EPI Health has graciously supported the COVID-19 News and Resource Center.
I, along with dermatology residents and dermatologists all over the country, have been watching the world leaders in our field as they try to keep a finger on the ever-changing pulse of the COVID-19 pandemic. For the dermatologist, we have either been forced into a technological world we had not yet fully embraced or we have been pulled back into the world of general medicine that we thought we had left behind.
This post will include highlights of information shared 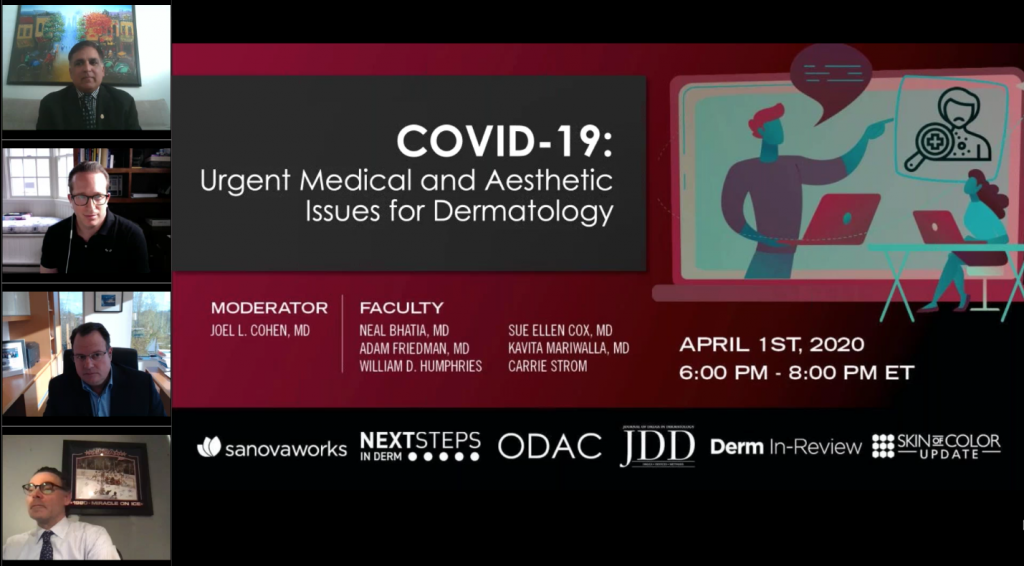 during part 1 of “COVID-19: Urgent Medical and Aesthetic Issues for Dermatology”, a special edition webinar hosted by the Journal of Drugs in Dermatology in partnership with Next Steps in Derm and SanovaWorks. The webinar was moderated by Joel L. Cohen, MD, Director of About Skin Dermatology and Associate Clinical Professor at the University of California at Irvine, and a panel of experts including Neal Bhatia, MD, Director of Clinical Dermatology, Therapeutics Clinical Research, Adam Friedman, MD, Professor and Interim Chair of Dermatology at George Washington School of Medicine & Health Sciences, and William D. Humphries, President of Ortho Dermatologics. The topics discussed give an overview of the following:
during part 1 of “COVID-19: Urgent Medical and Aesthetic Issues for Dermatology”, a special edition webinar hosted by the Journal of Drugs in Dermatology in partnership with Next Steps in Derm and SanovaWorks. The webinar was moderated by Joel L. Cohen, MD, Director of About Skin Dermatology and Associate Clinical Professor at the University of California at Irvine, and a panel of experts including Neal Bhatia, MD, Director of Clinical Dermatology, Therapeutics Clinical Research, Adam Friedman, MD, Professor and Interim Chair of Dermatology at George Washington School of Medicine & Health Sciences, and William D. Humphries, President of Ortho Dermatologics. The topics discussed give an overview of the following:
-
- Operating in a dermatologic practice with social distancing and telemedicine
- Who do we see in the office?
- Evolving medication management for dermatologists
- Dermatology training for residents during the pandemic
- Where do we go from here?
Perhaps the most telling opening statement made was by Dr. Adam Friedman when he prefaced everything by saying, “I do the best physical exam possible.” The practice of dermatology is a shadow of what it was months ago. In lieu of seeing patients in the office, we are seeing them on a screen to protect everyone from a potentially fatal virus. Dermatologists across the country are trying to decipher complicated rashes on a 4.7-inch phone or computer monitor while trying to figure out what to do with our hands. We can longer use palpation to help gauge the substance and depth of the lesion, we cannot tell if that scale is firm and adherent or just a flake of dandruff. We cannot take a step back to see if that mole is an “ugly duckling” or just a dark mole in a field of dark ducks. And, the logistics of performing the physical exam pales in comparison to the technical aspects of the teledermatology visit or even getting reimbursed for it.
Teledermatology: How to make it count
-
- Teledermatology encounters must be documented as a telehealth visit and as a place of service
- Teledermatology may now be used for both new and established patients
- Modifiers must be used
- Billing is based on the length of the encounter
- Teledermatology encounters must be documented as a telehealth visit and as a place of service
Dr. Friedman provided a basic structure for billing through medicare. For these non-face-to-face visits, the billing code is based on multiple factors. These include time spent in the visit, if the teledermatology service was synchronous (i.e., communicating in real-time) or asynchronous, as well as whether audio or both audio and images were provided. In addition to the coding for the primary encounter, a modifier must be added. A frequently updated guide can be found through the American Academy of Dermatology and a link is provided in the references below.1
Who might we need to see in the office and how do we keep them safe?
