Psoriasis is one of the most common immune-mediated inflammatory dermatoses, with increasing evidence for systemic comorbidities. Targeted systemic agents have revolutionized the management of moderate-to-severe psoriasis, with life-changing outcomes for many patients with the chronic disease. Injectable biologics, blocking interleukin (IL)-23 or IL-17 cytokine pathways, have become invaluable options. However, various high-impact subtypes of psoriasis, such as scalp and palmoplantar involvement, can be recalcitrant to combinations of advanced systemic and topical therapies. We continue our series, Therapeutic Cheat Sheet, with a closer look at deucravacitinib, which is approved by the United States Food and Drug Administration for adults with plaque psoriasis. Deucravacitinib is also used off-label for patients with cutaneous lupus and oral lichen planus.
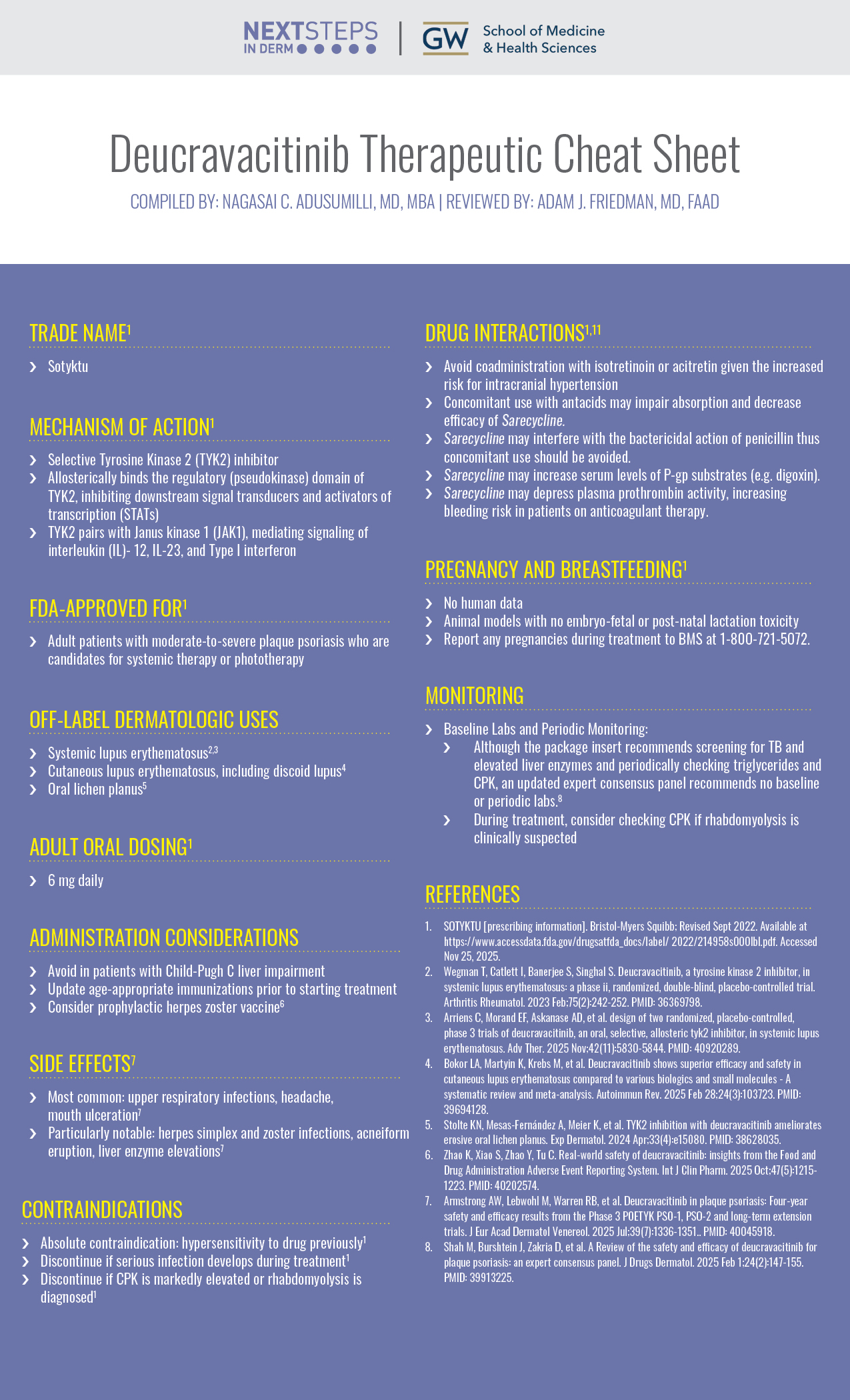
Deucravacitinib Therapeutic Cheat Sheet
Compiled by: Nagasai C. Adusumilli, MD, MBA | Reviewed by: Adam J. Friedman, MD, FAAD
TRADE NAME1
-
- Sotyktu
MECHANISM OF ACTION1
-
- Selective Tyrosine Kinase 2 (TYK2) inhibitor
- Allosterically binds the regulatory (pseudokinase) domain of TYK2, inhibiting downstream signal transducers and activators of transcription (STATs)
- TYK2 pairs with Janus kinase 1 (JAK1), mediating signaling of interleukin (IL)- 12, IL-23, and Type I interferon
FDA-APPROVED FOR1
-
- Adult patients with moderate-to-severe plaque psoriasis who are candidates for systemic therapy or phototherapy
OFF-LABEL DERMATOLOGIC USES
-
- Systemic lupus erythematosus2,3
- Cutaneous lupus erythematosus, including discoid lupus4
- Oral lichen planus5
ADULT ORAL DOSING1
-
- 6 mg daily
ADMINISTRATION CONSIDERATIONS
-
- Avoid in patients with Child-Pugh C liver impairment
- Update age-appropriate immunizations prior to starting treatment
- Consider prophylactic herpes zoster vaccine6
SIDE EFFECTS
-
- Most common: upper respiratory infections, headache, mouth ulceration7
- Particularly notable: herpes simplex and zoster infections, acneiform eruption, liver enzyme elevations7
CONTRAINDICATIONS
-
- Absolute contraindication: hypersensitivity to drug previously1
- Discontinue if serious infection develops during treatment1
- Discontinue if CPK is markedly elevated or rhabdomyolysis is diagnosed1
PREGNANCY AND BREASTFEEDING1
-
- No human data
- Animal models with no embryo-fetal or post-natal lactation toxicity
- Report any pregnancies during treatment to BMS at 1-800-721-5072.
