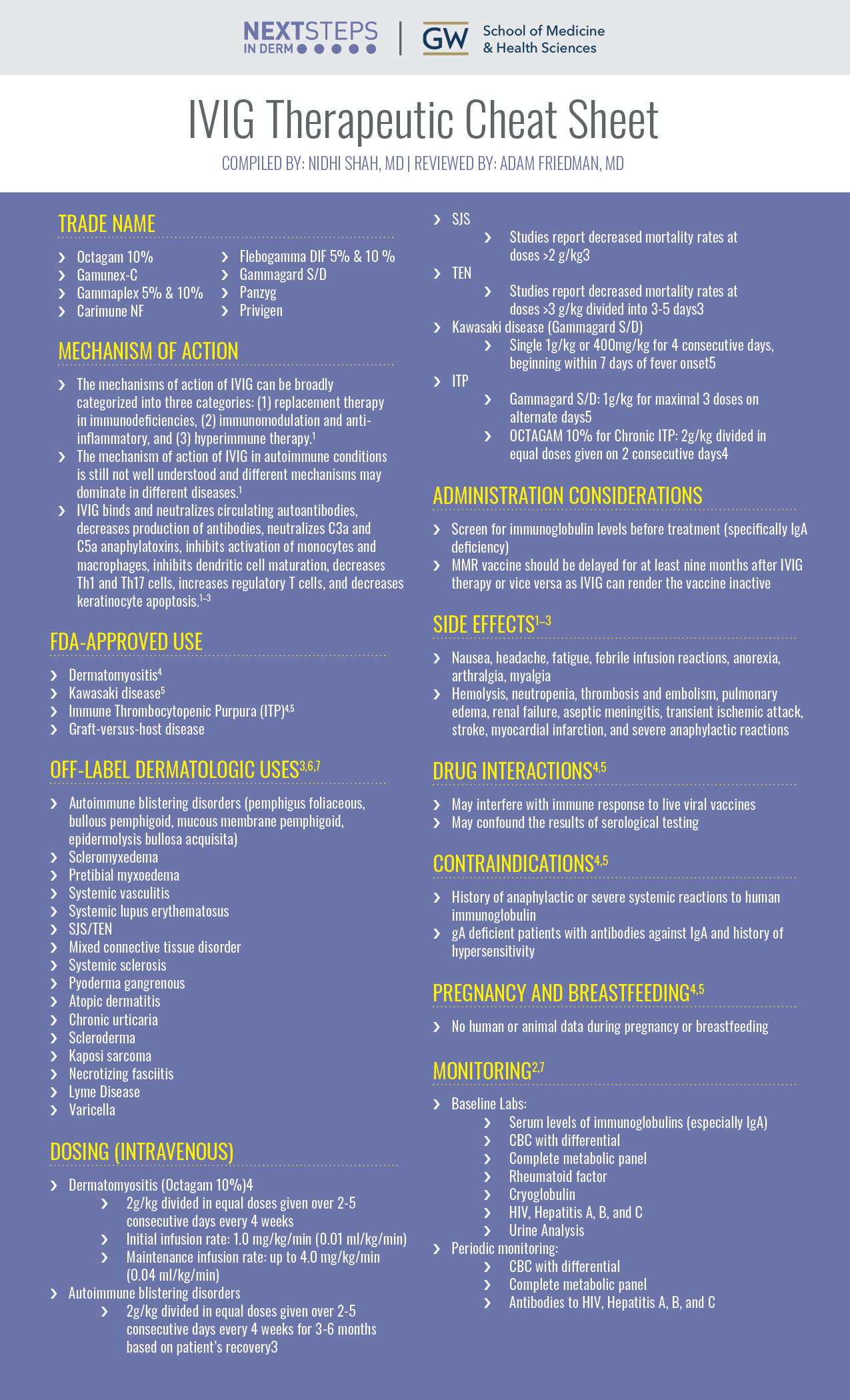
Intravenous immune globulin (IVIG) is a concentrate of pooled immunoglobulins derived from plasma donors. Its unique mechanism of action expands the utility of the medication to a variety of conditions. We continue our series, Therapeutic Cheat Sheet, with a closer look at IVIG, which is FDA-approved for the treatment of dermatologic conditions including dermatomyositis, Kawasaki disease, ITP, and acute graft-versus-host disease, and is also used off label for conditions including autoimmune blistering diseases, connective tissue diseases, SJS/TEN, and many more.
