Hair loss is a common yet complex condition that presents a significant challenge for both patients and dermatologists alike. Accurate diagnosis and effective management often require a meticulous and nuanced approach that enables the physician to discern subtle clues that distinguish between various etiologic forms of alopecia. At the 2025 Orlando Dermatology, Aesthetic, and Surgical Conference, Dr. Ronda Farah, a seasoned cosmetic dermatologist and hair loss specialist from the University of Minnesota Medical School, shared her expertise on this subject, emphasizing the critical steps in her approach to evaluating hair loss, while also highlighting clinical pearls derived from case presentations.
Initial Clinical Examination:
In the exam room, the first few moments spent with a hair loss patient are crucial to establishing a strong therapeutic alliance and building a differential diagnosis to guide further evaluation. Optimizing this encounter requires a thoughtful systematic approach to the physical exam that not only narrows down potential diagnoses swiftly, but also reassures the patient that they are receiving attentive care. With these goals in mind, Dr. Farah shared her prioritized checklist of high yield clinical findings across four key sites, affectionately termed her “top ten things to check within the first minute” of a clinical encounter. These sites include the:
-
- Scalp: Look for ①erythema, ②follicular-based papules, ③pustules, ④scale and ⑤loss of follicular ostia while assessing for ⑥thinning in a recognizable pattern. Also, check for ⑦tenderness to palpation. These signs can provide insights into current disease activity and help differentiate between scarring and nonscarring hair loss processes.
- Hair Shaft: Check for ⑧signs of chemical or heat processing damage such as hair shaft breakage. An intrinsic hair loss disorder can be compounded by external factors too.
- Nails: Identify clues such as ⑨pitting, trachonychia or dorsal pterygium that may be indicative of certain alopecic processes such as alopecia areata or lichen planopilaris.
- Eyebrows: Search for evidence of ⑩patchy loss or absence of eyebrows, which might signal conditions such as alopecia areata or frontal fibrosing alopecia (FFA).
Beyond the physical exam, there are several adjunctive tools and maneuvers that can facilitate the diagnosis and monitoring of alopecic processes. Chief amongst these is photodocumentation. Dr. Farah strongly advocates for obtaining a standardized photo series of hair loss patients to document clinical course and aid in the evaluation of treatment efficacy. Her standard photo series consists of 8 global images highlighting the frontal hairline, middle part, bilateral temporal hairline and nails, but additional views may be obtained per provider preference. Additional non-invasive diagnostics include:
-
- Hair pull test: This test involves gently pulling on 50-60 hair fibers from various areas of the scalp at a time, with the extent of hair loss is assessed by the number of hairs that come out. A positive hair pull test, indicated by more than five or six strands falling out, suggests an active hair loss process such as acute or chronic telogen effluvium.
- Hair tug test: This test is conducted by holding a group of 50-60 hairs between the thumb and forefinger of one hand and gently pulling the distal ends with the other hand. Any hair breakage is considered abnormal and indicative of hair fragility, which may suggest a component of external processing factors such as heat or chemicals.
- Hair mounts: This technique entails microscopic examination of the hair bulb and hair shaft by placing epilated hair roots on a glass slide, adding mounting medium and covering the specimen with a coverslip for light microscopy. This test is particularly helpful in identifying structural abnormalities in the hair shaft and determining the stage of the hair cycle based on the appearance of the hair root.
- Trichoscopy: This technique employs the application of dermoscopy to the hair and scalp, allowing for more detailed visualization of morphologic structures associated with the hair shaft, follicle and surrounding skin. This technique is particularly quick and instructive in discerning between scarring and non-scarring alopecic processes.
Taken together, these non-invasive diagnostic approaches can aid the astute physician in arriving at an accurate diagnosis. In the setting of a more complex presentation, a scalp punch biopsy can also provide profound diagnostic insights that can inform further management.
