Hyaluronic acid (HA) fillers are widely used in aesthetic medicine for facial rejuvenation, volumization, and wrinkle treatment. Noninflammatory nodules after HA filler injection are a relatively common phenomenon and a result of poor technique or a large volume bolus in one area.¹ Unlike these nodules, delayed-onset nodules (DON) occur in 0.5% of injections and can be inflammatory, granulomatous, or infectious. They often present as firm, nodular masses with variable swelling and drainage.² While relatively uncommon, DONs are a significant complication of HA filler treatment, and understanding the pathophysiology, diagnosis, and management of DONs is essential for clinicians to minimize risks and optimize patient outcomes.
CASE SUMMARY
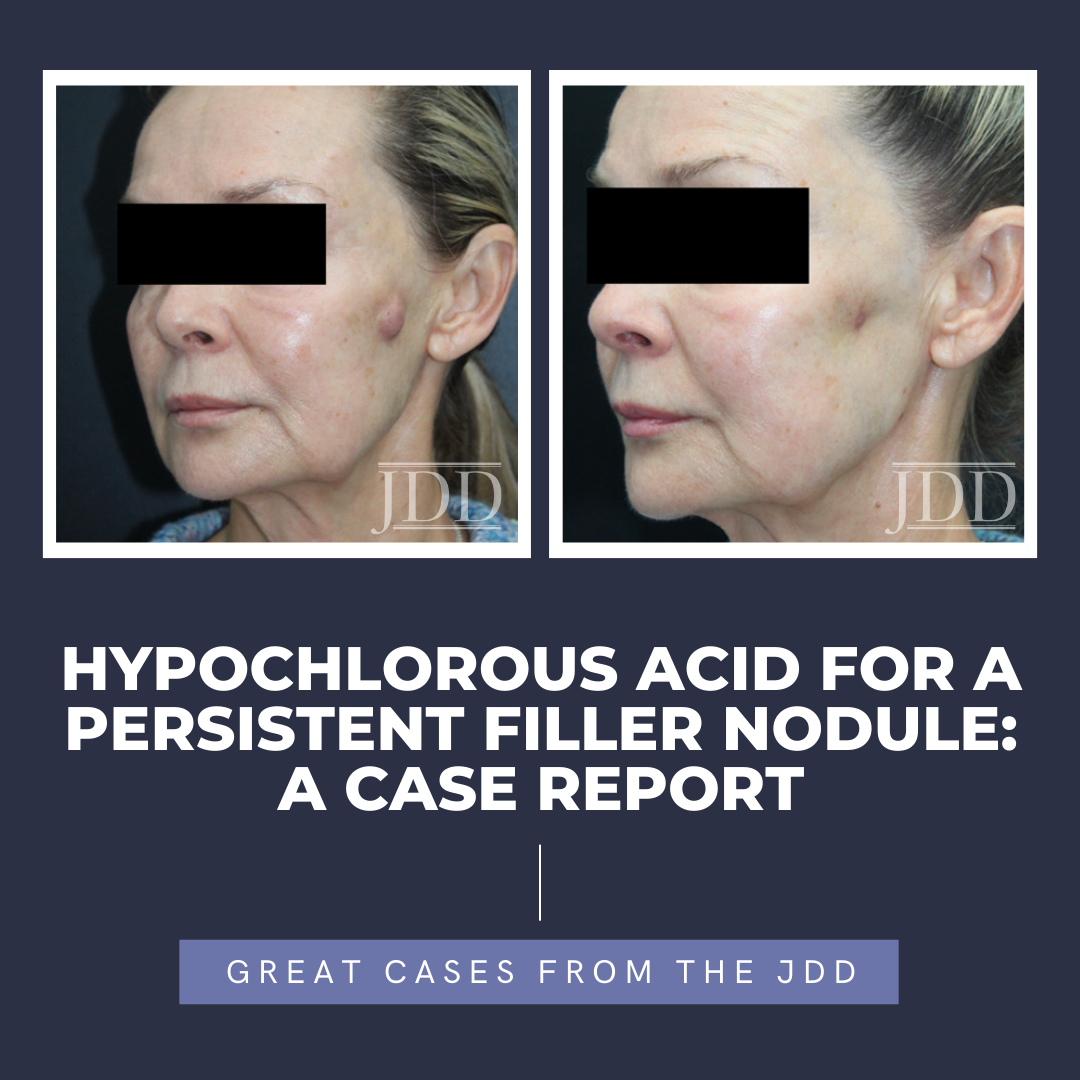
A sixty-year-old female presented to the clinic with a 3 cm hard, rope-like indurated nodule with finger-like projections and purulent exudate on the left zygomatic cheek (Figure 1). The patient had been injected with Skinvive™ at an outside medical facility for facial rejuvenation of the cheeks 2 months prior. She developed a firm, growing nodule, which was treated with hyaluronidase on 6 separate occasions. She was also treated with a combination of intralesional fluorouracil, dexamethasone, and Kenalog as well as one course of doxycycline and three courses of a Medrol dose pack. Steroid treatment resulted in attenuation of growth, but the nodule grew subsequently.