Intravenous Immune Globulin (IVIG)Therapeutic Cheat Sheet
Compiled by: Nidhi Shah, MD, Reviewed by: Adam Friedman, MD
TRADE NAME
-
- Octagam 10%
- Gamunex-C
- Gammaplex 5% & 10%
- Carimune NF
- Flebogamma DIF 5% & 10 %
- Gammagard S/D
- Panzyg
- Privigen
MECHANISM OF ACTION
-
- The mechanisms of action of IVIG can be broadly categorized into three categories: (1) replacement therapy in immunodeficiencies, (2) immunomodulation and anti-inflammatory, and (3) hyperimmune therapy.1
- The mechanism of action of IVIG in autoimmune conditions is still not well understood and different mechanisms may dominate in different diseases.1
- IVIG binds and neutralizes circulating autoantibodies, decreases production of antibodies, neutralizes C3a and C5a anaphylatoxins, inhibits activation of monocytes and macrophages, inhibits dendritic cell maturation, decreases Th1 and Th17 cells, increases regulatory T cells, and decreases keratinocyte apoptosis.1–3
FDA APPROVED FOR
-
- Dermatomyositis4
- Kawasaki disease5
- Immune Thrombocytopenic Purpura (ITP)4,5
- Graft-versus-host disease
OFF-LABEL DERMATOLOGIC USES3,6,7
-
- Autoimmune blistering disorders (pemphigus foliaceous, bullous pemphigoid, mucous membrane pemphigoid, epidermolysis bullosa acquisita)
- Scleromyxedema
- Pretibial myxoedema
- Systemic vasculitis
- Systemic lupus erythematosus
- SJS/TEN
- Mixed connective tissue disorder
- Systemic sclerosis
- Pyoderma gangrenous
- Atopic dermatitis
- Chronic urticaria
- Scleroderma
- Kaposi sarcoma
- Necrotizing fasciitis
- Lyme Disease
- Varicella
DOSING (INTRAVENOUS)
-
- Dermatomyositis (Octagam 10%)4
- 2g/kg divided in equal doses given over 2-5 consecutive days every 4 weeks
- Initial infusion rate: 1.0 mg/kg/min (0.01 ml/kg/min)
- Maintenance infusion rate: up to 4.0 mg/kg/min (0.04 ml/kg/min)
- Autoimmune blistering disorders
- 2g/kg divided in equal doses given over 2-5 consecutive days every 4 weeks for 3-6 months based on patient’s recovery3
- SJS
- Studies report decreased mortality rates at doses >2 g/kg3
- TEN
- Studies report decreased mortality rates at doses >3 g/kg divided into 3-5 days3
- Kawasaki disease (Gammagard S/D)
- Single 1g/kg or 400mg/kg for 4 consecutive days, beginning within 7 days of fever onset5
- ITP
- Gammagard S/D: 1g/kg for maximal 3 doses on alternate days5
- OCTAGAM 10% for Chronic ITP: 2g/kg divided in equal doses given on 2 consecutive days4
- Dermatomyositis (Octagam 10%)4
ADMINISTRATION CONSIDERATIONS
-
- Screen for immunoglobulin levels before treatment (specifically IgA deficiency)
- MMR vaccine should be delayed for at least nine months after IVIG therapy or vice versa as IVIG can render the vaccine inactive
SIDE EFFECTS1–3
-
- Nausea, headache, fatigue, febrile infusion reactions, anorexia, arthralgia, myalgia
- Hemolysis, neutropenia, thrombosis and embolism, pulmonary edema, renal failure, aseptic meningitis, transient ischemic attack, stroke, myocardial infarction, and severe anaphylactic reactions
DRUG INTERACTIONS4,5
-
- May interfere with immune response to live viral vaccines
- May confound the results of serological testing
CONTRAINDICATIONS4,5
-
- History of anaphylactic or severe systemic reactions to human immunoglobulin
- IgA deficient patients with antibodies against IgA and history of hypersensitivity
PREGNANCY AND BREASTFEEDING4,5
-
- No human or animal data during pregnancy or breastfeeding
MONITORING2,7
-
- Baseline Labs:
- Serum levels of immunoglobulins (especially IgA)
- CBC with differential
- Complete metabolic panel
- Rheumatoid factor
- Cryoglobulin
- HIV, Hepatitis A, B, and C
- Urine Analysis
- Periodic monitoring:
- CBC with differential
- Complete metabolic panel
- Antibodies to HIV, Hepatitis A, B, and C
- Baseline Labs:
FURTHER READING
