Do you feel comfortable recognizing retiform purpura and initiating the work up to identify the underlying etiology? What can cause “cellulitis” on the breast that does not get better with antibiotics? What are the most common drug culprits triggering eczematous eruptions in the elderly and stubborn psoriasis? What medication is associated with vulvovaginal pyoderma gangrenosum? If these cases strike your interest, you are in the right place.
At the ODAC 2021 Virtual Conference, Dr. Erik Stratman, MD, shared some clinical pearls regarding recognizing and diagnosing retiform purpura as well as some fascinating cases that serve as great teaching points. He challenged a dogma of dermatology, highlighting recent research that the link between systemic steroids and psoriasis flares may not be true after all.
Recognizing Retiform Purpura
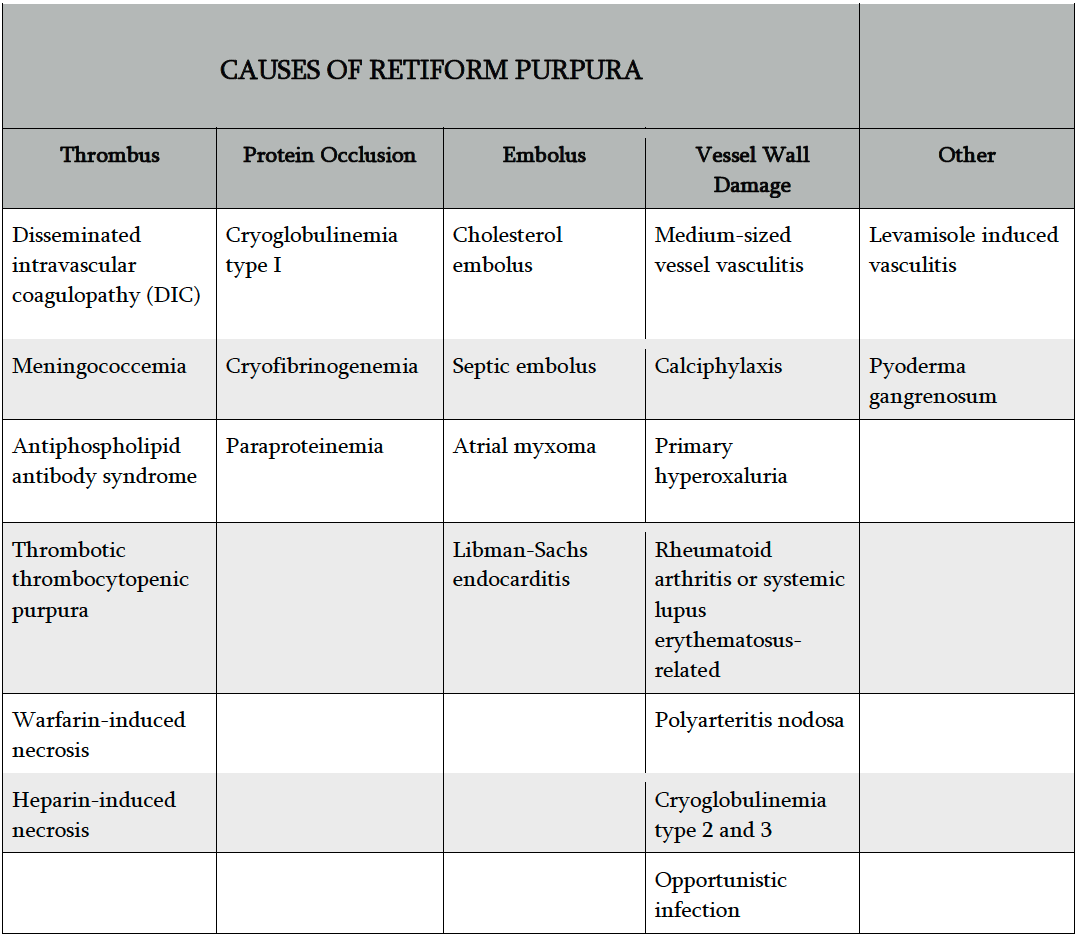
Dr. Stratman kicked off his presentation with a focus on identifying this cutaneous sign of serious systemic disease: retiform purpura. Retiform  purpura presents as angulated, non-blanching, dark red to dark purple hemorrhagic patches. Lesions may have surrounding erythema or central necrosis. Pain is common and often severe. Retiform purpura can occur in a number of different disorders (Table 1), and is different than classic palpable purpura of leukocytoclastic small vessel vasculitis. The retiform pattern results from vascular occlusion, which can be caused by thrombi, protein occlusion, emboli, or direct vessel wall damage.
purpura presents as angulated, non-blanching, dark red to dark purple hemorrhagic patches. Lesions may have surrounding erythema or central necrosis. Pain is common and often severe. Retiform purpura can occur in a number of different disorders (Table 1), and is different than classic palpable purpura of leukocytoclastic small vessel vasculitis. The retiform pattern results from vascular occlusion, which can be caused by thrombi, protein occlusion, emboli, or direct vessel wall damage.