Clinical Pearls from Real Cases:
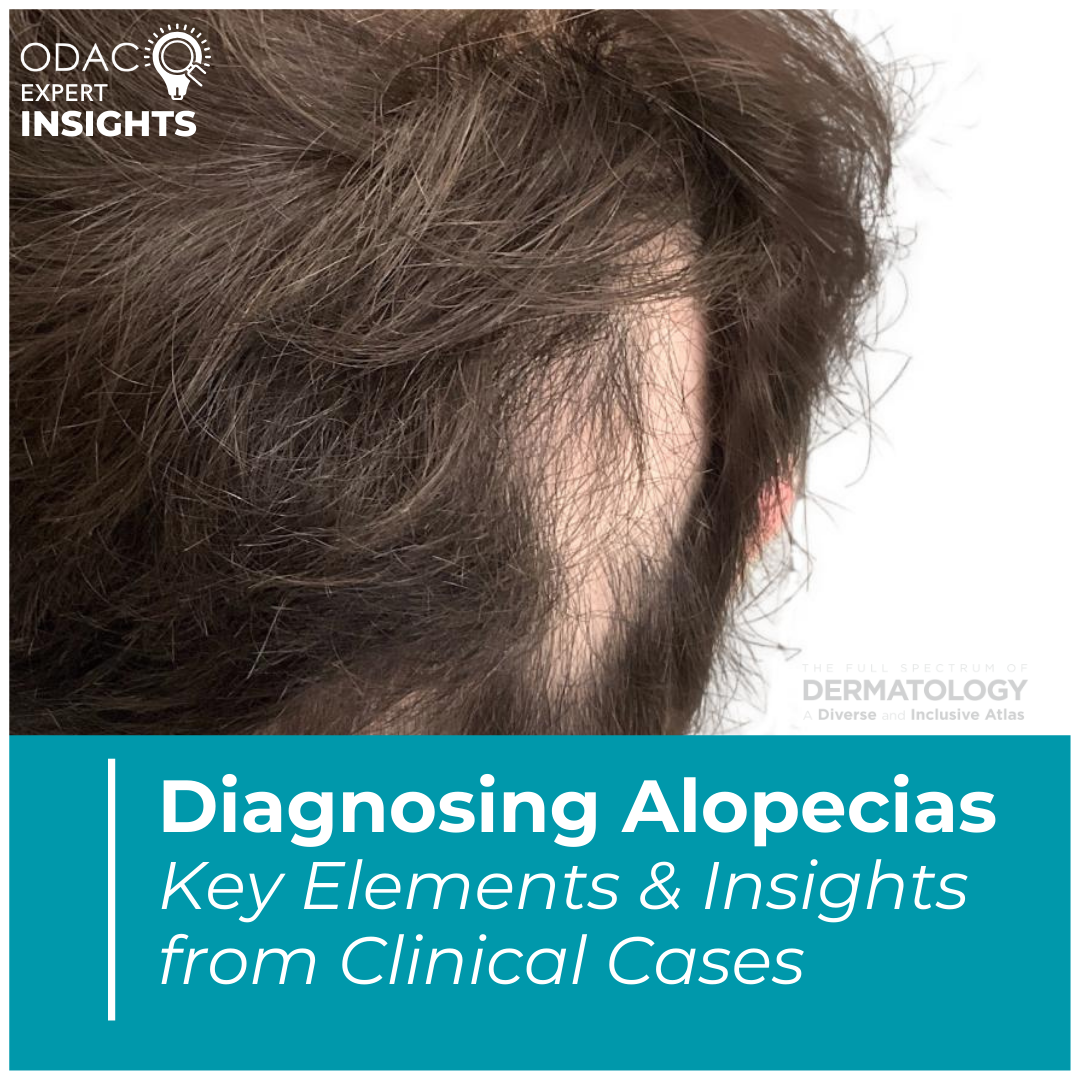
Examine the whole scalp for your patients. While a particular patch of hair loss may be especially distressing to a patient, an appropriate assessment requires complete evaluation of the whole scalp. An alopecic patch behind the ear, for example, could be secondary to ophiasis-pattern alopecia areata, trichotillomania, or frontal fibrosing alopecia (FFA); only a complete, thorough evaluation will discern between these diagnoses. A telltale sign of trichotillomania is broken hair shafts, whereas alopecia areata shows characteristic yellow dots and exclamation point hairs on trichoscopy, along with hypopigmented vellus hairs on hair regrowth1. FFA classically manifests as a progressive, symmetric band-like zone of hair loss along the anterior hairline that can become circumferential if left untreated.
Androgenetic alopecia can look like central centrifugal cicatricial alopecia. Androgenetic alopecia often presents as patterned thinning over the vertex scalp, which on quick glance can look similar in appearance to central centrifugal cicatricial alopecia (CCCA). This poses a potential diagnostic pitfall for the provider that can misdirect initial management. To mitigate against misdiagnosis, a combination of careful history-taking and the use of adjunctive diagnostic tools such as trichoscopy and scalp biopsy is recommended. In androgenetic alopecia, frontal hairline involvement and follicular miniaturization are very helpful clues to the diagnosis. In CCCA, peripilar white-gray halos and large interfollicular distances are good diagnostic indicators on trichoscopy1.
Central centrifugal cicatricial alopecia carries comorbidities. There is a genetic component to CCCA, with loss-of-function mutations in PADI3 playing a pathogenic role in this disease process2. Additionally, fibroproliferative gene signatures are upregulated in CCCA, with possible comorbid clinical correlates of type 2 diabetes, uterine leiomyomas and breast cancer3-5. While further research into the mechanisms underlying these associations is warranted, referral for further screening of these comorbidities is prudent.
Frontal fibrosing alopecia affects more than the scalp. FFA is characterized by hairline recession with perifollicular erythema and scale, hyperkeratosis, and absence of vellus hairs both macroscopically and on trichoscopy. Additional diagnostic features include thinning or absent eyebrows, facial papules, and possible evidence of mucocutaneous lichen planus. Altogether, these features help distinguish FFA from traction alopecia, which at early stages may be a diagnostic confounder. Emerging literature is also drawing attention to the depression of frontal veins as a potential clinical sign of FFA6,7. For this reason, photographic documentation at the initial office visit is essential as in-office treatment side effects (e.g. intralesional steroid injection) may may overlap with this feature.
