Dr. Diane Thiboutot, Professor of Dermatology at The Pennsylvania State University College of Medicine, gave a practical talk at the 2022 ODAC Dermatology, Aesthetic and Surgical Conference about hormonal treatment of acne. Dr. Thiboutot discussed the hormonal work up, indications for hormonal treatment, and guidelines for choosing a therapy, including oral contraceptives.
Hormonal Workup for Acne
Firstly, when is hormonal testing indicated? The AAD defines specific populations who merit further workup:1
-
- Clinical features or history of hyperandrogenism.
- Pre-pubertal children with acne, early-onset body odor, axillary or pubic hair, accelerated growth, advanced bone age, or genital maturation.
- Growth charts and hand films for bone age are good screening tools in this population.
- Post-pubertal females with infrequent menses, hirsutism, androgenetic alopecia, infertility, polycystic ovaries, clitoromegaly, or truncal obesity.
If your patient falls in one of these categories, consider the following tests: serum dehydroepiandrosterone sulfate (DHEAS), total and free testosterone, LH/FSH ratio, and 17-hydroxyprogesterone. Importantly, for at least 6 weeks your patients need to be off oral contraceptive pills, which could mask changes in these tests. In terms of timing, you should test during your patient’s menstrual period or one week prior; this ensures that you are not testing near ovulation. Here is a guide for interpreting the results from Dr. Thiboutot’s presentation (figure 1):
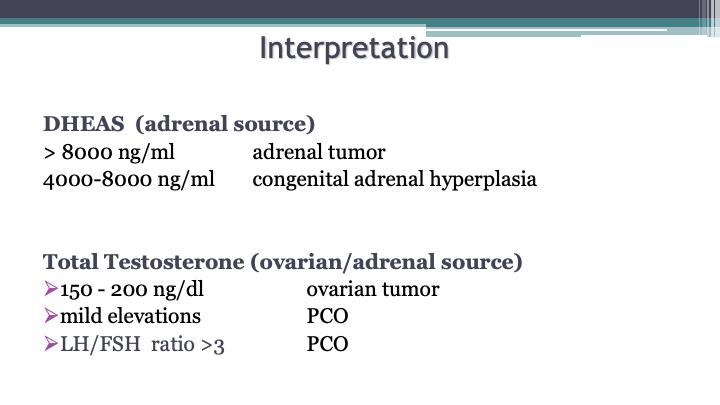
As you can see, you can use these lab results to help diagnose an adrenal tumor, congenital adrenal hyperplasia, or polycystic ovarian syndrome (PCOS). In addition to lab findings, there are other diagnostic criteria for PCOS, depending on whether your patient is an adult or adolescent. For adolescents, the diagnosis is made on clinical or biochemical hyperandrogenism with persistent oligomenorrhea. For adults, you need 2 of the 3 below criteria to make the diagnosis:
-
- Clinical or biochemical androgen excess
- Ovulatory dysfunction
- Polycystic ovaries on ultrasound
Hormonal Therapy for Acne
Hormonal treatments can be used in those with hyperandrogenism or normal serum androgens. You can consider hormonal therapy to spare patients from antibiotics or repeat courses of isotretinoin. As you can see in the algorithm in the 2016 AAD guidelines for the treatment of acne, start to think about hormonal therapies (combined oral contraceptives, COCs, or spironolactone) in female patients with moderate acne (figure 2):
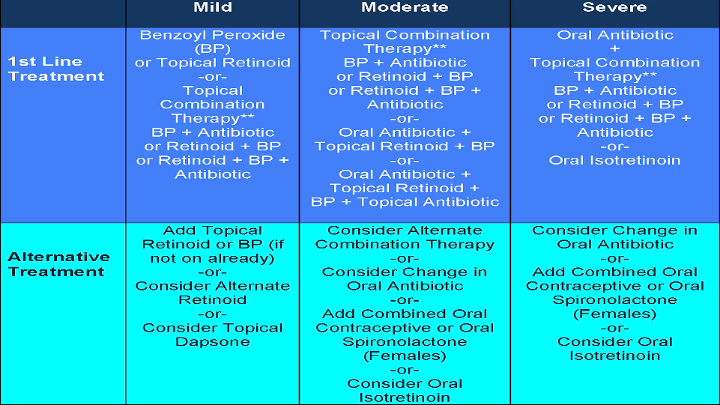
The AAD Acne guidelines state that COCs are effective for inflammatory acne and that spironolactone is useful in select patients.1 Further, the AAD recommends that for patients with adrenal hyperandrogenism, consider low-dose oral corticosteroids.1
What about the mechanisms of these therapies? COCs block ovarian production of hormones, which are made by the corpus luteum after ovulation, whereas glucocorticoids block adrenal production of hormones. Anti-androgens, including spironolactone or a new topical therapy called clascoterone, block the effects of androgens on the skin.
