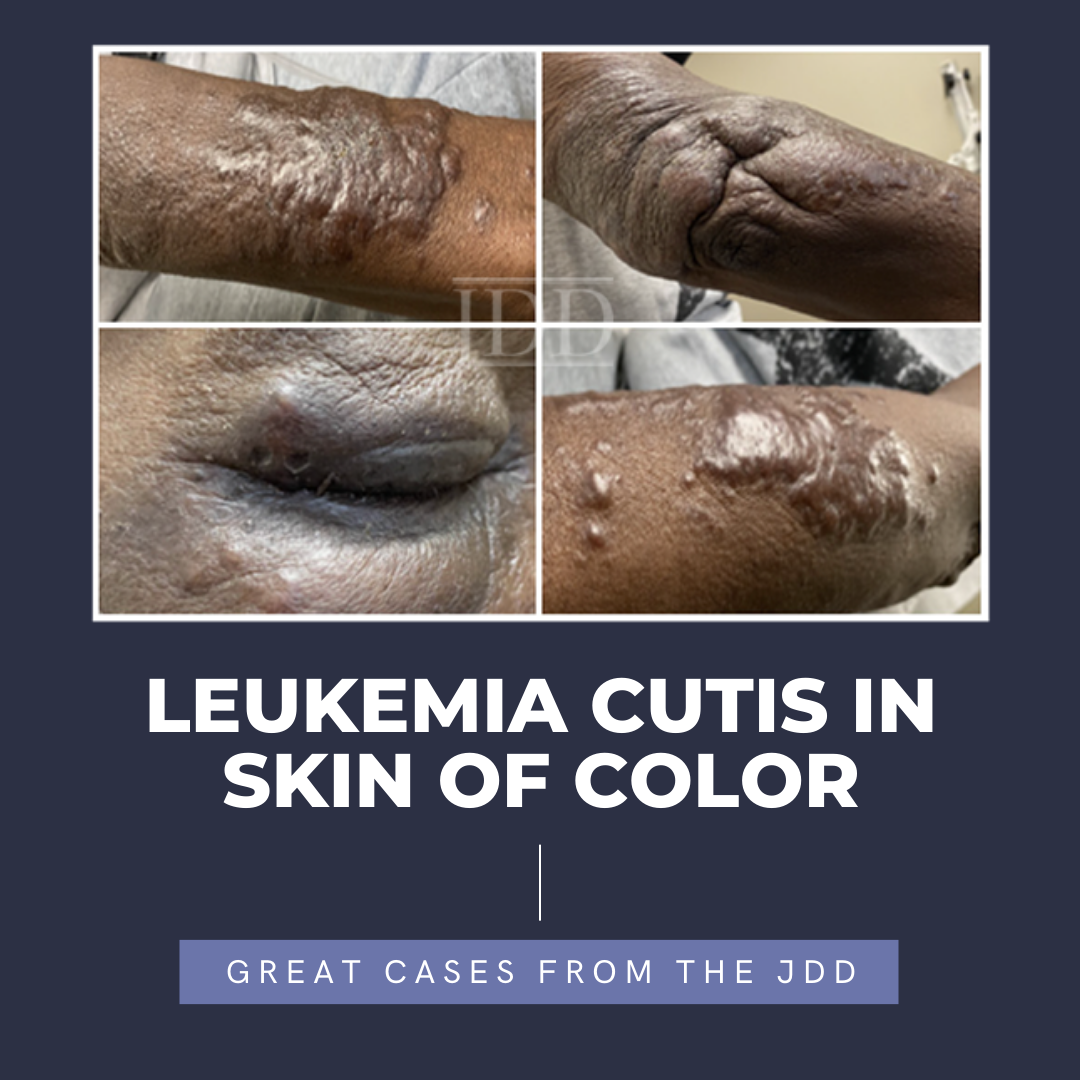
The various presentations of many dermatologic conditions among various skin types are slowly being elucidated throughout the recent years. These differences present as an issue as it leads to delayed diagnosis, treatment, and poorer quality of life. Herein, JDD authors Susuana Adjei MD, et al. present the characteristics of leukemia cutis in a skin of color patient with diagnosed chronic myelomonocytic leukemia.
