NBC News was one of the media outlets who covered the Marines’ recent tightening of shaving waivers, which could negatively impact the careers of Marines with pseudofolliculitis barbae (PFB). Under a 2022 policy, Marines with treatment-resistant PFB could receive temporary or permanent shaving waivers. Now, Marines with PFB could be separated from the branch if their PFB does not improve within a year under a four-part treatment plan. Critics say the change discriminates against Black Marines.
For background on PFB in patients with skin of color, I interviewed Andrew F. Alexis, MD, MPH, FAAD, professor of clinical dermatology and vice-chair for diversity and inclusion at the Weill Cornell Medical College Department of Dermatology. Dr. Alexis is also the Skin of Color Update conference co-chair, where he will lecture on a variety of medical dermatology topics.
How commonly do you see PFB in your practice, and do you find that it’s more common in your patients with skin of color?
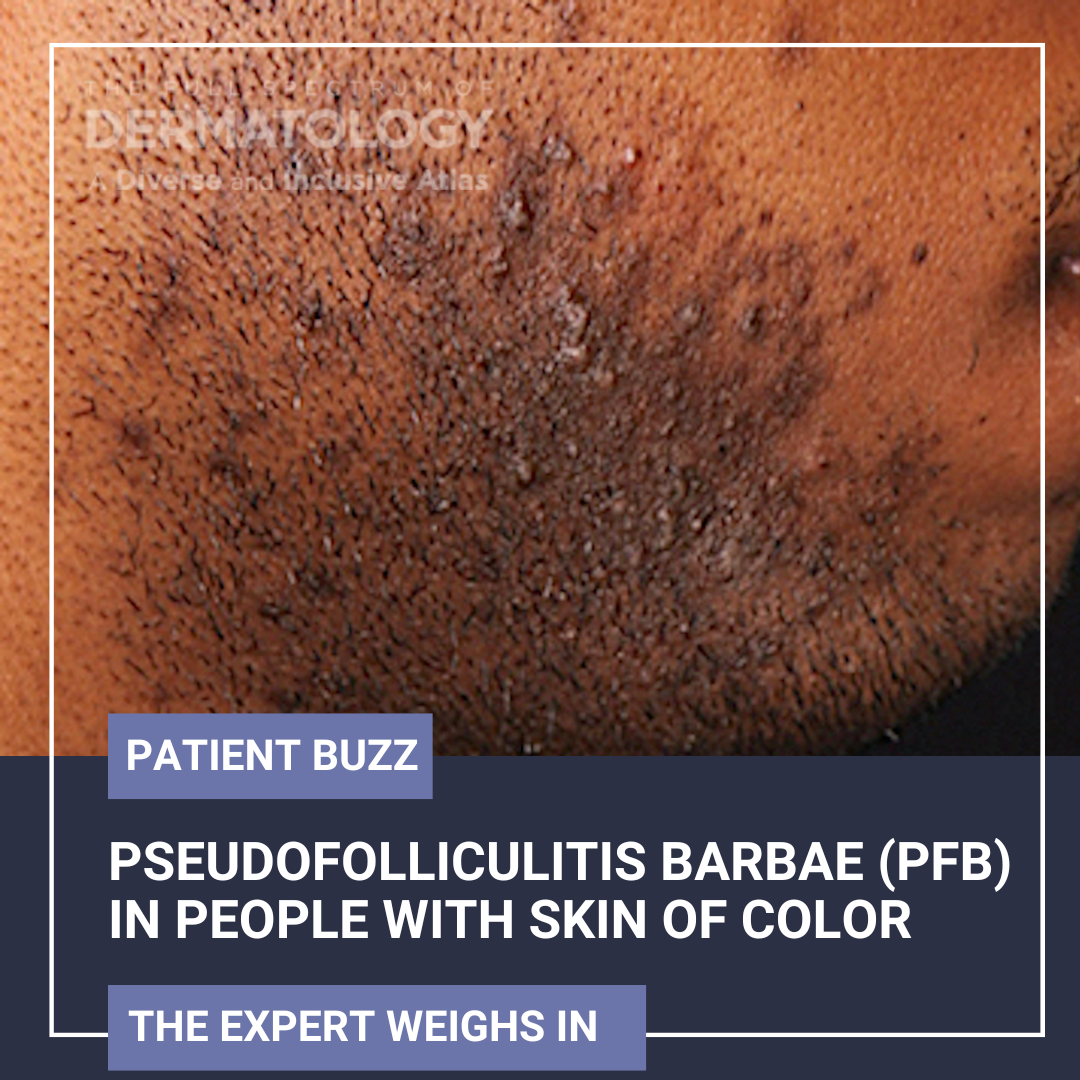
I would estimate that PFB is one of the top 10 most common disorders I see in my practice. In my practice, as in the dermatologic literature, it is more common in my patients with skin of color, especially Black or African American men. However, women who remove unwanted hair by tweezing or shaving are also affected.
What are some misconceptions about the condition?
One misconception is that PFB cannot be treated. There are medical and procedural treatment options that can improve the condition.
What’s your approach to treating PFB?
My approach includes providing guidance on shaving techniques and prescribing medications that reduce inflammation, promote exfoliation, and help reduce associated hyperpigmentation. As an adjunct to medical therapy and as a long-term solution, I routinely recommend laser hair removal.
What are some considerations that dermatologists should take note of when treating PFB?
Some considerations include taking a good history regarding patients’ shaving or hair removal practices. This is important because some of these practices contribute to or exacerbate PFB, such as close shaving leading to transfollicular penetration of the hair shaft into the dermis or tweezing contributing to inflammation and associated post-inflammatory hyperpigmentation.
How common is it for PFB to be resistant to topical treatment?
Topical therapy alone is often not able to yield satisfactory results, particularly in moderate-to-severe cases. Combination therapy with topicals (e.g., retinoids, benzoyl peroxide-clindamycin), oral agents (e.g., doxycycline, sarecycline, minocycline), intralesional corticosteroids to larger inflamed papules or nodules (e.g., 2.5-3.3 mg/mL), and laser hair removal (e.g., 1064 nm Nd:YAG) are often necessary to get the most efficacious outcomes. Superficial chemical peels (e.g., salicylic acid or glycolic acid) can also be used as an adjunct in some cases to reduce hyperpigmentation and help prevent extrafollicular penetration of the hair shafts.
What lifestyle recommendations do you make to your PFB patients?
I advise against tweezing hairs. For manual razor shaving, I recommend the following:
-
- Use blades that have been formulated to reduce excessively close shaves (which contributes to follicular penetration) and minimize mechanical irritation.
- Hydrate the beard pre-shave by washing with water and a hydrating cleanser followed by a moisturizing shaving gel or cream (to reduce surface tension and associated mechanical irritation).
- Shaving with the grain and not pulling the skin taught (to prevent follicular penetration of the shaved hair shafts).
For electric shaving, I recommend leaving short stubble (e.g., approximately 0.5-1mm) to prevent follicular penetration.
Some patients may choose to grow a beard (i.e., discontinued shaving), which is also curative in most cases.
Chemical depilatories as an alternative to shaving can be useful in some cases. However, risk of irritation is a limitation.
What other conditions can present either concurrently with or subsequently after PFB?
PIH, keloids, hypertrophic scars, and linear atrophic scars are common concurrent conditions.
What is important for dermatologists to know about PFB, especially when treating patients with skin of color?
Combination therapy, including medical and procedural therapies as well as behavioral modification (shaving guidance and avoidance of exacerbating factors), is key to success. Concomitant management of PIH and scars (if applicable) is also key.
Did you enjoy this Patient Buzz Expert Commentary? You can find more here.