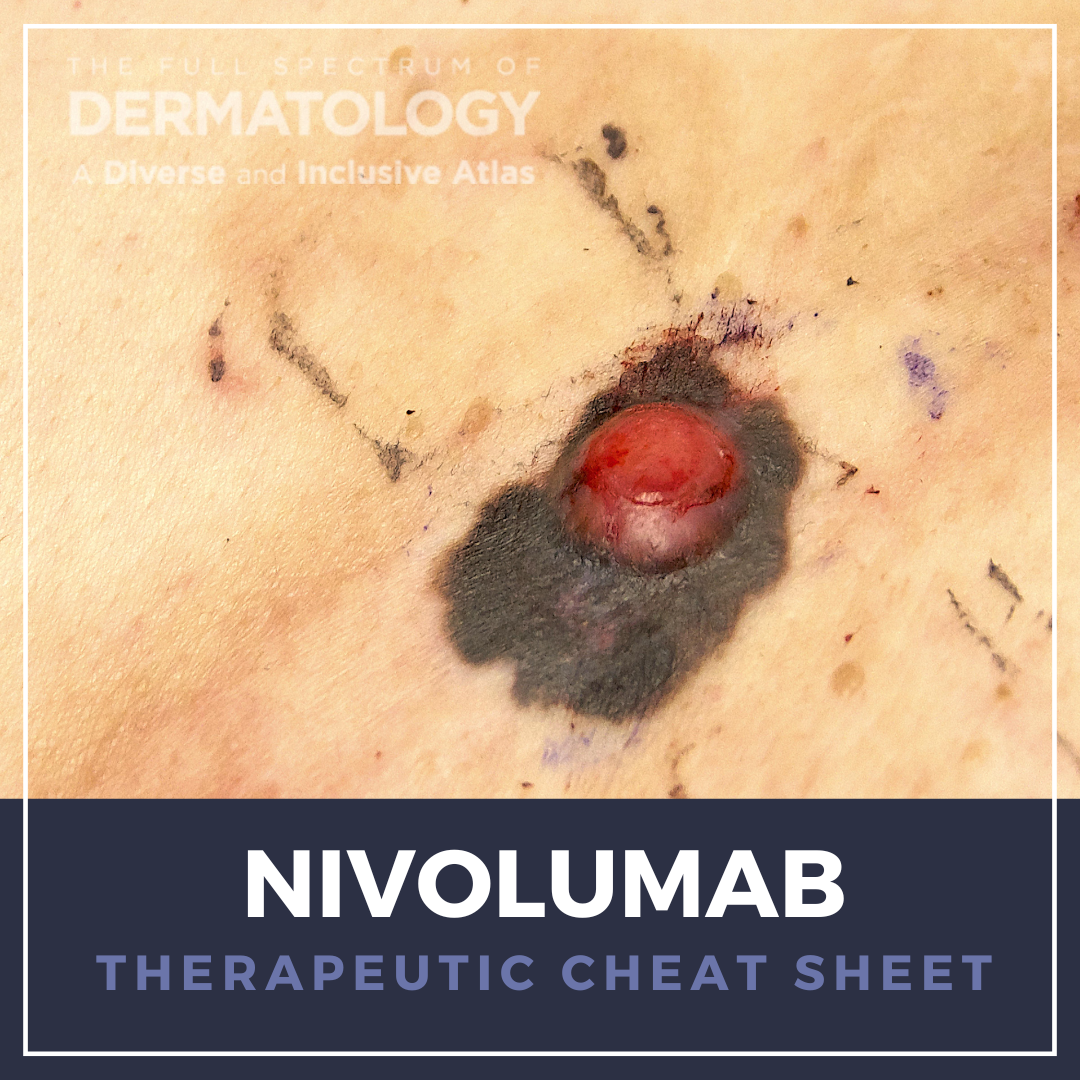
Nivolumab, a programmed death-1 (PD-1) immune checkpoint inhibitor, is a cornerstone in the evolving field of immuno-oncology. Originally developed for advanced cancers, nivolumab functions by blocking PD-1–mediated immune suppression, thereby enhancing T-cell–mediated antitumor responses. In dermatology, its relevance has grown not only because of its utility in melanoma treatment and cutaneous immune-related adverse events (irAEs), but also its emerging off-label potential in treating other varieties of skin cancer. As with other immune checkpoint inhibitors, nivolumab requires multidisciplinary management and vigilant monitoring due to potentially severe immune-related complications.
