The fusion of technology and medicine has led to the advent of advanced wound healing techniques that may be adapted to the management of surgical defects. Shortened duration of healing and ease-of-use are two potential benefits under investigation. Here, Matthew J. Lin MD, Danielle P. Dubin BA, Aaron S. Farberg MD, Hooman Khorasani MD, David A. Kriegel MD describe a 65-year-old male with a nasal alar wound that was allowed to heal with secondary intention, assisted by a novel methacrylate polymer powder dressing.
Background
Advances in technology have recently contributed to the development of innovative wound healing modalities that hold promise for the management of surgical defects.
Case
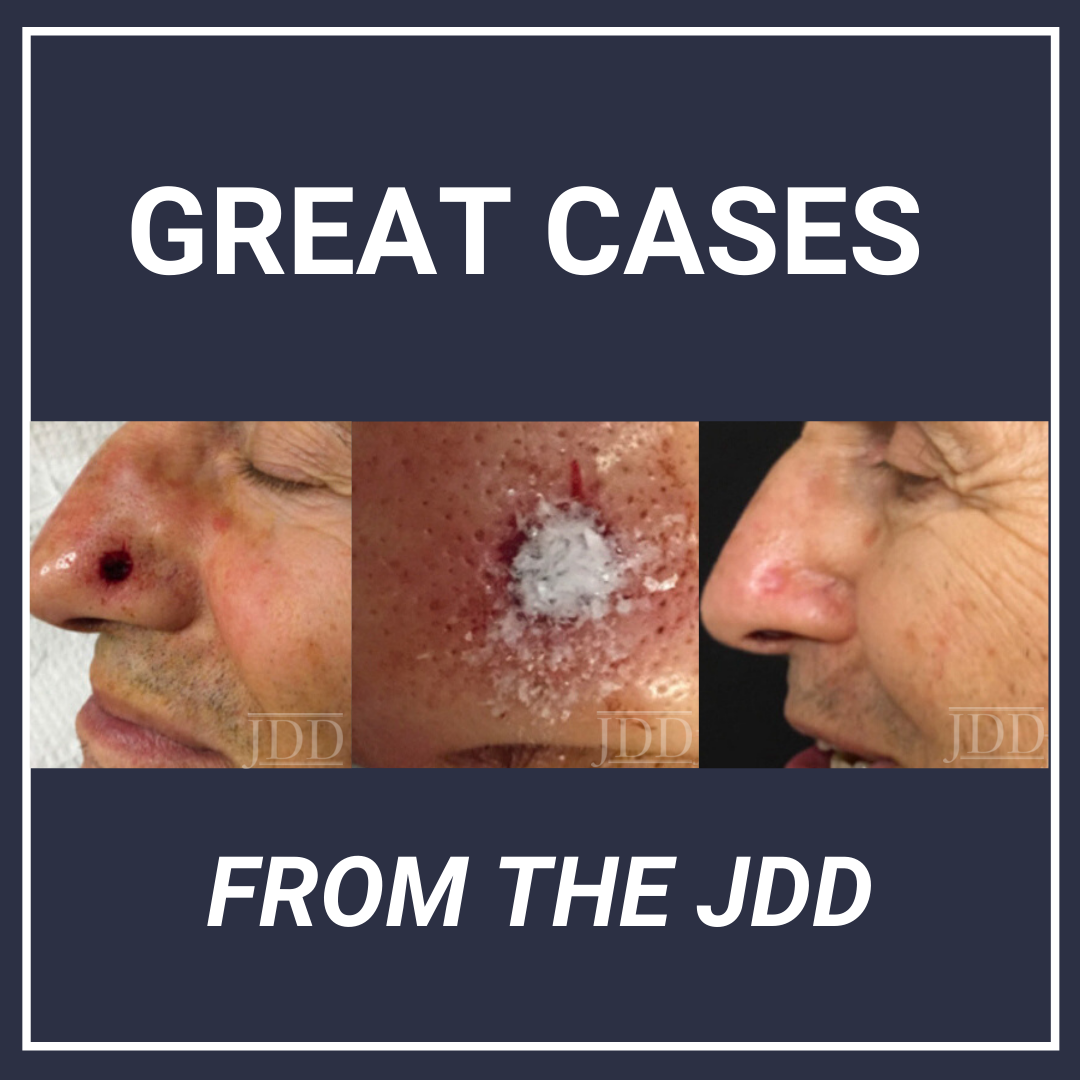
65-year-old Caucasian man presented with a biopsy-proven nodular basal cell carcinoma on the left nasal alar. The tumor was cleared after 2 stages of Mohs Micrographic Surgery with excision down to the nasalis muscle. The resultant defect measured 12mm x 14mm in area and 5mm in depth (wound size 840mm3). Reconstructive options were discussed, including random pattern flap repair, skin graft and secondary intention healing with the aid of a novel methacrylate powder dressing.The patient preferred to proceed with secondary intention healing assisted by the methacrylate powder dressing.
After achieving hemostasis, 10mg of a sterile, biologically inert polymerized methacrylate powder dressing (Altrazeal™, Uluru Inc., TX) was poured over the wound in a uniform layer to fill and seal the entire surface. 0.1ml of sterile ionic saline was sprayed onto the powder to activate the dressing. The single dressing was left intact for 3 weeks. A post-operative follow-up visit at 3 weeks found the wound completely epithelialized and reduced in size to 9 x 10mm in area and 1mm in depth (wound size volume 90mm3). This represented a 90% reduction in wound (Figure 1). The dressing was easy to maintain, non-painful, and there were no reported adverse effects.