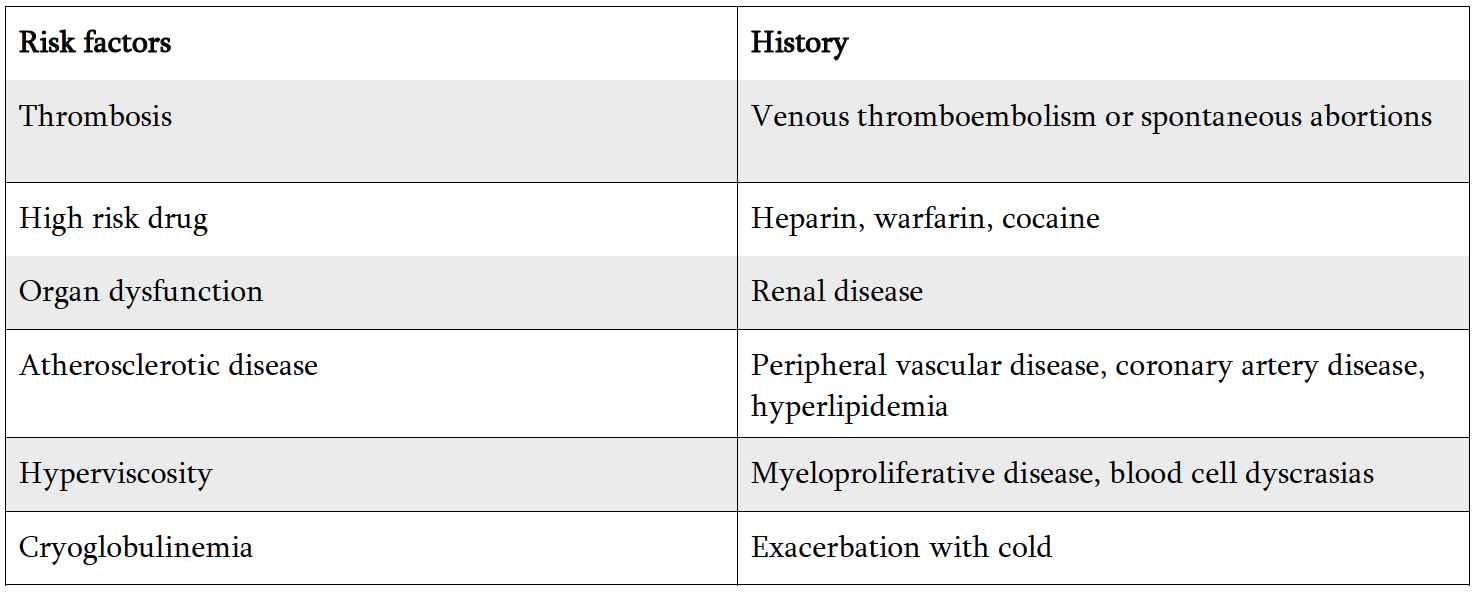
Dr. Stratman recommends taking a thorough history, detailed review of systems, and conduct a complete skin exam in cases of retiform purpura. A careful history can identify features that may be helpful to identify risk factors for vessel occlusion, such as renal disease in cases of calciphylaxis. See Table 2 for other key areas of patient history that may identify risk factors for occlusive disease presenting as retiform purpura.
What can be helpful to clue in the underlying cause on the physical exam? Location, location, location, says Dr. Stratman. For example, in fatty areas of the body such as the abdomen, thighs, and buttocks, warfarin-induced skin necrosis and calciphylaxis are common. If acral sites are predominant, think septic vasculitis, embolic disorders, cryoglobulinemia, or cryofibrinogenemia. Purpura fulminans, or widespread, extensive purpura, may occur in DIC or warfarin-induced skin necrosis. Unilateral involvement, especially involving the left leg, is frequently seen with embolic causes. Involvement of the lower extremities should clue in vasculitis, livedoid vasculopathy, cholesterol emboli, or calciphylaxis.
Collecting a skin biopsy of histology as well as tissue cultures (including bacteria, fungus, and mycobacteria, when indicated) is also critical. Specimen for histology should be collected from the advancing edge, overlapping with unaffected skin, whereas culture samples should be collected from the center of the purpura. Recommended lab workup includes complete blood count with differential, inflammatory markers, urine toxicology, blood cultures, DIC work up (D-dimer, fibrinogen, prothrombin time), and cryoglobulins.