INTRODUCTION
The malignant transformation of hematopoietic cells leads to the manifestation of leukemia.1 Depending on the cell lineage and maturity, the main overarching subtypes of leukemia are acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL), chronic myeloid leukemia (CML), and chronic lymphoblastic leukemia (CLL).1
In addition to bone marrow and peripheral blood involvement, extramedullary forms of leukemia such as granulocytic sarcoma and leukemia cutis also exist.2 Leukemia cutis (LC) is the infiltration of leukemia cells in the skin, leading to clinically apparent lesions, and occurs in about 3% of leukemia patients.3 While the pathophysiology of LC remains unknown, there is speculation that the migration of leukemia cells to the skin is a result of an attraction between various expressed chemokines and adhesion molecules.4 Genetic variations have also been associated with this extramedullary involvement of AML such as the inversion of chromosome 16, rearrangement of chromosome 11q23, and NPM1 mutation.5 LC typically occurs concomitantly or after leukemia diagnosis, but can rarely precede it by months to years.6 Approximately 55-77% of LC patients are diagnosed with leukemia prior to presentation.6 Compared with the other leukemias, AML and CLL have a higher propensity to cause LC, specifically those with AML. Poorer prognosis of leukemia is suspected when there is cutaneous involvement.5 Wang et al conducted a retrospective study of matched AML subjects with or without LC and revealed the 5-year survival to be 8.6% and 23.8%, respectively.5
CASE

 DISCUSSION
DISCUSSION
There are a paucity of data available for LC, specifically in those of skin of color; however, the differences in how LC presents across various groups can provide insight. There are ethnic and racial disparities evident in the incidence of leukemia. Non-Hispanic Whites (NHW) typically have the highest incidence and yet a better survival rate than those that are not NHWs.7 According to pooled data from 2010 to 2014, Whites had a higher incidence of AML than in Blacks, Pacific Islanders/Asians, and Hispanics.8 However, additional data from 1999 to 2008 revealed a higher risk of death at 12% and 6% in Blacks and Hispanics, respectively, compared with Whites.8 There were also apparent differences in treatment and treatment outcomes, where Hispanic and Black patients with AML and ALL were noted to have worse overall survival.8 Being African American was discovered to be an independent predictor for a shortened overall survival in patients with CLL.9
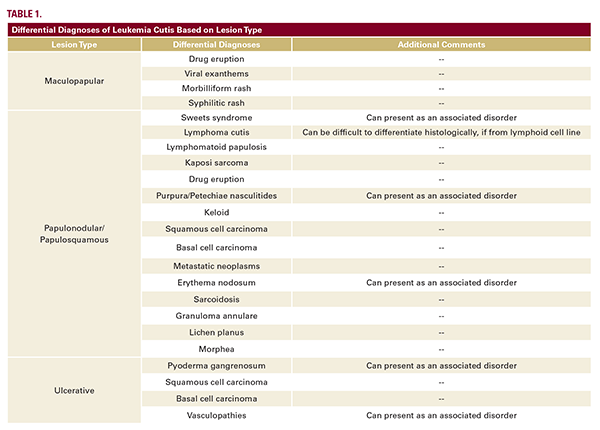
Dermatologic conditions can present differently in SOC, leading to delayed diagnoses and worse outcomes. Given its rarity and variable morphology, LC mimics other pathologies; thus, differences due to SOC should be also considered. A known leukemia history increases suspicion for LC, but in the rare cases of aleukemic LC (occurring in 2-3% of cases), diagnosis can be more elusive.6,10 Leukemia cutis lesions can present as erythematous/violaceous or skin-colored, solitary or multiple papules, nodules/tumors, plaques, ulcers, or even gingival hyperplasia.6 The distribution can either be disseminated or localized, but lesions have no predilection for specific anatomical sites.6 Differential diagnoses to be considered LC are included in Table 1.
