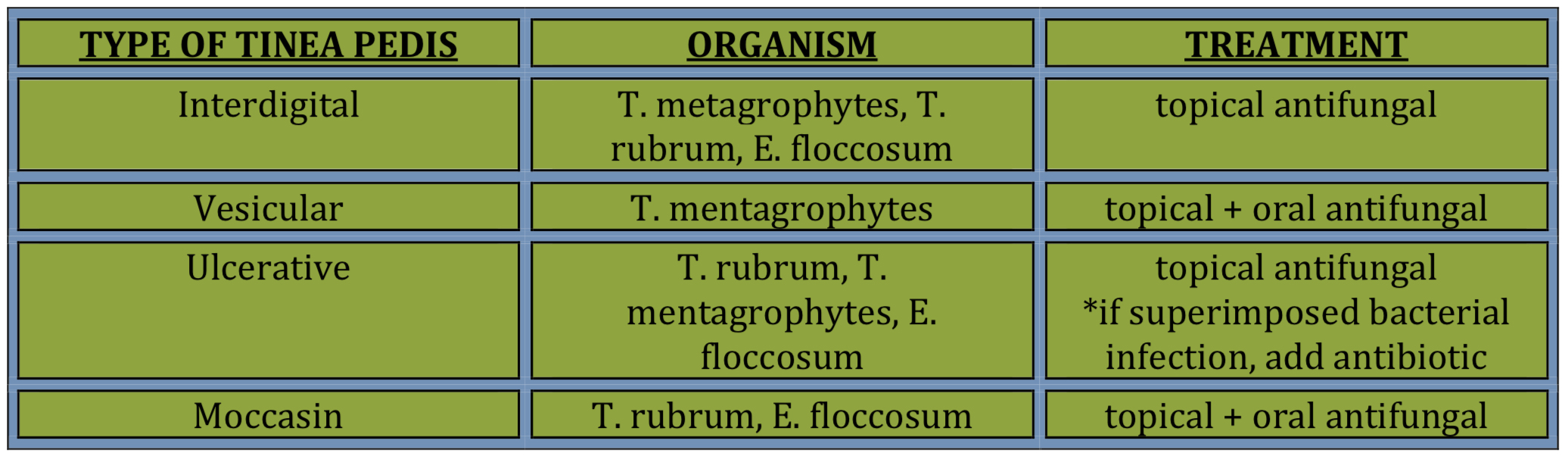
Topicals- (appropriate for toe web spaces); use for 2-4 weeks OR 1 week after scale gone
Azoles are fungistatic (ex: Econazole, etc)
Allylamines are fungistatic/fungicidal (ex: Terbinafine, Naftifine) Antifungal power/sprays to shoes weekly
**newer additions: Luliconazole 1% cream- Use for 2 weeks Naftifine 2% gel and cream
Tinea Capitis
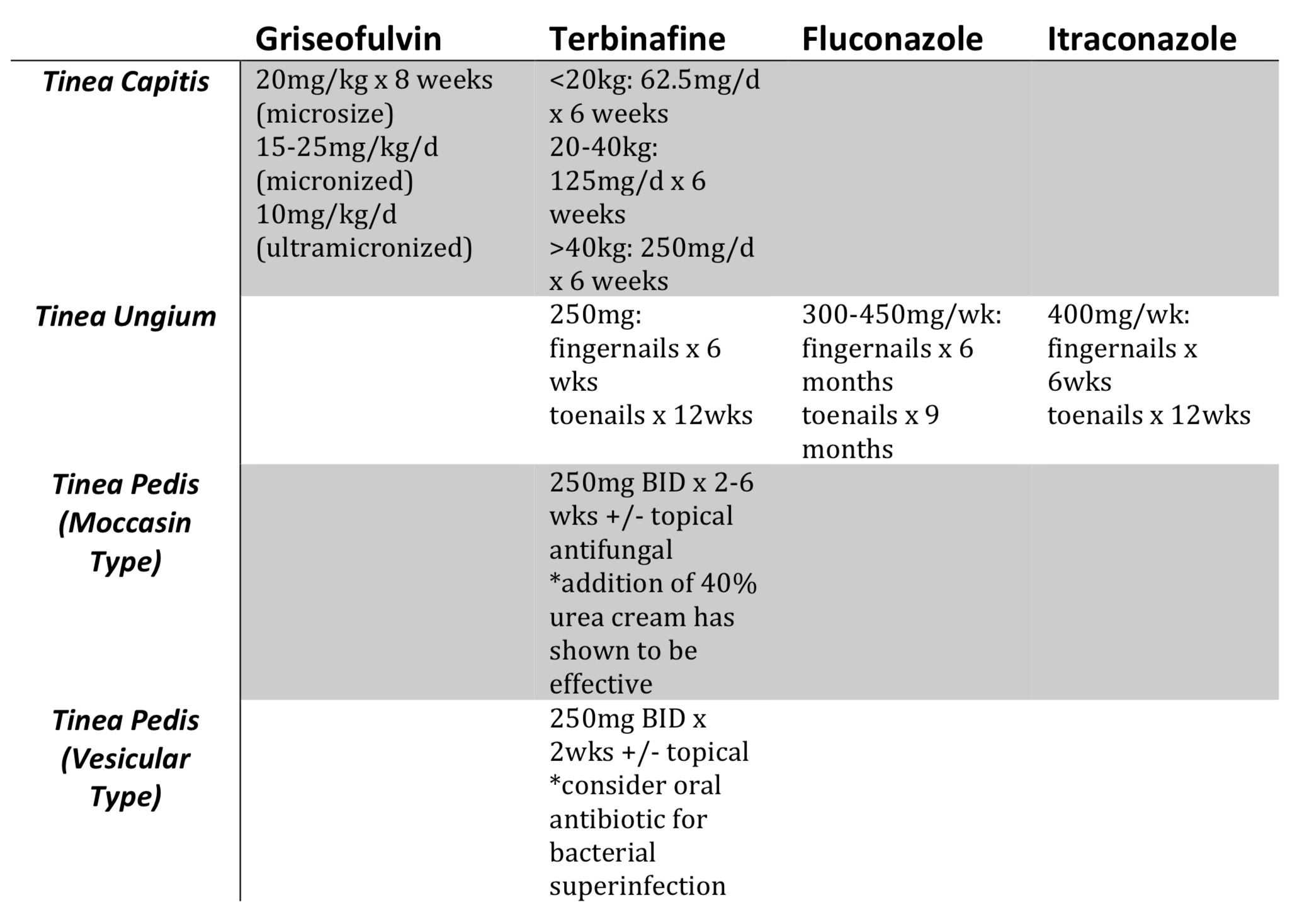
**IMPORTANT – Systemic treatment is required!
TIPS:
Terbinafine > Griseofulvin for T.rubrum, not M. canis
Ketoconazole 2% shampoo used as a 5 mins soak then rinse
Re-culture at 1 month
As a 1st year dermatology resident, one of the most frustrating patient encounters I have is a patient with onychomycosis. I find it very difficult to effectively treat this disorder to the satisfaction of some patients.
So what does onychomycosis mean? It is a term use to encompass ALL fungal infections of the nail (dermatophytes and nondermatophytes) in comparison to tinea unguium, which refers to dermatophyte infections of the nail unit. Now, let’s review.
- T.rubrum, T. mentagrophytes, E. floccosum
- 50% of nail dystrophy due to onychomycosis
- Other risk factors: Risk factors: age, DM, HIV, PVD, sports, trauma nail disorders
- 90% of onychomycosis is tinea unguium
- **ALWAYS look for coinciding tinea pedis!
4 patterns:
1. Distal lateral subungal onychomycosis – invasion via hyponychium
a. T. rubrum
2. Proximal subungal onychomycosis – direct invasion via proximal nail fold
a. Immunocompromised patients
b. T. rubrum
3. Proximal white subungal onychomycosis
a. Marker of AIDS
b. T. rubrum
4. White superficial onychomycosis – direct invasion via superficial nail plate
a. T. mentagrophytes (*In HIV/AIDS -T.rubrum)