We continue our Therapeutic Cheat Sheet series with a closer look at the dermatologic applications of nivolumab, which is FDA-approved for the treatment of a variety of advanced cancers, including melanoma, and used off-label for the management of cutaneous squamous cell carcinoma and Merkel cell carcinoma.
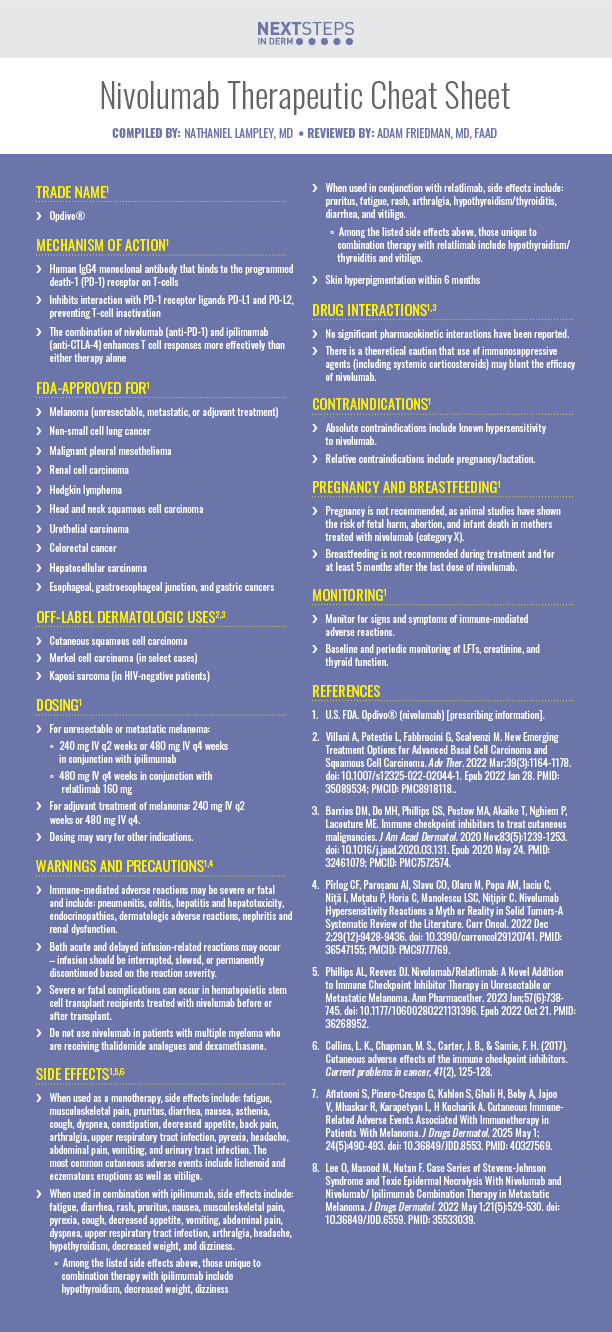
Nivolumab Therapeutic Cheat Sheet
Compiled by: Nathaniel Lampley, MD | Reviewed by: Adam Friedman, MD, FAAD
TRADE NAME
-
- Opdivo®
MECHANISM OF ACTION1
-
- Human IgG4 monoclonal antibody that binds to the programmed death-1 (PD-1) receptor on T-cells
- Inhibits interaction with PD-1 receptor ligands PD-L1 and PD-L2, preventing T-cell inactivation
- The combination of nivolumab (anti-PD-1) and ipilimumab (anti-CTLA-4) enhances T cell responses more effectively than either therapy alone
FDA-APPROVED FOR1
-
- Melanoma (unresectable, metastatic, or adjuvant treatment)
- Non-small cell lung cancer
- Malignant pleural mesothelioma
- Renal cell carcinoma
- Hodgkin lymphoma
- Head and neck squamous cell carcinoma
- Urothelial carcinoma
- Colorectal cancer
- Hepatocellular carcinoma
- Esophageal, gastroesophageal junction, and gastric cancers
OFF-LABEL DERMATOLOGIC USES2,3
-
- Cutaneous squamous cell carcinoma
- Merkel cell carcinoma (in select cases)
- Kaposi sarcoma (in HIV-negative patients)
DOSING1
-
- For unresectable or metastatic melanoma:
- 240 mg IV q2 weeks or 480 mg IV q4 weeks in conjunction with ipilimumab
- 480 mg IV q4 weeks in conjunction with relatlimab 160 mg
- For adjuvant treatment of melanoma: 240 mg IV q2 weeks or 480 mg IV q4.
