TODAY.com recently posted an article about one woman’s experience with subungual melanoma, which was initially diagnosed as a mole. What are some common mimics to nail melanoma that could result in a missed diagnosis, and when should a dermatologist perform a nail biopsy?
For expert advice, I reached out to Shari Lipner, MD, PhD, associate professor of clinical dermatology and director of the nail division at Weill Cornell Medicine in New York. Dr. Lipner will speak on nail disorders in patients with skin of color at Skin of Color Update 2022.
How likely is a dermatologist to encounter a patient with a subungual melanoma?
Nail melanomas are relatively uncommon. Since dermatologists are trained in diagnosing nail disorders, in addition to skin and hair conditions, they are likely to encounter several nail melanomas over the course of their careers. With a thorough nail examination, a dermatologist can detect nail melanomas in the in situ stage and save lives!
Nail discoloration is quite common and often benign. What are some mimics to subungual melanoma that may cause a missed diagnosis?
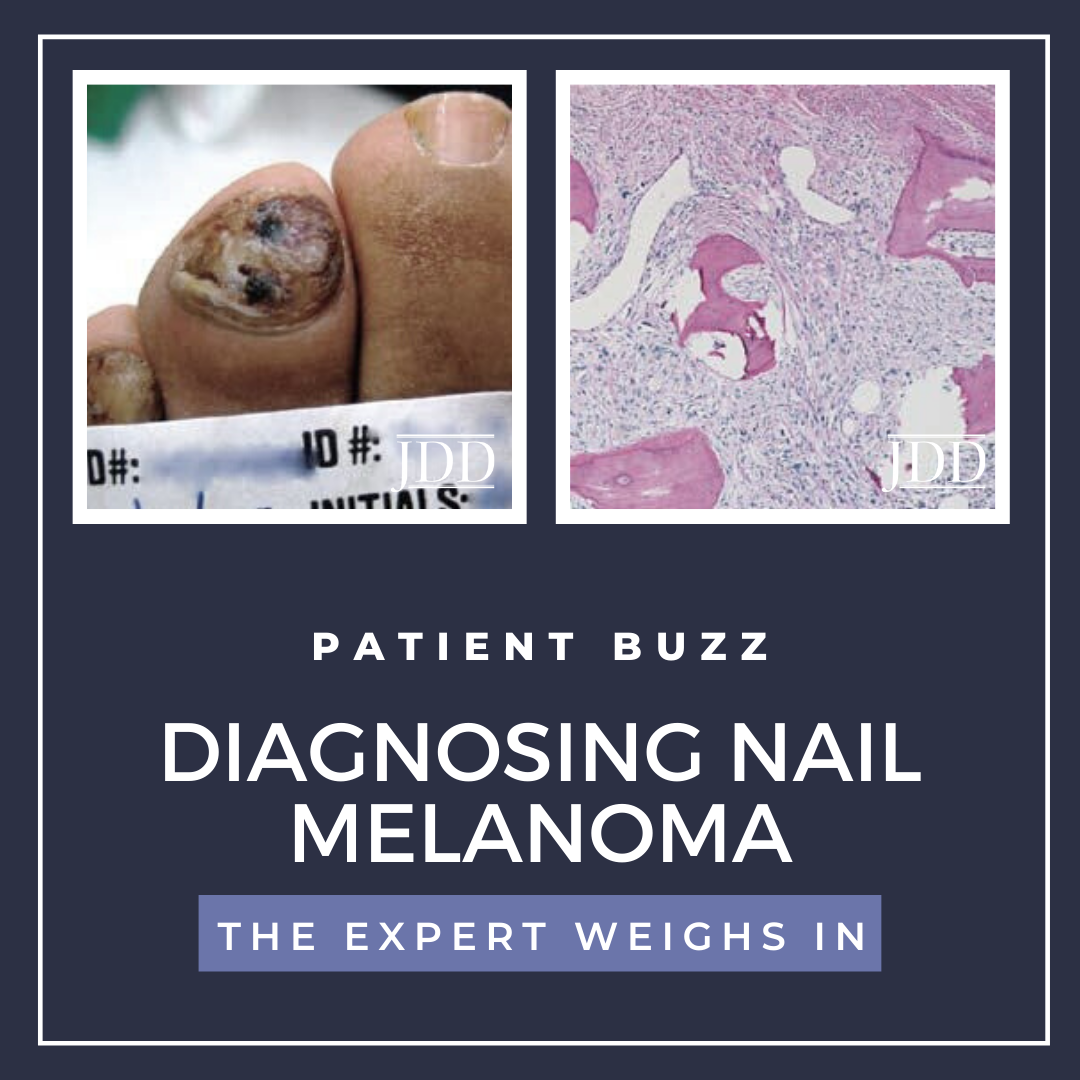
Longitudinal melanonychia is a brown to black line extending the length of the nail plate and is commonly seen in dermatological practice. The differential diagnosis of longitudinal melanonychia is quite broad and includes exogenous pigment, hematoma, bacterial and fungal infections, melanocytic activation, nevi and melanomas.
What are some key indicators dermatologists should look for when suspecting subungual melanoma?
A nail melanoma should be suspected when the longitudinal band involves a single digit, particularly the thumb or hallux, is black or multi-colored, wide, has associated pigment on the skin, has irregular lines on dermoscopy, is split, bleeding, painful and is evolving.
In what situations do you recommend a biopsy?
A nail matrix biopsy is recommended for patients with clinical findings of a brown to black longitudinal band, that is wide, split, bleeding, painful, or that is evolving. Ideally, the nail plate should be partially avulsed and a tangential shave of the matrix performed to make the diagnosis. In equivocal cases, the patient can be followed every few months, with clinical and dermoscopic photographs and measurements to evaluate for changes.
If the biopsy results show subungual melanoma, should dermatologists perform the removal surgery themselves or refer to a nail specialist or other provider?
The preferred technique for treatment of nail unit melanoma in situ is an en bloc excision, that is, removal of the entire nail unit, including the nail matrix. Dermatologists who have been trained in this technique may perform it themselves. Dermatologists who do not feel comfortable performing en bloc nail unit excisions may refer patients to dermatologists who are nail specialists or Mohs surgeons.
What additional tips or advice do you have for dermatologists when diagnosing and treating subungual melanoma?
Diagnosing nail melanomas is challenging. Dermatologists should have a low threshold to perform a biopsy of the nail matrix when there are concerning signs and symptoms for nail melanoma. Residents should gain confidence and competency in performing nail biopsies during residency. Dermatology residents without nail specialists on faculty should seek opportunities at outside institutions to learn nail procedures.
Did you enjoy this Patient Buzz Expert Commentary? You can find more here.