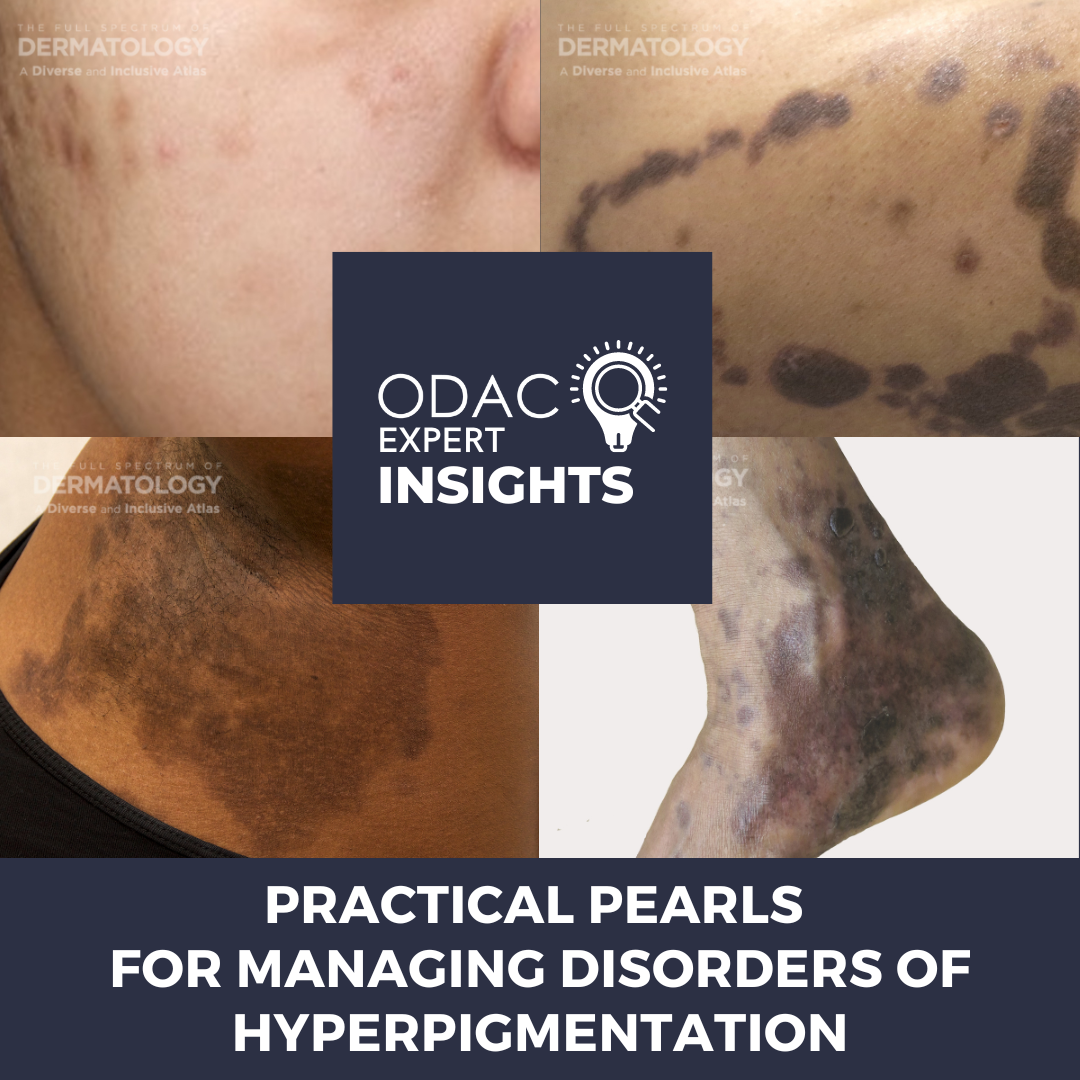
If you find diagnosing disorders of hyperpigmentation challenging, then this is just for you! I had the privilege of attending the 2023 ODAC Dermatology, Aesthetic, and Surgical Conference to learn about disorders of hyperpigmentation from Dr. Nada Elbuluk. Dr. Elbuluk is an Associate Professor and Director of the Skin of Color Program and Pigmentary Disorders Clinic at the University of Southern California Keck School of Medicine.