- Dosing may vary for other indications.
- For unresectable or metastatic melanoma:
WARNINGS AND PRECAUTIONS1,4
-
- Immune-mediated adverse reactions may be severe or fatal and include: pneumonitis, colitis, hepatitis and hepatotoxicity, endocrinopathies, dermatologic adverse reactions, nephritis and renal dysfunction.
- Both acute and delayed infusion-related reactions may occur – infusion should be interrupted, slowed, or permanently discontinued based on the reaction severity.
- Severe or fatal complications can occur in hematopoietic stem cell transplant recipients treated with nivolumab before or after transplant.
- Do not use nivolumab in patients with multiple myeloma who are receiving thalidomide analogues and dexamethasone.
SIDE EFFECTS1,5,6
-
- When used as a monotherapy, side effects include: fatigue, musculoskeletal pain, pruritus, diarrhea, nausea, asthenia, cough, dyspnea, constipation, decreased appetite, back pain, arthralgia, upper respiratory tract infection, pyrexia, headache, abdominal pain, vomiting, and urinary tract infection. The most common cutaneous adverse events include lichenoid and eczematous eruptions as well as vitiligo.
- When used in combination with ipilimumab, side effects include: fatigue, diarrhea, rash, pruritus, nausea, musculoskeletal pain, pyrexia, cough, decreased appetite, vomiting, abdominal pain, dyspnea, upper respiratory tract infection, arthralgia, headache, hypothyroidism, decreased weight, and dizziness.
- Among the listed side effects above, those unique to combination therapy with ipilimumab include hypothyroidism, decreased weight, dizziness
- When used in conjunction with relatlimab, side effects include: pruritus, fatigue, rash, arthralgia, hypothyroidism/thyroiditis, diarrhea, and vitiligo.
- Among the listed side effects above, those unique to combination therapy with relatlimab include hypothyroidism/thyroiditis and vitiligo.
DRUG INTERACTIONS1,3
-
- No significant pharmacokinetic interactions have been reported.
- There is a theoretical caution that use of immunosuppressive agents (including systemic corticosteroids) may blunt the efficacy of nivolumab.
CONTRAINDICATIONS1
-
- Absolute contraindications include known hypersensitivity to nivolumab.
- Relative contraindications include pregnancy/lactation.
PREGNANCY AND BREASTFEEDING1
-
- Pregnancy is not recommended, as animal studies have shown the risk of fetal harm, abortion, and infant death in mothers treated with nivolumab (category X).
- Breastfeeding is not recommended during treatment and for at least 5 months after the last dose of nivolumab.
MONITORING1
-
- Monitor for signs and symptoms of immune-mediated adverse reactions.
- Baseline and periodic monitoring of LFTs, creatinine, and thyroid function.
FURTHER READING
If you would like to learn more about nivolumab, check out the following articles in the Journal of Drugs in Dermatology:
Cutaneous Immune-Related Adverse Events Associated With Immunotherapy in Patients With Melanoma
Aflatooni, G. Pinero-Crespo, S. Kahlon, H. Ghali, A. Boby, V. Jajoo, R. Mhaskar, L. Karapetyan, A.H. Kucharik
ABSTRACT
Background: Cutaneous immune-related adverse events (irCAEs) have been commonly reported as a consequence of immune checkpoint inhibitors (ICIs) for the treatment of advanced stage III and stage IV melanoma.
Objective and Methods: We sought to compare systemic irAEs in melanoma patients taking ICIs, with and without irCAEs in a retrospective cohort study of 147 patients at Moffitt Cancer Center.