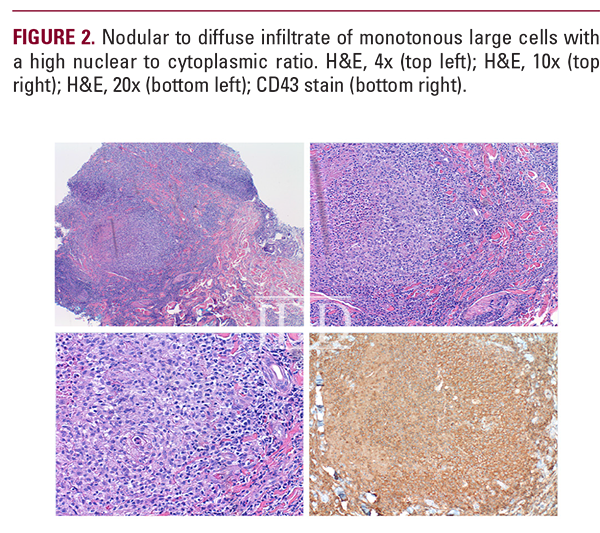
 Histology and immunohistochemistry are also crucial in the accurate diagnosis of LC. Histological findings typically reveal leukemia cells infiltrating superficial to deep layers of the skin.11 There can also be evidence of a “Grenz zone” or dermal-epidermal junction, suggesting perivascular and periadnexal infiltrate, especially in the acute leukemias.10
Histology and immunohistochemistry are also crucial in the accurate diagnosis of LC. Histological findings typically reveal leukemia cells infiltrating superficial to deep layers of the skin.11 There can also be evidence of a “Grenz zone” or dermal-epidermal junction, suggesting perivascular and periadnexal infiltrate, especially in the acute leukemias.10
CONCLUSION
DISCLOSURES
REFERENCES
-
- Preisler HD. The leukemias. Dis Mon. 1994;40(10):525-579.
- Grunwald MR, McDonnell MH, Induru R, et al. Cutaneous manifestations in leukemia patients. Semin Oncol. 2016;43(3):359-365.
- Bakst RL, Tallman MS, Douer D, et al. How I treat extramedullary acute myeloid leukemia. Blood. 2011;118(14):3785-93.
- Cho-Vega JH, Medeiros LJ, Prieto VG, et al. Leukemia cutis. Am J Clin Pathol. 2008;129(1):130-142
- Wang CX, Pusic I, Anadkat MJ. Association of leukemia cutis with survival in acute myeloid leukemia. JAMA Dermatol. 2019;155(7):826-832.
- Gunnar Wagner, Klaus Fenchel, Walter Back, et al. Leukemia cutis – epidemiology, clinical presentation, and differential diagnoses. J Dtsch Dermatol Ges. 2012;10(1):27-36.
- Matasar MJ, Ritchie EK, Consedine N, et al. Incidence rates of the major leukemia subtypes among US Hispanics, Blacks, and non-Hispanic Whites. Leuk Lymphoma. 2006;47(11):2365-2370.
- Kirtane K, Lee SJ. Racial and ethnic disparities in hematologic malignancies. Blood. 2017;130(15):1699-1705.
- Falchi L, Keating MJ, Wang X, et al. Clinical characteristics, response to therapy, and survival of African American patients diagnosed with chronic lymphocytic leukemia: joint experience of the MD Anderson Cancer Center and Duke University Medical Center. Cancer. 2013;119(17):3177-3185.
- Martínez-Leboráns L, Victoria-Martínez AM, Torregrosa-Calatayud JL, et al. Leukemia cutis: a report of 17 cases and a review of the literature. (Leucemia cutis. Serie de 17 casos y revisión de la literatura.) Actas Dermosifiliogr. 2016;107(9):e65-e69.
- Li L, Wang Y, Lian CG, et al. Clinical and pathological features of myeloid leukemia cutis. An Bras Dermatol. 2018;93(2):216-221.
- Cibull TL, Thomas AB, O’Malley DP, et al. Myeloid leukemia cutis: a histologic and immunohistochemical review. J Cutan Pathol. 2008;35(2):180-185.
- Qiao Y, Jian J, Deng L, et al. Leukaemia cutis as a specific skin involvement in chronic myelomonocytic leukaemia and review of the literature: Acknowledgments. Transl Cancer Res. 2020;9(8):4988-4998.
Source
Adjei, Susuana, et al. “Leukemia Cutis in Skin of Color.” Journal of Drugs in Dermatology: JDD 22.7 (2023): 687-689.
Adapted from original article for length and style.
Did you enjoy this JDD case report? You can find more here.