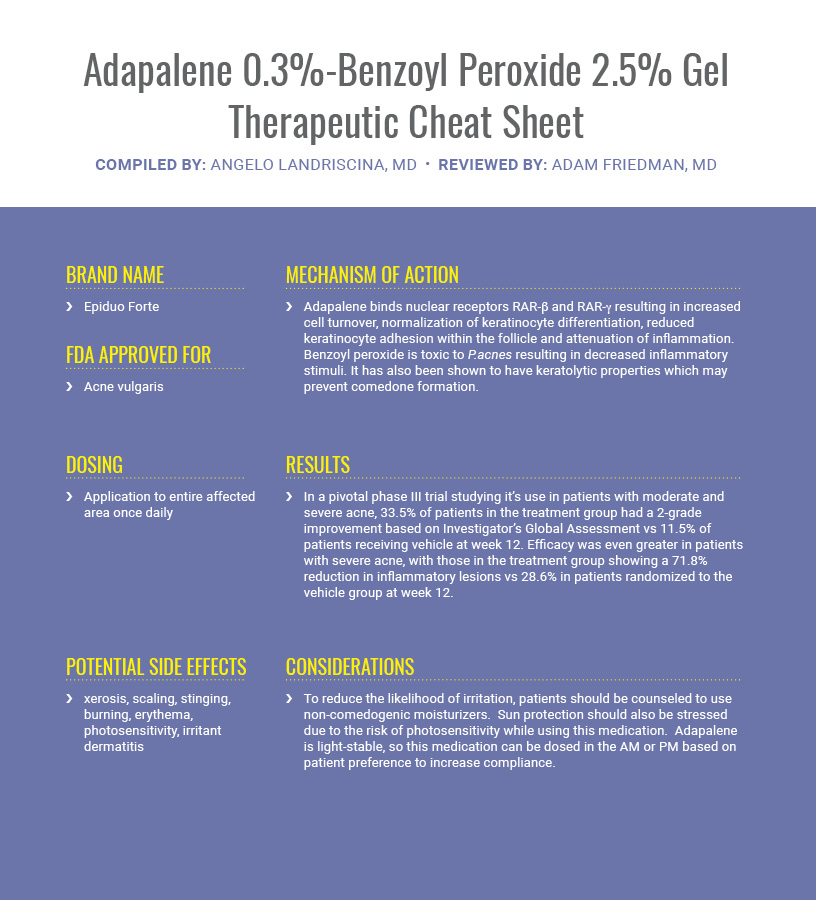
In the newest installment of our Therapeutic Cheat Sheet series, we turn to the treatment of acne. Mutli-mechanistic approaches result in improved outcomes for patients, especially when it comes to the multifactorial causes of acne. Adapalene 0.3%-benzoyl peroxide 2.5% gel (also known as Epiduo Forte) provides a useful tool for delivering two mainstays of acne therapy in one topical agent.
If you would like to read more about Adapalene 0.3%-Benzoyl Peroxide 2.5% Gel, check out the following journal articles published in the Journal of Drugs in Dermatology:
BACKGROUND: Patients with skin of color (SOC) and Fitzpatrick skin types (FST) IV–VI frequently develop acne.
OBJECTIVE: Evaluate subject-reported outcomes after treatment with adapalene 0.3%/ benzoyl peroxide 2.5% gel (0.3% A/BPO) (trade name: Epiduo Forte/adapalene and benzoyl peroxide) in subjects with SOC and moderate to severe acne vulgaris.
METHODS: This was an open-label interventional study conducted in 3 countries (Mauritius, Singapore, and USA) in subjects of Asian, Latin-American, or black/African-American ethnicity, with an Investigator’s Global Assessment (IGA) of moderate or severe facial acne (enrollment 2:1), and FST IV to VI. For 16 weeks, subjects applied 0.3% A/BPO (once daily) and utilized a skin care regimen (oil control foam wash and oil control moisturizer SPF30). Assessments included quality of life (QoL) and subject questionnaires, IGA, Investigator’s Global Assessment of Improvement (GAI), postinflammatory hyperpigmentation (PIH; if present at baseline), and safety.