Combination Oral Contraceptives (COC) in Acne
Given many of us may be less comfortable with COCs, Dr. Thiboutot then took a deep dive into these therapies. As stated above, COCs block ovarian hormone production, leading to reduced serum androgens (testosterone, dihydrotestosterone, and DHEAS). Specifically for testosterone, free levels are also reduced via increased sex hormone binding globulin. COCs also function to decrease sebum production. While all COCs have efficacy for the treatment of acne by virtue of their mechanism, there are 4 FDA-approved treatments:
-
- Ortho Tricyclen® (35 μg ethinyl estradiol/norgestimate)
- Estrostep® (20-35 μg ethinyl estradiol/norethindrone acetate)
- Yaz® (20 μg ethinyl estradiol/drospirenone)
- Beyaz® (20 μg ethinyl estradiol/ drospirenone/levomefolate)
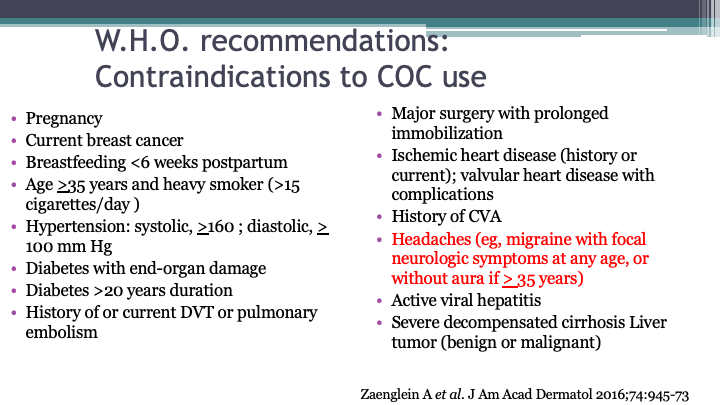
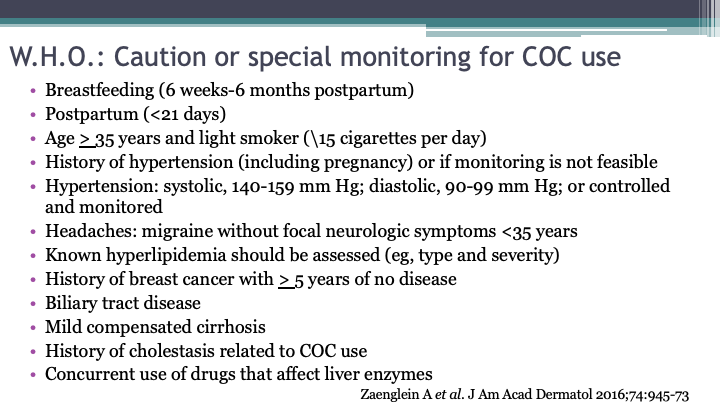
There are many contraindications to COCs, as well as scenarios that require caution or special monitoring, as you can see in Dr. Thiboutot’s slides below (figure 3 and figure 4). Be sure to obtain a thorough medical history and blood pressure before starting a COC. A less intuitive contraindication to remember is headaches with a preceding aura, or focal neurological symptom. Per an American College of Obstetrics and Gynecology Practice Bulletin, the absolute risk of stroke remains low in women with migraines, so COCs can still be considered, as long as they do not have focal neurologic signs, do not smoke, are otherwise healthy, and are younger than 35 years old.2 Regardless, it would be best to make the decision about starting a COC in a patient with migraines in consultation with an OBGYN. With proper selection of patients, you will be able to minimize risks associated with COC use.
