Alopecia areata is a form of non-scarring hair loss that affects both children and adults, causing significant quality of life impairment. Varying from localized to widespread hair loss, including alopecia totalis and universalis variants, alopecia areata can be self-resolving or chronic in its course. For years and in some cases centuries, treatment was limited to caustic substances that irritate the skin and corticosteroids. Until recently, the current treatment modalities were not that different from these traditional strategies. To hear about what’s new as well as the established therapies, keep reading here!
One of the highlights of the 2021 ODAC Virtual Conference was from the hair loss guru himself, Dr. Jerry Shapiro, Professor at NYU Grossman School of Medicine, and his presentation on an evidence-based approach to treating alopecia areata to maximize regrowth and mitigate adverse events.
Alopecia areata treatment has been documented as early as the 1800s, when caustic substances derived from plants were noted to induce blistering and hair regrowth. Over the last two hundred years, treatment has expanded to include corticosteroids in addition to the contact immunotherapy, as reviewed by Strazzulla LC, et al. in “Alopecia areata: An appraisal of new treatment approaches and overview of current therapies” in JAAD in 2018. However, the janus kinase (Jak) inhibitors have revolutionized treatment options for alopecia areata.
Corticosteroids: Topical and Intralesional
Dr. Shapiro reviewed some of the landmark studies that demonstrated the efficacy of topical and injected corticosteroids for alopecia areata. One of the first studies in 2003 demonstrated the efficacy of nightly clobetasol ointment in a split scalp study to accelerate regrowth (Tosti A,et al. Clobetasol propionate 0.05% under occlusion in the treatment of alopecia totalis/universalis. J Am Acad Dermatol. 2003 Jul;49(1):96-8.).
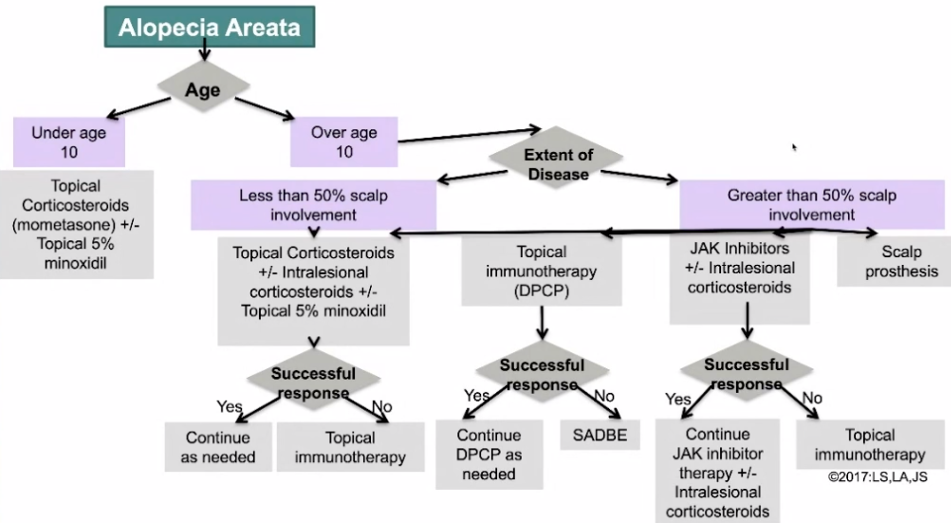
If the patient that can tolerate the procedure, intralesional corticosteroids can also be an effective treatment modality to adjunct topicals. What is the best concentration of triamcinolone acetonide to use for scalp injections? Based on a study in 2015, intralesional injections every 6 weeks for 36 weeks of different concentrations of triamcinolone (2.5 mg/mL, 5 mg/mL, 10 mg/mL, versus sa-line), it was shown triamcinolone does result in more regrowth than saline, and there is no added benefit above triamcinolone concentration of 2.5mg/mL (Chu TW, et al. Benefit of different concentrations of intralesional triamcinolone acetonide in alopecia areata: An intrasubject pilot study. J Am Acad Dermatol. 2015 Aug;73(2):338-40).
Based on these results, Dr. Shapiro recommends using 2.5mg/mL triamcinolone concentration which can be used for both the scalp and eyebrows. His approach it to prepare 9mL total per treatment, which is a total of 90 injections (80 for scalp and 10 for eyebrows). Dr. Shapiro reported his treatment approach of combining topical clobetasol solution 0.05% BID with topical minox-idil 5% solution BID with these intralesional injections monthly to optimize regrowth.
Contact Immunotherapy
Using Diphenylcyclopropenone 1.5% solution (DPCP) in the office is a great option for patients with extensive alopecia (>50% of scalp involvement). Patients that do not respond to DPCP can be treated with squaric acid dibutylester (SADBE). These topical agents cause an intentional allergic contact dermatitis that shifts the immune reaction away from the lymphocytic destruction of the hair follicle. Studies with DPCP showed 78% response rate in non-totalis/universalis, however there was a 62% relapse rate among those with regrowth. Only half of these patients that relapsed responded again to topical immunotherapy with DPCP. The response to DPCP was only 17% in patients with alopecia totalis or universalis (Wiseman MC, Shapiro J, MacDonald N, Lui H. Predictive model for immunotherapy of alopecia areata with diphencyprone. Arch Dermatol. 2001 Aug;137(8):1063-8.)
With contact immunotherapy, Dr. Shapiro recommends treating only half of the scalp initially so response to treatment can be assessed for the individual patient. If the patient tolerates DPCP on the scalp, it can be used for eyebrows as well. If there are patchy areas within regrowth that are not responding to the DPCP, Dr. Shapiro recommends the addition of intralesional steroids to target these areas specifically, as often as every 4 weeks.
Adverse events of topical immunotherapy include eczematous eruption, bullae, facial edema, lymphadenopathy, and pigmentary alterations. Dr. Shapiro advised nearly everyone has some lymphadenopathy with DPCP therapy, however he has not observed any cases of lymphoma in the patients he has treated over the decades with DPCP.
The Paradigm Shift: JAK Inhibitors
What’s new to alopecia areata? Jak kinase inhibitors, or specifically tofacitinib, which has been the JAK inhibitor that has been evaluated the most in its efficacy for alopecia areata (Kennedy Cri-spin, M, et al. Safety and efficacy of the JAK inhibitor tofacitinib citrate in patients with alopecia areata. JCI Insight. 2016 Sep 22;1(15):e89776.). This study found that in alopecia areata patients treated with tofacitinib 5mg BID, 64% had improvement in hair regrowth. Interestingly, all of the patients experienced hair loss after discontinuation on average after 8 weeks. Further, only grade I and grade II adverse events were noted in the study, demonstrating the favorable safety profile of this treatment.
Dr. Shapiro’s strategy for using tofacitinib involves dosing with tofacitinib 10-15mg total daily in conjunction with intralesional injections of corticosteroids (See Figure 1). Once a response has been obtained, he continues the lowest tofacitinib dose that continues to be effective. How does approval work for this expensive medication? Dr. Shapiro advises strong letters of medical necessity can be helpful for insurance approval as well as the support program through Pfizer called XelSource.
While there is no current cure for alopecia areata, there are treatments that can be effective for pa-tients, even those with long standing hair loss. This is an exciting time as the arsenal to treat hair loss is expanding to include a novel class of immunomodulators in addition to the tried-and-true therapies.
This information was presented by Dr. Jerry Shapiro at the 2021 ODAC Virtual Conference held on January 14-17, 2021. The above highlights from his lecture were written and compiled by Dr. Edita Newton, third-year dermatology resident at the University of Arkansas for Medical Sciences.
Did you enjoy this article? Find more on Medical Dermatology here.