- DDX: Allergic contact dermatitis, Candidal chronic paronychia, Psoriasis, Lichen planus, Nail dystrophies, medications
Patients with nail psoriasis are at a 2-fold risk of onychomycosis compared to those without psoriasis.
So back to my frustration about onychomycosis…as I mentioned, many patients typically have unrealistic expectations and treatment is often difficult for patients with moderate to severe nail involvement. I often have to counsel these patients that severe disease requires oral therapy with a worse prognosis. Moderate disease offers a good prognosis with oral therapy but you can still consider topicals, while mild nail involvement can be treated with either option.
Why do topical therapies usually fail in the treatment of tinea unguium? The nail plate has no stratum corneum, thus hydrophilic agents penetrate much more readily. Also, smaller molecules penetrate better, but unfortunately, most are larger and less hydrophilic. However, newer topical antifungals have improved penetration, such as efinaconazole and tavaborole solution which are used once daily for 48 weeks.
For oral therapies, recurrence rates are estimated to be between 40% and 70%. Why is this? Either the patient has severe nail disease, non-dermatophyte pathogen (such as scopulariopsis brevicaulis), host factors (immunosuppression, PVD, DM, concomitant disease, elderly), and most important…WRONG DIAGNOSIS!!! Although it can be a challenging disorder to treat, I’ve learned that it takes patience and realistic expectations from all involved (patient and provider).
Well, I hope I’ve been able to give you some helpful tips on treatment options for the various fungal infections that you will certainly encounter in your clinic. And remember…
if it’s scaly, scrape it!