What if you want to start a patient on both a COC and oral antibiotic? COCs can safely be used with other oral acne therapies, including tetracyclines and spironolactone. The only anti-infective agents that decrease the effectiveness of COCs are rifampin and griseofulvin.
While some providers may be concerned about the risk of thromboembolic events with COCs, the risk remains lower than that during pregnancy and the postpartum period. Further, there are some epidemiologic studies showing that the risk of blood clots is actually due to drospirenone-containing pills. Regardless, as mentioned above, proper patient selection is key and will minimize side effects, including serious ones like blood clots.
Spironolactone
In addition to COCs, spironolactone is another commonly used hormonal therapy. This medication blocks the androgen receptor and 5α-reductase, which converts testosterone to dihydrotestosterone. Spironolactone is used in doses of 25-100 milligram twice daily. Common side effects include breast tenderness and menstrual irregularity. Women with lower blood pressures can also experience dizziness, so it is important to remind patients to maintain proper hydration. Women must also avoid pregnancy given that in the later stages of pregnancy, spironolactone can inhibit the development of genitalia in male fetuses.
Spironolactone also carries of block box warning that it is a tumorigen in rat studies. However, this warning is based on animal studies alone and doses that were 10 times higher than those used in humans. As for human data, a 2013 study used a large Danish database to examine the association of breast, uterine, and ovarian cancers with spironolactone.3 The authors concluded that the use of spironolactone in women did not increase the risk of these cancers.3
As for the effectiveness of long-term spironolactone, a recent study looked at 403 females who used spironolactone for a mean of 470 days, either with a topical retinoid, oral antibiotic, or COC.4 At least 70% of participants improved or cleared their acne (face, chest, and back).4 A smaller study of adolescent females showed similar results, with 80% of patients experiencing improvement in their acne with spironolactone.5
Finally, for monitoring while on spironolactone, Dr. Thiboutot concluded that monitoring is not needed in young, healthy women. A large study of over 974 young, healthy women on spironolactone for acne found that the rate of hyperkalemia was equivalent to the baseline rate in this population.6
Conclusion
Dr. Thiboutot concluded her lecture with short, practical pearls to remember when treating women with acne. Hormonal therapy has many benefits for women with acne – it is best used as one part of the treatment regimen. In particular, consider hormonal therapy as an alternative to antibiotics. Hormonal therapy can also facilitate the transition to isotretinoin. With this lecture, we should all now have the knowledge needed to choose the best hormonal therapy at the proper dose, and to monitor patients appropriately. For spironolactone in particular, in young, healthy patients, monitoring should not include checking potassium levels as the rates of hyperkalemia are not higher than baseline in this population!
References
-
- Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74(5):945-973.e33. doi:10.1016/j.jaad.2015.12.037
- ACOG Committee on Practice Bulletins-Gynecology. ACOG practice bulletin. No. 73: Use of hormonal contraception in women with coexisting medical conditions. Obstet Gynecol. 2006;107(6):1453-1472. doi:10.1097/00006250-200606000-00055
- Biggar RJ, Andersen EW, Wohlfahrt J, Melbye M. Spironolactone use and the risk of breast and gynecologic cancers. Cancer Epidemiol. 2013;37(6):870-875. doi:10.1016/j.canep.2013.10.004
- Garg V, Choi JK, James WD, Barbieri JS. Long-term use of spironolactone for acne in women: A case series of 403 patients. J Am Acad Dermatol. 2021;84(5):1348-1355. doi:10.1016/j.jaad.2020.12.071
- Roberts EE, Nowsheen S, Davis DMR, Hand JL, Tollefson MM, Wetter DA. Use of spironolactone to treat acne in adolescent females. Pediatr Dermatol. 2021;38(1):72-76. doi:10.1111/pde.14391
- Plovanich M, Weng QY, Mostaghimi A. Low Usefulness of Potassium Monitoring Among Healthy Young Women Taking Spironolactone for Acne. JAMA Dermatol. 2015;151(9):941-944. doi:10.1001/jamadermatol.2015.34
This information was presented by Dr. Diane Thiboutot at the 2022 ODAC Dermatology, Aesthetic and Surgical Conference held January 14-17, 2022. The above highlights from her lecture were written and compiled by Dr. Emily Murphy.
Did you enjoy this article? You can find more on Medical Dermatology here.