At our office, incision and drainage were performed along with irrigation with hypochlorous acid. The patient was initially injected with a combination solution of 1.0 cc of fluorouracil, 0.5 cc of dexamethasone and 1.0 cc of Kenalog 10 along with 0.2 cc of Ceftriaxone and was given a five-day course of colchicine. One week later, the patient was injected with 20 units of hyaluronidase and 0.5 cc of hypochlorous acid. The patient returned to the clinic 3 weeks later, and was injected with 10 units of hyaluronidase, followed by 0.3 cc of hypochlorous acid, followed by the combination solution of fluorouracil, dexamethasone, and Kenalog 10. Following treatment, the lesion decreased in size significantly with no tenderness, swelling, or drainage (Figure 2).

DISCUSSION
Nodules are a significant complication of aesthetic procedures, made further challenging because patients often seek medical help from a different provider than the one who performed the procedure.³ However, understanding treatment options for DONs is important for minimizing complications and restoring patient trust.
DONs can be inflammatory, granulomatous, or infectious. For inflammatory and granulomatous nodules, corticosteroids and 5-fluorouracil attenuate the immunologic response.³ Hyaluronidase can hydrolyze hyaluronan glycosaminoglycan polysaccharide complexes; however, allergic reactions can occur.³ Commercially sold fillers are greater than 500 kDa; however, degradation of these products to smaller HA molecules (520 kDa) can elicit an inflammatory response and cell migration.4
Of note, products made with Vycross technology are more resistant to hyaluronidase because these products have shorter HA chains and are more densely packed.5 Nodules that persist after these treatments can be removed surgically.
DONs can be infectious and develop biofilms. Biofilms are heterogenous extracellular matrices of bacterial colonies on the surface of injected HA that often escape immunologic detection by hindering phagocytosis by macrophages.6 Bacteria commonly found in biofilms include Pseudomonas species, Cutibacterium acnes (formerly Propionibacterium acnes), and resident skin and mucosal flora such as Streptococcus, Enterococcus, and Staphylococcus species.6 These nodules can be managed with incision and drainage followed by administration of hyaluronidase.8 Although the culture of nodules is recommended, it requires tissue specimens, which may be difficult to obtain in cosmetically sensitive areas. In addition, some species of mycobacteria can take up to 6 weeks to result.9 Regardless, systemic antibiotics should cover gram-positive, gram-negative aerobic bacteria, anaerobes, and/or atypical mycobacterial infection. Duration of treatment depends on clinical response, and antibiotics should be continued seven days postresolution of symptoms. Moxifloxacin and clarithromycin are commonly used empiric antibiotics, especially in the context of biofilms.10 Attila et al reported the use of 5-fluorouracil to inhibit bacterial DNA synthesis and reduce bacterial burden. Corticosteroids and non-steroidal anti-inflammatory drugs (NSAID) can attenuate the immunologic response to infections.7
Our patient’s nodule failed several courses of hyaluronidase as well as intralesional and systemic corticosteroids, intralesional fluorouracil, and systemic antibiotics. However, irrigation with and, later, intralesional injection of hypochlorous acid and oral colchicine contributed to the resolution of symptoms. Hypochlorous acid is an endogenous antimicrobial agent produced by neutrophils and macrophages for bacterial killing.11 Hypochlorous acid causes oxidation of intracellular proteins, membrane lipids, leading to inhibition of ATP and DNA synthesis. Hypochlorous acid is particularly useful as a broad-spectrum antibacterial agent because of its low molecular weight, rapid diffusion, and lack of charge, preventing it from being repelled by bacterial cell surfaces.11 Several in vivo and in vitro studies support its antimicrobial and anti-inflammatory properties which have led to its rise in the treatment of skin wounds, pruritus, diabetic ulcers and other inflammatory skin conditions.11
CONCLUSION
Infectious nodules are a significant concern for aesthetic providers, and understanding the treatment options will help mitigate complications and improve outcomes. Biofilms are a therapeutic challenge because of their antibiotic resistance, unique biochemical milieu, and ability to evade the immune system. Hypochlorous acid is a safe and effective treatment for infections because of its broad-spectrum antimicrobial coverage and oxidative properties.
