Dermatologic surgery (particularly Mohs micrographic surgery) is associated with low overall postoperative pain that is largely readily resolvable with acetaminophen and ibuprofen. However, certain medical history and predisposing factors for postoperative pain (discussed below) may present scenarios where a broader repertoire of analgesics is required. In this Surgical Dermatology Cheat Sheet, we present an accessible reference tool for postoperative pain management in dermatologic surgery to assist with meeting the needs of our surgical patients.
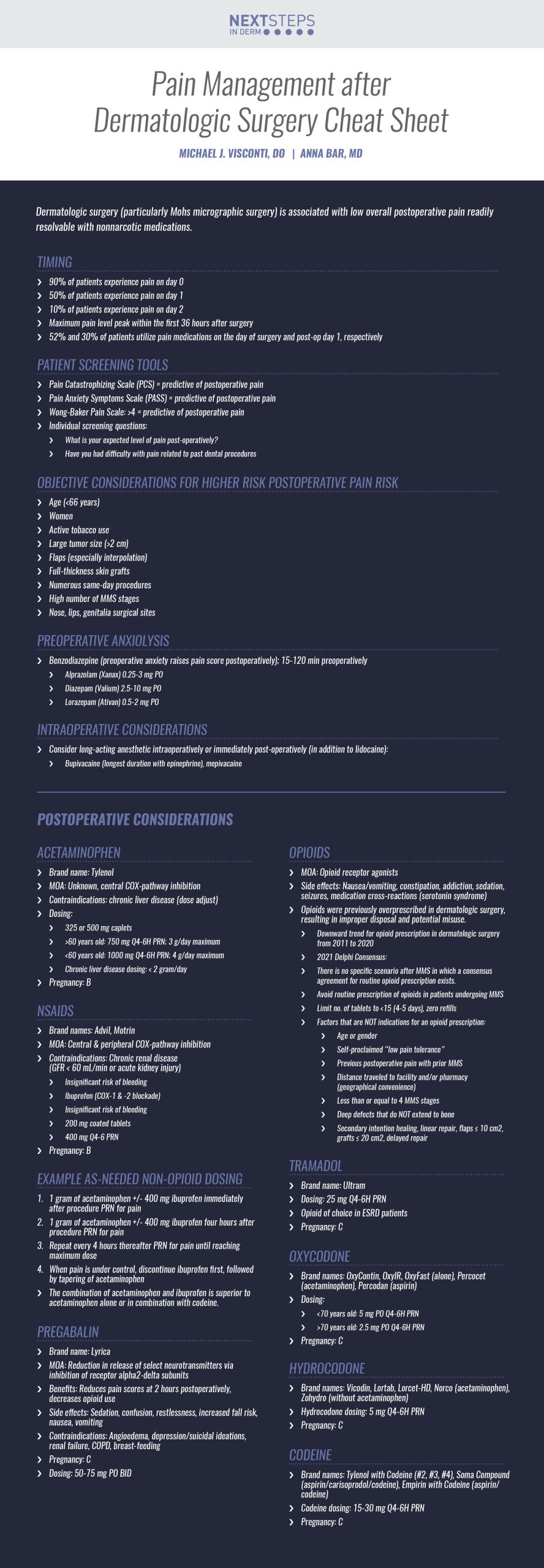
Timing
-
- 90% of patients experience pain on day 0
- 50% of patients experience pain on day 1
- 10% of patients experience pain on day 2
- Maximum pain level peak within the first 36 hours after surgery
- 52% and 30% of patients utilize pain medications on the day of surgery and post-op day 1, respectively
Patient Screening Tools
-
- Pain Catastrophizing Scale (PCS) = predictive of postoperative pain
- Pain Anxiety Symptoms Scale (PASS) = predictive of postoperative pain
- Wong-Baker Pain Scale: >4 = predictive of postoperative pain
- Individual screening questions:
- What is your expected level of pain post-operatively?
- Have you had difficulty with pain related to past dental procedures?