RESULTS: Fifty subjects were enrolled: 20 Asians, 17 black/African-Americans, and 13 Latin-Americans. Most had FST IV (74%) or V (22%), with moderate (70%; IGA 3) or severe (30%; IGA 4) acne. At week 16, 77% of subjects were satisfied or very satisfied with treatment, 56% of subjects had an IGA of 0 or 1 (clear/almost clear), and 87% had a good to excellent improvement in GAI. QoL improved throughout the study for all subjects; subject selection of “no effect at all” of acne on QoL increased from 16% of subjects at baseline to 55% at week 16. Of those with baseline PIH (60%), all were rated very mild to moderate. By week 16, the majority (75%) had no or very mild PIH, and the mean decrease in PIH was 27%. There were no adverse events leading to study discontinuation.
CONCLUSION: Patients with SOC and moderate or severe facial acne reported high satisfaction with 0.3% A/BPO treatment and experienced good tolerability, improved QoL, treatment efficacy, and improvement in PIH.
Clinicaltrials.gov number: NCT02932267
![]() Customized Single-agent Therapy Management of Severe Inflammatory Acne: A Randomized, Double-blind, Parallel-group, Controlled Study of a New Treatment – Adapalene 0.3%-Benzoyl Peroxide 2.5% Gel
Customized Single-agent Therapy Management of Severe Inflammatory Acne: A Randomized, Double-blind, Parallel-group, Controlled Study of a New Treatment – Adapalene 0.3%-Benzoyl Peroxide 2.5% Gel
BACKGROUND: More effective therapies are needed in the specific treatment of severe inflammatory acne vulgaris.
OBJECTIVES: To demonstrate superior efficacy of adapalene 0.3%-benzoyl peroxide 2.5% gel (0.3% A/BPO) vs. vehicle, and to assess efficacy of 0.3% A/BPO vs. 0.1% A/BPO in subjects with severe inflammatory acne (Investigator’s Global Assessment [IGA] of 4) in the context of a larger trial in a moderate and severe population.
METHODS: This was a multicenter, randomized, double-blind, parallel-group, 12-week study. Subjects were randomized to receive 0.3% A/BPO, 0.1% A/BPO (benchmark) or vehicle (comparator) once daily for 12 weeks. Co-primary efficacy endpoints were success rate at week 12 (percentage of subjects rated “clear” or “almost clear,” ≥3-grade IGA improvement), and change in inflammatory (IN) and noninflammatory (NIN) lesion counts from baseline to week 12. Secondary efficacy endpoints were percent changes in IN and NIN lesion counts. Safety endpoints were incidence of adverse events (AEs) and local tolerability signs/symptoms.
RESULTS: In the severe inflammatory acne population, a total of 252 subjects were randomized with 106, 112 and 34 subjects in the 0.3% A/BPO, 0.1% A/BPO and vehicle groups, respectively, reaching a high rate of study completion (88.5%). At week 12, both 0.3% A/BPO and 0.1% A/BPO were superior to vehicle in terms of lesion count reduction. However for success rate, only 0.3% A/BPO achieved significantly greater efficacy over vehicle with a treatment difference of 20.1% (31.9% vs. 11.8%; 95% Confidence Interval (CI): [6.0%, 34.2%], P=.029), whereas 0.1% A/BPO did not (treatment difference vs. vehicle of 8.8%; P=.443). This translates to an 11% difference between active treatments in favor of 0.3% A/BPO. Also, 0.3% A/BPO was safe and well tolerated.
CONCLUSIONS: Availability of this new treatment option should allow clinicians to better customize severe inflammatory acne management, and the high-strength product provides a step-up treatment when needed.