Discussion
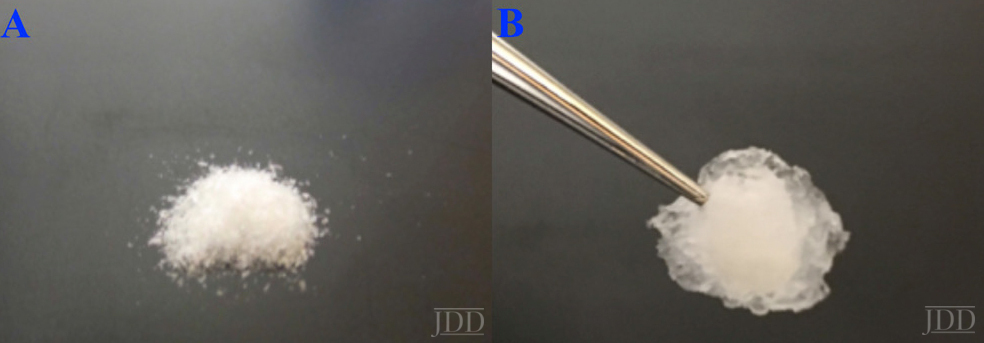
Polymerized methacrylate powder dressings are a novel, sophisticated dressing modality with great potential in the management of wounds following cutaneous surgery. The dressing used in this case was a lyophilized, sterile powder consisting of 84.8% poly-2-hydroxyethylmethacrylate, 14.9% poly-2-hydroxypropylmethacrylate (pHPMA), and 0.3% sodium deoxycholate. These hydrophilic polymers have a covalent methacrylate backbone with a hydroxyl aliphatic side chain. When saline or wound exudate contacts the powder, the spheres hydrate and non-reversibly aggregate to form a moist, flexible dressing that conforms to the topography of the wound and seals it (Figure 2).1
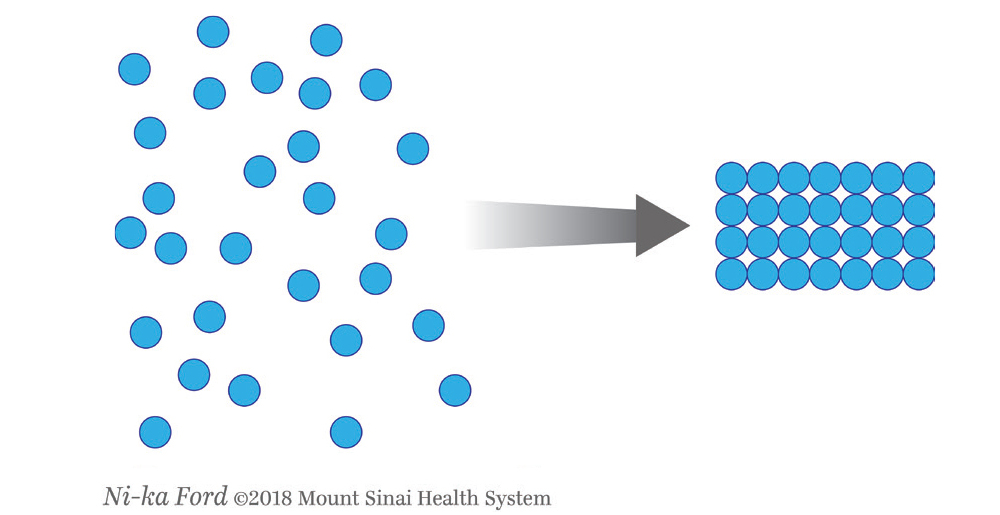
Once the spheres have aggregated, they are designed to orientate in a honeycomb formation with 4-10nm openings (Figure 3) that serve as capillary channels. This porous architecture of the polymer is essential for adequate moisture management, as it allows for vapor transpiration at a rate of 12 l/m2 per day. This ensures the capillary flow from the moist wound surface is distributed evenly through the dressing, which contributes to its 68% water content. Notably, this approximately 3/5 water composition is similar to the water makeup of human skin. Optimized moisture management is theorized to enhance epithelial migration, stimulate angiogenesis, retain growth factors, promote autolytic debridement, and maintain ideal voltage and oxygen gradients for wound healing. The risk of infection is not increased by the existence of these pores, as their small size does not allow for bacterial migration.1
Conclusion
This case demonstrates the effectiveness of a polymerized methacrylate powder dressing to promote timely wound healing of a nasal alar defect. This low maintenance, single-application, user-friendly dressing spared the patient the inconvenience and pain associated with more conventional primary and secondary dressings. The dressing was well tolerated and resulted in a 90% reduction in wound size.
Further studies are needed to investigate the utility of this promising technology.
References
- Fitzgerald RH, Bharara M, Mills JL, Armstrong DG. Use of a Nanoflex powder dressing for wound management following debridement for necrotising fasciitis in the diabetic foot. Int Wound J. 2009;6(2):133–9.
Source:
Matthew J. Lin MD, Danielle P. Dubin BA, Aaron S. Farberg MD, Hooman Khorasani MD, David A. Kriegel MD, (2019). Methacrylate Polymer Powder Dressing for a Nasal Surgical Defect. Journal of Drugs in Dermatology, 18(12), 1274-1275. https://jddonline.com/articles/dermatology/S1545961619P0472X/3/
Content and images used with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
Did you enjoy this case report? Find more here.
Next Steps in Derm is brought to you by SanovaWorks.