What about retiform purpura in COVID19 infection? In one study, 10.3% of COVID-confirmed patients with skin manifestations were noted to have vascular or purpuric lesions (Jindal R, Chauhan P. Cutaneous manifestations of coronavirus disease 2019 in 458 confirmed cases: A systematic review. J Family Med Prim Care. 2020 Sep 30;9(9):4563-4569). These patients were generally older and had poor clinical outcomes.
In otherwise young, healthy patients, retiform purpura in the setting of fever and headache may represent a dermatologic emergency due to concern for meningococcemia.
Challenging cases from Dr. Stratman
-
 Itchy rash in a high school wrestler? Think about prurigo pigmentosa, also known as the “Keto rash” due to growing frequency of this rash with the popularity of the ketogenic diet. This rash responds best to a balanced diet. Triamcinolone cream and oral doxycycline can also be helpful.
Itchy rash in a high school wrestler? Think about prurigo pigmentosa, also known as the “Keto rash” due to growing frequency of this rash with the popularity of the ketogenic diet. This rash responds best to a balanced diet. Triamcinolone cream and oral doxycycline can also be helpful.
-
- Painful hardening of the skin in a dialysis patient? Yes, nephrogenic systemic fibrosis still happens, albeit rarely, these days despite the reduced risk with improved gadolinium and dialysis protocols after MRI imaging. The adoption of macrocyclic gadolinium-based contrast agents since 2007 has reduced the number of cases, however, they still happen. So be on the lookout!
- Itchy erosions on the occipital scalp? Think dermatitis herpetiformis (DH)! The scalp is commonly affected, as well as extensor surfaces and the buttocks. Lesional skin biopsy for histology and perilesional skin for DIF will be diagnostic. Be sure to screen DH patients for celiac sprue by asking questions about abdominal bloating, cramping, pain, diarrhea, or constipation, and recognize they also have significantly higher risks of thyroid disease as well.
 Painful, red rash on the breast that does not improve with antibiotics? Consider carcinoma erysipeloides. When tumor cells block lymphatic flow, cellulitis-like or stasis-like inflammation can be observed clinically. This has also been reported on the abdomen with ovarian cancer. Keep in mind that “cellulitis” that does not resolve with appropriate therapy should be considered for a biopsy to rule out a different etiology.
Painful, red rash on the breast that does not improve with antibiotics? Consider carcinoma erysipeloides. When tumor cells block lymphatic flow, cellulitis-like or stasis-like inflammation can be observed clinically. This has also been reported on the abdomen with ovarian cancer. Keep in mind that “cellulitis” that does not resolve with appropriate therapy should be considered for a biopsy to rule out a different etiology.- Where to turn when stubborn psoriasis does not improve with therapy? Review that patient’s medication list. Beta-blockers are the most strongly implicated, however, lithium, antimalarials, NSAIDs, interferon, ACE inhibitors, TNF-alpha inhibitors, terbinafine, tetracyclines, and benzodiazepines are also reported.
- What about eczematous rashes in the elderly? Dr. Stratman recommends reviewing those medication lists as well. If recalcitrant despite the dry skin care, consider working with their primary care doctor to consider a drug holiday from the calcium channel blocker for 3 months (Summers EM et al. Chronic eczematous eruptions in the aging: further support for an association with exposure to calcium channel blockers. JAMA Dermatol. 2013 Jul;149(7):814-8.)
- What medication is associated with vulvovaginal pyoderma gangrenosum? Consider rituximab as an associated medication. This can present as deep ulcerations affecting the vulva and vagina with severe pain and copious purulent drainage. While this entity is thankfully rare, Dr. Stratman expects cases may become more prevalent as rituximab use is increasing, especially in our field.
Dr. Stratman noted a common perception among dermatologists is that systemic steroids in psoriasis patients pose a great risk for causing erythrodermic or pustular psoriasis flares. To address this long-standing dogma, Dr. Stratman and his colleagues investigated this hypothesis using a retrospective chart review of hundreds of psoriasis patients exposed to systemic steroids for variable lengths of time to see if they indeed had complications with their skin disease during or immediately following tapering of the steroids. Ultimately, they found only 1.42% of patients had a flare of psoriasis after systemic steroids, suggesting this suspected risk is not evidence-based after all (Gregoire ARF, DeRuyter BK, Stratman EJ. Psoriasis Flares Following Systemic Glucocorticoid Exposure in Patients With a History of Psoriasis. JAMA Dermatol. 2020 Nov 18:e204219.)
This information was presented by Dr. Erik Stratman at the 2021 ODAC Virtual Conference held on January 14-17, 2021. The above highlights from hir lecture were written and compiled by Dr. Edita Newton, second-year dermatology resident at the University of Arkansas for Medical Sciences.
Clinical images used with permission from Erik Stratman, MD
Did you enjoy this article? Find more on medical dermatology topics here.