![]() Efficacy and Safety of Adapalene 0.3%/Benzoyl Peroxide 2.5% Gel Plus Oral Doxycycline in Subjects With Severe Inflammatory Acne Who Are Candidates for Oral Isotretinoin
Efficacy and Safety of Adapalene 0.3%/Benzoyl Peroxide 2.5% Gel Plus Oral Doxycycline in Subjects With Severe Inflammatory Acne Who Are Candidates for Oral Isotretinoin
INTRODUCTION: Acne treatment guidelines suggest a combination approach with topical therapy including a topical retinoid, benzoyl peroxide and an oral antibiotic, or oral isotretinoin (OI), as first-line treatment options for severe acne vulgaris (AV). This study evaluated the efficacy and safety of a daily regimen of 0.3% adapalene and 2.5% benzoyl peroxide (0.3% A/BPO) gel and oral doxycycline 100 mg twice daily in severe (nonnodulocystic, non-conglobate) inflammatory AV.
METHODS: This was a phase 4, 12-week, single-arm, openlabel, multi-center investigational study. Subjects (males and females, 12 or older, with severe inflammatory AV, Investigator Global Assessment [IGA] 4, and less than equal to 4 nodulocystic lesions, n=186) were considered OI candidates at baseline by the investigator. OI candidacy was re-evaluated at each study visit. Efficacy endpoints included inflammatory lesion (IL) reduction (week 12), IGA success (defined as IGA 0 [Clear] or 1 [Almost Clear], weeks 4, 8, and 12), percent reduction in lesions (weeks 4, 8, and 12), and subject questionnaires (week 12). Safety assessments included adverse events (AEs) and tolerability.
RESULTS: Mean IL counts were significantly reduced from baseline to the end of the study (mean [SD]; baseline, 44.8 (21.73); week 12, 14.8 (16.11); mean percent reduction, 66.2% [30.47]; P less than .0001). By week 12, 37.1% of subjects achieved IGA Success (n=69, P less than .0001). Most subjects self-reported at least moderate improvement in AV (90.2%), and were “Satisfied” or “Very Satisfied” with the study treatment overall (83.2%). 41.9% of the subjects were no longer considered by their investigator to be OI candidates at week 4. At 12 weeks, only 19.9% were still considered OI candidates.
CONCLUSION: 0.3% A/BPO + DOX is an effective and safe treatment option for severe inflammatory AV, before starting OI treatment, or as an alternative when OI cannot be used. ClinicalTrials.gov identifier: NCT02899000
![]() Two Randomized, Double-Blind, Split-Face Studies to Compare the Irritation Potential of Two Topical Acne Fixed Combinations Over a 21-Day Treatment Period
Two Randomized, Double-Blind, Split-Face Studies to Compare the Irritation Potential of Two Topical Acne Fixed Combinations Over a 21-Day Treatment Period
Topical therapy of acne vulgaris (acne) is very common, however cutaneous tolerability can influence patient adherence, and concerns about skin irritation have lead to a number of comparative split-face studies. Advances in formulation technology have provided new fixed combinations with lower concentrations of potentially irritating ingredients without compromising efficacy. These developments now afford the opportunity to formulate fixed combinations with higher concentrations of active ingredients that may provide the greater efficacy needed in more severe disease with good tolerability.
Here, we compare the tolerability of two such developments, clindamycin-BP 3.75% gel and adapalene 0.3%-BP 2.5% gel, in healthy volunteers with no apparent facial redness or dryness over 21-days, using a split-face methodology.
Clindamycin-BP 3.75% gel was more tolerable than adapalene 0.3%-BP 2.5% gel over the duration of the two studies, with statistically significant differences in cumulative change from baseline starting as early as day 4 (stinging), day 5 (erythema, dryness, and scaling), day 6 (burning), and day 8 (itching); and in composite irritation index (stinging, erythema, dryness, scaling, burning, and itching) from day 4. Transepidermal water loss was less with clindamycin-BP 3.75% gel (statistically significant from day 8). Adverse events were twice as common with adapalene 0.3%-BP 2.5% gel.
These data suggest that clindamycin-BP 3.75% gel is likely to be better tolerated than adapalene 0.3%-BP 2.5% gel in moderate-to-severe acne.
Did you enjoy cheat sheet? You can find more here.