Objective Considerations for Higher Risk Postoperative Pain Risk
-
- Age (<66 years)
- Women
- Active tobacco use
- Large tumor size (>2 cm)
- Flaps (especially interpolation)
- Full-thickness skin grafts
- Numerous same-day procedures
- High number of MMS stages
- Nose, lips, genitalia surgical sites
Preoperative Anxiolysis
-
- Benzodiazepine (preoperative anxiety raises pain score postoperatively); 15-120 min preoperatively
- Alprazolam (Xanax) 0.25-3 mg PO
- Diazepam (Valium) 2.5-10 mg PO
- Lorazepam (Ativan) 0.5-2 mg PO
- Benzodiazepine (preoperative anxiety raises pain score postoperatively); 15-120 min preoperatively
Intraoperative Considerations
-
- Consider long-acting anesthetic intraoperatively or immediately post-operatively (in addition to lidocaine):
- Bupivacaine (longest duration with epinephrine), mepivacaine
- Consider long-acting anesthetic intraoperatively or immediately post-operatively (in addition to lidocaine):
Postoperative Considerations
Acetaminophen
-
- Brand name: Tylenol
- MOA: Unknown, central COX-pathway inhibition
- Contraindications: chronic liver disease (dose adjust)
- Dosing:
- 325 or 500 mg caplets
- >60 years old: 750 mg Q4-6H PRN; 3 g/day maximum
- <60 years old: 1000 mg Q4-6H PRN; 4 g/day maximum
- Chronic liver disease dosing: < 2 gram/day
- Pregnancy: B
NSAIDs
-
- Brand names: Advil, Motrin
- MOA: Central & peripheral COX-pathway inhibition
- Contraindications: Chronic renal disease (GFR < 60 mL/min or acute kidney injury)
- Insignificant risk of bleeding
- Ibuprofen (COX-1 & -2 blockade)
- Insignificant risk of bleeding
- 200 mg coated tablets
- 400 mg Q4-6 PRN
- Pregnancy: B
Example As-Needed Non-Opioid Dosing
-
- 1 gram of acetaminophen +/- 400 mg ibuprofen immediately after procedure PRN for pain
- 1 gram of acetaminophen +/- 400 mg ibuprofen four hours after procedure PRN for pain
- Repeat every 4 hours thereafter PRN for pain until reaching maximum dose
- When pain is under control, discontinue ibuprofen first, followed by tapering of acetaminophen
The combination of acetaminophen and ibuprofen is superior to acetaminophen alone or in combination with codeine.
Pregabalin
-
- Brand name: Lyrica
- MOA: Reduction in release of select neurotransmitters via inhibition of receptor alpha2-delta subunits
- Benefits: Reduces pain scores at 2 hours postoperatively, decreases opioid use
- Side effects: Sedation, confusion, restlessness, increased fall risk, nausea, vomiting
- Contraindications: Angioedema, depression/suicidal ideations, renal failure, COPD, breast-feeding
- Pregnancy: C
- Dosing: 50-75 mg PO BID
Opioids
-
- MOA: Opioid receptor agonists
- Side effects: Nausea/vomiting, constipation, addiction, sedation, seizures, medication cross-reactions (serotonin syndrome)
- Opioids were previously overprescribed in dermatologic surgery, resulting in improper disposal and potential misuse.
- Downward trend for opioid prescription in dermatologic surgery from 2011 to 2020
- 2021 Delphi Consensus:
- There is no specific scenario after MMS in which a consensus agreement for routine opioid prescription exists.