Hyperpigmentation tends to be a common diagnosis among patients that visit Dr. Elbuluk and our outpatient offices. In fact, it has been noted to be one of the top diagnoses for many patients, including patients of color [1]. After all, it significantly affects our patients’ quality of life, and hyperpigmentation may bother patients more than the primary diagnosis. For example, the dark spots that stay after acne, known as postinflammatory hyperpigmentation (PIH), can be a sign of the intensity of inflammation the person is experiencing from their acne. As such, Dr. Elbuluk urges us to think about addressing both the acne and the hyperpigmentation when discussing treatment with our patients. The differential diagnosis for hyperpigmentation can be very wide and careful examination and questioning can reveal underlying diagnoses. This differential can include inflammatory, infectious, and neoplastic processes amongst others.
During her session, Dr. Elbuluk discussed several cases that were of great clinical value to exemplify the importance of thinking of a wide differential:
Case 1
A middle-aged woman was losing her hair at the vertex of her scalp and presented with fine papules on the face. The initial diagnosis was central centrifugal cicatricial alopecia and acne, but the patient chose to seek a second opinon. Dr. Elbuluk’s keen eye noted the patient’s fine papules on the face and the loss of the lateral eyebrows and not only on the scalp, as previously thought. Dermoscopy revealed a brown pseudonetwork and decreased hair density with faint erythema. A biopsy was performed on the scalp and the face, which revealed findings consistent with lichen planus pigmentosus and lichen planopilaris. This case highlights that doing a biopsy can be helpful and necessary at times to elicit the correct diagnosis.
Case 2
A Caribbean woman with a history of melasma had used many topical therapies but noticed that her pigmentation was worsening. Dr. Elbuluk noted fine papules on the patient’s face, and dermoscopy revealed dark-brown areas with visible telangiectasias. Patient was diagnosed with ochronosis, for which an appropriate treatment regimen was recommended and hydroquinone was discontinued. This case highlights the importance of conducting a thorough history and understanding the background historical information that patients provide.
All of these cases presented by Dr. Elbuluk highlight some of the important clinical pearls that she impressed upon us when evaluating and treating patients with pigmentary disorders:
-
- Pigmentary disorders can have unique diagnostic and therapeutic challenges.
- Patients with pigmentary disorders can have more than one pigmentary condition.
- Common pigmentary conditions can have uncommon presentations.
- It’s important to determine if the pigmentation is in fact from an active disease, treatment sequelae, or post inflammatory. If it is active disease, it is important to treat the active disease and the pigmentary changes concomitantly when possible. This is especially true in the examples that Dr. Elbuluk talked about with acne and PIH.
- Obtaining a detailed history, reviewing medications, medical history, and looking at prior records is of utmost importance.
Other important clinical pearls useful in caring for these patients include:
-
- Ask the patients to change into a gown to check their entire body. Sometimes patients may have one spot that may be indicative of other areas of great interest to help make the diagnosis.
- Using a low threshold for biopsy and re-biopsying if necessary may be essential.
- Having an established relationship with dermatopathology to discuss cases where there’s a lack of clinicopathologic correlation or consensus.
- It is also important to use the tools that we have, such as Wood’s lamp and dermoscopy examinations, to obtain additional helpful information.
- Advise patients on prognosis, patience, and the importance of sun protection.
Finally, Dr. Elbuluk emphasized the need for more studies, particularly randomized controlled trials, on pigmentary disorders so that we may have better information to guide our patients. With more information being disseminated and the tips we gained from Dr. Elbuluk, perhaps you too can be more confident in making the diagnosis!
References:
-
- Amatya B, Jha AK, Shrestha S. Frequency of different types of facial melanoses referring to the Department of Dermatology and Venereology, Nepal Medical College and Teaching Hospital in 2019, and assessment of their effect on health-related quality of life. BMC Dermatol. 2020;20(1):4. Published 2020 Aug 3. doi:10.1186/s12895-020-00100-3
- Elbuluk N, Grimes P, Chien A, et al. The Pathogenesis and Management of Acne-Induced Post-inflammatory Hyperpigmentation. Am J Clin Dermatol. 2021;22(6):829-836. doi:10.1007/s40257-021-00633-4
This information was presented by Dr. Nada Elbuluk at the 2023 ODAC Dermatology, Aesthetic and Surgical Conference held January 12-15, 2023. The above highlights from her lecture were written and compiled by Dr. Nishad Sathe.
Did you enjoy this post? Find more on pigmentary disorders here.