of α-melanocyte-stimulating hormone that is FDA-approved to increase pain-free sunlight exposure in adult patients with erythropoietic protoporphyria. Its dual photoprotective and anti-inflammatory effects also make it a promising therapy for other photosensitive dermatologic diseases that are resistant to treatment. The PubMed/MEDLINE and ClinicalTrials.gov databases were searched for literature and ongoing trials describing the use of afamelanotide in treating cutaneous diseases. There is randomized controlled trial (RCT) evidence for the successful use of afamelanotide in several conditions beyond erythropoietic protoporphyria, including polymorphic light eruption and vitiligo. Smaller studies have also demonstrated its efficacy in treating acne vulgaris, Hailey-Hailey disease, and solar urticaria. No serious adverse effects with afamelanotide use have been reported, though diffuse hyperpigmentation is experienced by almost all patients. Larger scale studies are needed to confirm the efficacy of afamelanotide in treating dermatologic conditions beyond erythropoietic protoporphyria, and further research should focus on determining the safety, efficacy, and optimal dosing of afamelanotide for pediatric patients.
J Drugs Dermatol. 20(3):290-294. doi:10.36849/JDD.2021.5526
Into the Light: Treatment of Erythropoietic Protoporphyria in the United States
Resnik, D. Targett, BI. Resnik
Abstract
Background: Erythropoietic protoporphyria (EPP) is a rare disease that causes disabling cutaneous photosensitivity with pain and burning sensations. In 2019, afamelanotide, an α-melanocyte-stimulating hormone analogue, was approved in the United States for treatment of EPP. In this study, patients receiving afamelanotide filled out questionnaires assessing the benefit of treatment. Outcomes measured included: return to normal activities, experience of phototoxic reactions, effect on patient confidence, and more. Patients ranked their experience on a descriptive scale ranging from “very much” to “never”.
Results: Prior to treatment, 75% of patients indicated that EPP affected their lives “very much” or “a lot”. This number fell to 11% after the 1st implant and to 0% after each subsequent implant. The number of patients that willingly ventured outside increased with each subsequent implant.
Conclusion: The results of this study clearly show that afamelanotide treatment can dramatically and positively impact the lives of EPP patients.
J Drugs Dermatol. 2023;22(9):941-949. doi:10.36849/JDD.7126R1
REFERENCES
-
- SCENESSE [prescribing information]. Clinuvel, Inc.; Revised Oct 2019. Available at https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/210797s000lbl.pdf. Accessed March 23, 2025.
- Böhm M, Luger TA, Tobin DJ, García-Borrón JC. Melanocortin receptor ligands: new horizons for skin biology and clinical dermatology. J Invest Dermatol. 2006 Sep;126(9):1966-75. PMID: 16912693.
- Lim HW, Grimes PE, Agbai O, et al. Afamelanotide and narrowband UV-B phototherapy for the treatment of vitiligo: a randomized multicenter trial. JAMA Dermatol. 2015 Jan;151(1):42-50. PMID: 25230094.
- Toh JJH, Chuah SY, Jhingan A, Chong WS, Thng STG. Afamelanotide implants and narrow-band ultraviolet B phototherapy for the treatment of nonsegmental vitiligo in Asians. J Am Acad Dermatol. 2020 Jun;82(6):1517-1519. PMID: 31987791.
- Grimes PE, Hamzavi I, Lebwohl M, Ortonne JP, Lim HW. The efficacy of afamelanotide and narrowband UV-B phototherapy for repigmentation of vitiligo. JAMA Dermatol. 2013 Jan;149(1):68-73. PMID: 23407924.
- Haylett AK, Nie Z, Brownrigg M, Taylor R, Rhodes LE. Systemic photoprotection in solar urticaria with α-melanocyte-stimulating hormone analogue [Nle4-D-Phe7]-α-MSH. Br J Dermatol. 2011 Feb;164(2):407-14. PMID: 20969564.
- Biolcati G, Aurizi C, Barbieri L, Cialfi S, Screpanti I, Talora C. Efficacy of the melanocortin analogue Nle4-D-Phe7-α-melanocyte-stimulating hormone in the treatment of patients with Hailey-Hailey disease. Clin Exp Dermatol. 2014 Mar;39(2):168-75. PMID: 24256215.
- Langendonk JG, Balwani M, Anderson KE, et al. Afamelanotide for erythropoietic protoporphyria. N Engl J Med. 2015 Jul 2;373(1):48-59. PMID: 26132941.
- Biolcati G, Marchesini E, Sorge F, Barbieri L, Schneider-Yin X, Minder EI. Long-term observational study of afamelanotide in 115 patients with erythropoietic protoporphyria. Br J Dermatol. 2015 Jun;172(6):1601-1612. PMID: 25494545.
Did you enjoy this Therapeutic Cheat Sheet? You can find more here.