If you would like to learn more about IVIG, check out the following articles in the Journal of Drugs in Dermatology:
Early Treatment With Nonsucrose Intravenous Immunoglobulin in a Burn Unit Reduces Toxic Epidermal Necrolysis Mortality, published in the Journal of Drugs in Dermatology
Aires, G. Fraga, R. Korentager, C. P. Richie, S. Aggarwal, J. Wick, and D. Y. Liu
Abstract
Background: Intravenous immunoglobulin (IVIG) can be used to treat potentially deadly toxic epidermal necrolysis (TEN), milder Stevens Johnson Syndrome (SJS) and intermediate TEN/SJS overlap. Some formularies now deny IVIG for TEN based on the EuroSCAR TEN/SJS study that reported a nonsignificant trend toward increased mortality in 75 IVIG-treated TEN/SJS patients; of note the IVIG patients had more TEN and less SJS than patients in other treatment arms. EuroSCAR data on mortality among the 25 IVIG-treated TEN patients, use of nonsucrose IVIG, and admission to specialized settings such as burn units was not disclosed. The impact of treatment setting (specialized unit vs general ward) on IVIG efficacy has not previously been studied.
Objective: To evaluate efficacy of treating TEN with early nonsucrose IVIG in a burn unit.
Methods: Data were retrospectively collected from 13 IVIG-treated TEN patients admitted to a burn unit over a 6-year period.
Results: We report 0% mortality among 13 IVIG-treated TEN patients. Mortality was significantly lower than predicted by SCORTEN. Mortality was also significantly lower than the EuroSCAR groups receiving IVIG (P<.005), supportive care (P<.018), and corticosteroids only (P<.046).
Conclusion: TEN patients may benefit from early nonsucrose IVIG administered in burn units or other specialized settings
J Drugs Dermatol. 2013;12(6):679-684.
Treatment of Nevirapine-Associated DRESS Syndrome with Intravenous Immune Globulin (IVIG), published in the Journal of Drugs in Dermatology
Fields, M. Petersen, E. Chiao, and P. Tristani-Firouz
Abstract
Drug rash with eosinophilia and systemic symptoms (DRESS) syndrome is an adverse drug reaction most commonly associated with aromatic antiepileptic agents. It is characterized by the triad of skin eruption, fever, and systemic involvement, with the latter usually manifesting as hepatitis and lymphadenopathy.1 Mortality is primarily due to hepatic failure and can be as high as 10%.2 Formerly referred to by names such as Dilantin hypersensitivity syndrome and anticonvulsant hypersensitivity syndrome, DRESS syndrome is a more precise term since this reaction pattern can be seen with other agents. DRESS syndrome has also been reported in association with sulfonamides, allopurinol, terbinafine, minocycline, azathioprine, and dapsone3 as well as with several antiretroviral agents such as abacavir and nevirapine.4,5 We describe a patient with HIV who developed nevirapine hypersensitivity syndrome who was successfully treated with intravenous immune globulin (IVIG).
J Drugs Dermatol. 2005;4(4):510.
REFERENCES
-
- Arumugham VB, Rayi A. Intravenous Immunoglobulin (IVIG).; 2023.
- Dhar S. Intravenous immunoglobulin in dermatology. Indian J Dermatol. 2009;54(1):77. doi:10.4103/0019-5154.48996
- Emre S. Intravenous immunoglobulin treatment: Where do dermatologists stand? Dermatol Ther. 2019;32(3). doi:10.1111/dth.12854
- Octapharma. Octagam 10% Package Insert. https://www.fda.gov/media/70911/download?attachment.
- Baxter Healthcare Corporation. Gammagard S/D Package Insert. https://www.fda.gov/media/78185/download.
- Hoffmann JHO, Enk AH. High-Dose Intravenous Immunoglobulin in Skin Autoimmune Disease. Front Immunol. 2019;10. doi:10.3389/fimmu.2019.01090
- Fernandez AP, Kerdel FA. The use of i.v. IG therapy in dermatology. Dermatol Ther. 2007;20(4):288-305. doi:10.1111/j.1529-8019.2007.00142.xv
Did you enjoy this Therapeutic Cheat Sheet? You can find more here.