DISCLOSURES
The authors have no conflict of interest to disclose.
REFERENCES
-
- Saputra DI, Kapoor KM. Management of noninflammatory nodule in chin after a large volume bolus injection of hyaluronic acid filler. Dermatol Ther. 2020;33(3):e13424. doi:10.1111/dth.13424
- Kroumpouzos G, Treacy P. Hyaluronidase for dermal filler complications: review of applications and dosage recommendations. JMIR Dermatol. 2024;7:e50403. doi:10.2196/50403
- Modarressi A, Nizet C, Lombardi T. Granulomas and nongranulomatous nodules after filler injection: different complications require different treatments. J Plast Reconstr Aesthetic Surg. 2020;73(11):2010-2015. doi:10.1016/j.bjps.2020.08.012
- Funt DK. Treatment of Delayed-onset Inflammatory reactions to hyaluronic acid filler: an algorithmic approach. Plast Reconstr Surg Glob Open. 2022;10(6):e4362. doi:10.1097/GOX.0000000000004362
- Faivre J, Pigweh AI, Iehl J, et al. Crosslinking hyaluronic acid soft-tissue fillers: current status and perspectives from an industrial point of view. Expert Rev Med Devices. 2021;18(12):1175-1187. doi:10.1080/17434440.20 21.2014320
- Zhang Y liang, Sun Z sheng, et al. Biofilm formation is a risk factor for late and delayed complications of filler injection. Front Microbiol. 2024;14:1297948. doi:10.3389/fmicb.2023.1297948
- Dumitraşcu DI, Georgescu AV. The management of biofilm formation after hyaluronic acid gel filler injections: a review. Clujul Med 1957. 2013;86(3):192- 195.
- Ferneini EM, Beauvais D, Aronin SI. An overview of infections associated with soft tissue facial fillers: identification, prevention, and treatment. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 2017;75(1):160-166. doi:10.1016/j.joms.2016.09.004
- Uwamino Y, Hasegawa N, Kamoshita Y, et al. Optimal incubation duration of liquid cultures for assessing culture negative conversion in patients with Mycobacterium avium complex and Mycobacterium abscessus pulmonary diseases. Eur J Clin Microbiol Infect Dis. 2025;44(1):45-51. doi:10.1007/ s10096-024-04973-x
- Marusza W, Olszanski R, Sierdzinski J, et al. Treatment of late bacterial infections resulting from soft-tissue filler injections. Infect Drug Resist. 2019;12:469-480. doi:10.2147/IDR.S186996
- Del Rosso JQ, Bhatia N. Status Report on topical hypochlorous acid: clinical relevance of specific formulations, potential modes of action, and study outcomes. J Clin Aesth Dermatol. 2018;11(11):36-39.
SOURCE
Urbanski, Nicholas, Kanthi Bommareddy, and Shino Bay Aguilera. “Hypochlorous Acid for a Persistent Filler Nodule: A Case Report.” Journal of drugs in dermatology: JDD 24, no. 9 (2025): 934-936.
Content and images used with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
Did you enjoy this JDD case report? You can find more here.