Although the National Comprehensive Cancer Network (NCCN) has recommendations for the delay of definitive treatment for most non-melanoma skin cancers2 and cutaneous melanomas of any depth with negative margins after biopsy,3 some of the panelists are uncomfortable with the idea of delaying treatment and patients may be uncomfortable as well. The guidelines do acknowledge consideration for excising tumors with risks for debilitating progression or metastasis weighed against the risk of contracting COVID-19.2
In addition to patients who already have diagnosed skin cancer needing definitive treatment, patients with new lesions may need more than an examination via a video platform. Panelists acknowledged a need for patients to be physically present in the clinic to obtain a more accurate assessment of a rash or potential neoplasm.
For patients who are seen in the office, all possible precautions should be employed. In Dr. Friedman’s clinic, “everyone is wearing a mask,” and “appointments are spaced 30 minutes apart.” In Dr. Bhatia’s clinic, staff members and patients are screened for fevers and wait in their cars until it is their turn to be seen. Dermatologists need to selectively and deliberately fulfill their role in caring for their patient’s skin.
Evolving drug therapy in dermatology
“If it’s something that doesn’t require close follow up, there’s no need to be sticklers about (it).” Dr. Friedman spoke about ensuring patients get routine medications such as ketoconazole shampoo while minimizing the burden on the patient.
For patients on biologics and other systemic agents, the data is not available for definitive instruction about their use during the COVID-19 outbreak. In an effort to keep patients out of the emergency room, the more significant risk may be a patient’s disease flaring from stopping a medication. “I really have no intention of taking people off of biologics, especially downstream blockers,” said Dr. Friedman. Although not considered immunosuppressive, Dr. Bhatia highlighted spironolactone and its role in the renin-aldosterone-angiotensin pathway, and just days following this panelist discussion, more new information has been published. As. Dr. Friedman prefaced the discussion, “this could (all) be outdated tomorrow.
Dermatologists have a long history with hydroxychloroquine use. Along with that comes familiarity with some of the most notable adverse events, such as ocular toxicity. This outcome occurs after chronic use of the medication, and when considering the short-term use in patients with COVID-19, this adverse event may not even be relevant. However, other adverse events, such as cardiac arrhythmias, may be more germane. Another concern is that patients who are already on hydroxychloroquine for lupus or other autoimmune conditions may have trouble filling their prescriptions. Mr. Humphries highlighted the industry’s role, stating that multiple companies have adapted by switching supply chains to make hand sanitizer, azithromycin, or hydroxychloroquine and donating these necessities to meet the growing demand. Once industry ramps up production, hopefully we can ‘have our cake and eat it too,” whereby we can use medications experimentally and continue to supply our patients that need these medications for a previous indication.
Dermatologists in training
Because dermatology residents are closer to their years of medical training, they are being pulled to help care for patients with COVID-19. Concerns about this involve both the dermatology resident’s role in caring for these non-dermatologic patients as well as an interruption in their training.
The panel spoke to concerns that dermatology residents may be pulled into the emergency department, intensive care unit, or other settings but assured trainees that they will always have appropriate supervision or support to allow dermatology residents to work at the highest level possible without hurting themselves or others.
For dermatology residents not on the front lines, they may find that the flow of patients seen in dermatology clinics has slowed or even stopped. Dr. Friedman highlights that a silver lining is that by being forced to embrace virtual didactics and telemedicine, these can continue to be used in the future to enhance education down the road. Although no one knows what the dermatology resident’s role may be tomorrow or a month from now, a concluding message from Dr. Friedman for the residents and dermatologists was:
Where do we go from here?
Building off of some concerns of dermatologists and other specialists who do not regularly care for the acute patient, Dr. Bhatia considered that “…we have to worry about the other side of this. Are we going to start seeing the lawyers (with messages stating) ‘were you hurt by a doctor who wasn’t trained when you had coronavirus?’” These things may not seem important now, but we need to be aware of this for the future. While no answer was provided, and no one knows what the future holds, Dr. Bhatia then shifted attention back to the field of dermatology. He emphatically stated:
As medicine moves forward in a world with COVID-19, so must dermatologists. We must ensure that our patients are still being seen in a judicious manner, are able to get efficacious and safe medications, and eventually are being seen in person to optimize their care. What this looks like, we do not yet know, but as always, innovative dermatologists will always be taking care of their patients.
Stay tuned for highlights of part 2 of this webinar, where Sue Ellen Cox, MD, Founder of Aesthetic Solutions, Kavita Mariwalla, MD, Founder of Mariwalla Dermatology, and Carrie Strom, Senior Vice President, US Medical Aesthetics at Allergan answer questions and provide guidance on aesthetic dermatology during the Covid-19 pandemic.
References:
-
- Practice management center: Dermatology code quick reference. https://assets.ctfassets.net/1ny4yoiyrqia/2xS4GaUJOr4esym0nH0r5w/ba2110cc858f3439b4ff4d99d9239aa2/Telederm-QuickReference-rev040120.pdf. April 1, 2020. Accessed April 24th, 2020.
- Advisory Statement for Non-Melanoma Skin Cancer Care During the COVID-19 Pandemic. https://www.nccn.org/covid-19/pdf/NCCN-NMSC.pdf. Version 2: March 30, 2020. Accessed April 18th, 2020.
- Short-Term Recommendations for Cutaneous Melanoma Management During COVID-19 Pandemic. https://www.nccn.org/covid-19/pdf/Melanoma.pdf. Version 2 March 25, 2020. Accessed April 18th, 2020.
- Did you enjoy this article? Find more on Covid-19 here.