Conscientious cosmetic interventions can uplift more than skin in hair loss patients. Hair loss often carries significant stigma for patients, prompting increasing interest in cosmetic interventions, particularly facial rejuvenation. While alopecia is not a contraindication for any cosmetic procedure, care should be exercised in the use of resurfacing modalities in FFA patients given known defects in their wound healing response. Ablative lasers such as the erbium 2940-nm laser and deep chemical peels, for example, may raise concern for scarring in patients with active disease8,9. In contrast, non-ablative Nd:YAG laser is a viable option for management of facial papules in FFA, while oral isotretinoin is a non-invasive alternative10,11. Careful placement of dermal filler and neurotoxin can also help offset aesthetic features accentuated by alopecic processes, such as forehead heaviness. Of note, there are a few rare reports of dermal filler-induced alopecia, so caution and close monitoring is recommended when using filler products near the hairline12.
Overall, accurately diagnosing alopecias relies on a structured and systematic approach to patient examination that incorporates close inspection of the scalp, hair shaft, nails and eyebrows. The clinical pearls shared by Dr. Farah underscore the nuances of different hair loss presentations, emphasizing the need for thinking about patients wholistically in their evaluation and management. In cases where initial clinical assessment is inconclusive, the use of adjunctive tools such as hair mounts, trichoscopy and biopsy are extremely helpful in elucidating a diagnosis. Building proficiency in these approaches will not help the clinician make swift and accurate diagnoses, but also will lead to better patient outcomes and satisfaction.
References
-
- Pirmez R. The dermatoscope in the hair clinic: Trichoscopy of scarring and nonscarring alopecia. J Am Acad Dermatol. Aug 2023;89(2s):S9-s15. doi:10.1016/j.jaad.2023.04.033
- Malki L, Sarig O, Romano MT, et al. Variant PADI3 in Central Centrifugal Cicatricial Alopecia. N Engl J Med. Feb 28 2019;380(9):833-841. doi:10.1056/NEJMoa1816614
- Aguh C, Dina Y, Talbot CC, Jr., Garza L. Fibroproliferative genes are preferentially expressed in central centrifugal cicatricial alopecia. J Am Acad Dermatol. Nov 2018;79(5):904-912.e1. doi:10.1016/j.jaad.2018.05.1257
- Dina Y, Okoye GA, Aguh C. Association of Uterine Leiomyomas With Central Centrifugal Cicatricial Alopecia. JAMA Dermatol. Feb 1 2018;154(2):213-214. doi:10.1001/jamadermatol.2017.5163
- Green M, Feschuk A, Valdebran M. Risk factors and comorbidities associated with central centrifugal cicatricial alopecia. Int J Womens Dermatol. Oct 2023;9(3):e108. doi:10.1097/jw9.0000000000000108
- Vañó-Galván S, Rodrigues-Barata AR, Urech M, et al. Depression of the frontal veins: A new clinical sign of frontal fibrosing alopecia. J Am Acad Dermatol. Jun 2015;72(6):1087-8. doi:10.1016/j.jaad.2015.02.1129
- Sechi A, Li JN, Tosti A. Beyond the forehead: nuchal papules and ectatic veins in frontal fibrosing alopecia. Int J Dermatol. Oct 14 2024;doi:10.1111/ijd.17521
- Sun C, Lim D, Bekhor P. Extensive facial scarring after ablative laser resurfacing in a patient with frontal fibrosing alopecia. JAAD Case Rep. May 2022;23:123-127. doi:10.1016/j.jdcr.2022.03.024
- Landau M, Tosti A, Kroumpouzos G, Eims E, Goldust M. Frontal fibrosing alopecia-A new absolute contraindication for deep chemical peels. Clin Dermatol. Nov-Dec 2024;42(6):696-700. doi:10.1016/j.clindermatol.2024.06.024
- Subash J, Eginli A, Bomar L, McMichael A. Frontal fibrosing alopecia treatment with Nd:YAG (1064 nm) nonablative laser. Int J Womens Dermatol. Jun 2021;7(3):355-356. doi:10.1016/j.ijwd.2020.10.007
- Beyzaee AM, Babaei M, Ghoreishi B, et al. Isotretinoin as a promising option in the treatment of facial papules of frontal fibrosing alopecia. Int J Dermatol. Dec 2024;63(12):1685-1690. doi:10.1111/ijd.17356
- Xie Y, Chen X, Wei A. Cosmetic filler-induced hair loss: case series and literature review. J Dermatolog Treat. Dec 15 2024;36(1):2443111. doi:10.1080/09546634.2024.2443111
This information was presented by Dr. Ronda Farah at the 2025 Annual ODAC Dermatology, Aesthetic and Surgical Conference held January 17–20, 2025 in Orlando, FL. The above highlights from her lecture were written and compiled by Damien Abreu, Chief Dermatology Resident at Washington University in St Louis. Dr. Abreu was one of the five residents selected to participate in the Young Dermatology Leader Mentorship Program sponsored by Sun Pharma and organized by Derm In-Review.