- Avoid routine prescription of opioids in patients undergoing MMS
- Limit no. of tablets to <15 (4-5 days), zero refills
- Factors that are NOT indications for an opioid prescription:
- Age or gender
- Self-proclaimed “low pain tolerance”
- Previous postoperative pain with prior MMS
- Distance traveled to facility and/or pharmacy (geographical convenience)
- Less than or equal to 4 MMS stages
- Deep defects that do NOT extend to bone
Tramadol
-
- Brand name: Ultram
- Dosing: 25 mg Q4-6H PRN
- Opioid of choice in ESRD patients
- Pregnancy: C
Oxycodone
-
- Brand names: OxyContin, OxyIR, OxyFast (alone), Percocet (acetaminophen), Percodan (aspirin)
- Dosing:
- <70 years old: 5 mg PO Q4-6H PRN
- >70 years old: 2.5 mg PO Q4-6H PRN
- Pregnancy: C
Hydrocodone
-
- Brand names: Vicodin, Lortab, Lorcet-HD, Norco (acetaminophen), Zohydro (without acetaminophen)
- Hydrocodone dosing: 5 mg Q4-6H PRN
- Pregnancy: C
Codeine
-
- Brand names: Tylenol with Codeine (#2, #3, #4), Soma Compound (aspirin/carisoprodol/codeine), Empirin with Codeine (aspirin/codeine)
- Codeine dosing: 15-30 mg Q4-6H PRN
- Pregnancy: C
CLICK ON THE IMAGE BELOW TO ENLARGE AND/OR DOWNLOAD YOUR CHEAT SHEET
-
- Boettler, Michelle A., et al. “Safety and Efficacy of Oral Benzodiazepines for Periprocedural Anxiolysis: A Systematic Review.” Dermatologic Surgery: Official Publication for American Society for Dermatologic Surgery [et al.] (2022).
- Carroll, Pugliese, et al. “Acute and Chronic Pain Management in Dermatology. American Academy of Dermatology Dialogues in Dermatology Podcast. iTunes (2022): https://downloads.ctfassets.net/3l981im5dunw/1NjzdQsRXlyVx8ESplDNc4/13a019c9b46c84fa42942018e1dc6088/Acute___Chronic_Pain_Management.Feb_21.mp3
- Chen, Andrea F., et al. “Prediction of postoperative pain after Mohs micrographic surgery with 2 validated pain anxiety scales.” Dermatologic Surgery 41.1 (2015): 40-47.
- Donigan, Jessica M., et al. “Opioid prescribing recommendations after Mohs micrographic surgery and reconstruction: a Delphi consensus.” Dermatologic Surgery 47.2 (2021): 167-169.
- Eikenberg, Joshua D., et al. “Postoperative Pain After Mohs Surgery: Physician Perceptions and How Those Perceptions Influence Opioid Prescribing Practices.” Dermatologic Surgery 47.2 (2021): 170-173.
- Evans, Tyler, et al. “How We Do It: Postoperative Pain Control in Mohs Micrographic Surgery.” Dermatologic Surgery 47.2 (2021): 280-282.
- Firoz, Bahar F., et al. “An analysis of pain and analgesia after Mohs micrographic surgery.” Journal of the American Academy of Dermatology 63.1 (2010): 79-86.
- Harris, KaLynne, et al. “Opioid pain medication use after dermatologic surgery: a prospective observational study of 212 dermatologic surgery patients.” JAMA dermatology 149.3 (2013): 317-321.
- Kelley, Brian P., et al. “Ibuprofen does not increase bleeding risk in plastic surgery: a systematic review and meta-analysis.” Plastic and reconstructive surgery 137.4 (2016): 1309.
- Merritt, Bradley G., et al. “The safety of Mohs surgery: a prospective multicenter cohort study.” Journal of the American Academy of Dermatology 67.6 (2012): 1302-1309.
- Paul, Deborah, et al. “Review of Mohs Surgeons’ Intraoperative Anxiolytic Practices: A Survey of the American College of Mohs Surgery.” Dermatologic Surgery (2022): 10-1097.
- Saco, Michael, and Nicholas Golda. “Optimal timing of postoperative pharmacologic pain control in Mohs micrographic surgery: A prospective cohort study.” Journal of the American Academy of Dermatology 82.2 (2020): 495-497.
- Sniezek, Patrick J., David G. Brodland, and John A. Zitelli. “A randomized controlled trial comparing acetaminophen, acetaminophen and ibuprofen, and acetaminophen and codeine for postoperative pain relief after Mohs surgery and cutaneous reconstruction.” Dermatologic surgery 37.7 (2011): 1007-1013.
Did you enjoy this article? Find more on surgical dermatology topics here.