Results: 38.8% of patients experienced an irCAE on adjuvant ICI therapy, and 54.4% of these patients also experienced a systemic irAE. There was no significant association between irCAEs and systemic irAEs in the adjuvant treatment group (P=0.240). Among patients who progressed on first-line ICI therapy, 28.8% of patients experienced an irCAE on second-line ICI therapy. Of these patients, 53.3% also experienced a systemic irAE. There was a significant association between irCAEs and systemic irAE in the metastatic treatment group (P<0.001). The median overall survival for patients who encountered an irCAE was 118 months, compared to 69 months for those who did not experience an irCAE (P=0.102).
Conclusion: Patients with stage III and stage IV melanoma who progress on first-line ICI therapy and experience an irCAE are more likely to also experience a systemic irAE.
Lee, M. Masood, F. Nutan
ABSTRACT
Nivolumab (anti PD-1 antibody) and ipilimumab (anti CTLA-4 antibody) are immune checkpoint inhibitors (ICI) that effectively stimulate the native T cell response and lead to an antitumor response. The medications have been approved for the treatment of metastatic melanoma. However, ICIs are associated with higher risk for cutaneous immune-related adverse events (irAEs). Although most of the adverse events present as maculopapular rash, some patients develop Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis which are dermatologic emergencies with high mortality. We report a fatal case of SJS associated with nivolumab and a non-fatal case of TEN with nivolumab/ipilimumab combination therapy in patients with metastatic melanoma. It is also not unusual to develop SJS or TEN after weeks or months on checkpoint inhibitor therapy. Given the high rate for mortality, dermatologists and other clinicians should closely follow any rash from these immunotherapies due to the risk for future development of SJS or TEN.
References
-
- U.S. FDA. Opdivo® (nivolumab) [prescribing information].
- Villani A, Potestio L, Fabbrocini G, Scalvenzi M. New Emerging Treatment Options for Advanced Basal Cell Carcinoma and Squamous Cell Carcinoma. Adv Ther. 2022 Mar;39(3):1164-1178. doi: 10.1007/s12325-022-02044-1. Epub 2022 Jan 28. PMID: 35089534; PMCID: PMC8918118.
- Barrios DM, Do MH, Phillips GS, Postow MA, Akaike T, Nghiem P, Lacouture ME. Immune checkpoint inhibitors to treat cutaneous malignancies. J Am Acad Dermatol. 2020 Nov;83(5):1239-1253. doi: 10.1016/j.jaad.2020.03.131. Epub 2020 May 24. PMID: 32461079; PMCID: PMC7572574.
- Pîrlog CF, Paroșanu AI, Slavu CO, Olaru M, Popa AM, Iaciu C, Niță I, Moțatu P, Horia C, Manolescu LSC, Nițipir C. Nivolumab Hypersensitivity Reactions a Myth or Reality in Solid Tumors-A Systematic Review of the Literature. Curr Oncol. 2022 Dec 2;29(12):9428-9436. doi: 10.3390/curroncol29120741. PMID: 36547155; PMCID: PMC9777769.
- Phillips AL, Reeves DJ. Nivolumab/Relatlimab: A Novel Addition to Immune Checkpoint Inhibitor Therapy in Unresectable or Metastatic Melanoma. Ann Pharmacother. 2023 Jun;57(6):738-745. doi: 10.1177/10600280221131396. Epub 2022 Oct 21. PMID: 36268952.
- Collins, L. K., Chapman, M. S., Carter, J. B., & Samie, F. H. (2017). Cutaneous adverse effects of the immune checkpoint inhibitors. Current problems in cancer, 41(2), 125-128.
- Aflatooni S, Pinero-Crespo G, Kahlon S, Ghali H, Boby A, Jajoo V, Mhaskar R, Karapetyan L, H Kucharik A. Cutaneous Immune-Related Adverse Events Associated With Immunotherapy in Patients With Melanoma. J Drugs Dermatol. 2025 May 1;24(5):490-493. doi: 10.36849/JDD.8553. PMID: 40327569.
- Lee O, Masood M, Nutan F. Case Series of Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis With Nivolumab and Nivolumab/ Ipilimumab Combination Therapy in Metastatic Melanoma. J Drugs Dermatol. 2022 May 1;21(5):529-530. doi: 10.36849/JDD.6559. PMID: 35533039.
Did you enjoy this Therapeutic Cheat Sheet? You can find more here.