MONITORING
Baseline Labs and Periodic Monitoring:
-
- Although the package insert recommends screening for TB and elevated liver enzymes and periodically checking triglycerides and CPK, an updated expert consensus panel recommends no baseline or periodic labs.8
- During treatment, consider checking CPK if rhabdomyolysis is clinically suspected
FURTHER READING
If you would like to learn more about deucravacitinib, check out the following articles in the Journal of Drugs in Dermatology:
Patel, A. Hetzel, S. Park, et al
Abstract
Background: Plaque psoriasis of the scalp, a common psoriasis location, remains difficult to manage. The comparative efficacy of newer oral agents, such as deucravacitinib, versus traditional first-generation biologics has not been characterized in the treatment of scalp psoriasis. This study indirectly compared the long-term efficacy of deucravacitinib versus that of adalimumab for the treatment of scalp psoriasis.
Methods: A literature review identified trial publications reporting long-term efficacy (≥48 weeks) of adalimumab in patients with scalp psoriasis. Based on a feasibility assessment, summary-level adalimumab data (VOYAGE 1 trial [NCT02207231]) were deemed suitable for comparison to patient-level deucravacitinib data (POETYK PSO-1 trial [NCT03624127]). Unadjusted analyses and adjusted analyses using an unanchored matching-adjusted indirect comparison (MAIC) approach were used to describe and compare baseline characteristics and efficacy outcomes in terms of rates of achievement of clear or almost clear scalp psoriasis (scalp-specific Physician Global Assessment score of 0/1 [ss-PGA 0/1]) at weeks 16, 24, and 48.
Results: Cross-trial differences were observed in age, race, severe scalp psoriasis, and quality of life scores. A larger percentage of patients achieved ss-PGA 0/1 at week 48 with deucravacitinib (unadjusted: 76.7%; adjusted: 73.0%) versus adalimumab (60.5%). Similarly, a larger percentage of patients achieved ss-PGA 0/1 at weeks 16 and 24 with deucravacitinib versus adalimumab.
Conclusions: In this study, treatment with deucravacitinib was effective in treating scalp psoriasis and, when compared with adalimumab, was also associated with a larger percentage of patients achieving ss-PGA 0/1 over 48 weeks.
J Drugs Dermatol. 2025;24(8):788.
Shah, J. Burshtein, D. Zakria, et al.
Abstract
Background: Psoriasis is a chronic, inflammatory disease associated with numerous negative physical and psychosocial impacts. Deucravacitinib is a novel, selective TYK2 inhibitor approved by the FDA for the treatment of moderate-to-severe plaque psoriasis in adults. Deucravacitinib has established efficacy and safety through several clinical trials, but many clinicians are unfamiliar with its safety profile given the lack of formal guidelines. Thus, this expert consensus panel aims to provide clinical recommendations on the efficacy, safety, and appropriate laboratory monitoring for deucravacitinib.
Methods: A comprehensive literature search of PubMed, Scopus, and Google Scholar was completed for English-language original research articles on the efficacy and safety of deucravacitinib. A panel of 10 dermatologists with expertise in managing psoriasis reviewed the relevant literature and crafted consensus statements regarding the efficacy, safety, and recommended laboratory monitoring for deucravacitinib. Using a modified Delphi process, each statement received supermajority approval and was assigned a strength of recommendation using the Strength of Recommendation Taxonomy (SORT) criteria.
Results: The literature search resulted in 101 articles that met search criteria. After screening the articles for relevance to the discussion topic, 14 articles were selected and distributed to the panelists for review prior to the roundtable discussion. The panel unanimously voted to adopt 6 consensus statements and recommendations, 5 of which were given a strength of “A,” 0 were given a strength of “B,” and 1 was given a strength of “C.”
Conclusion: Deucravacitinib is an effective treatment for plaque psoriasis that is well-tolerated and has an excellent safety profile. The 6 consensus statements created by the panel provide expert recommendations regarding the efficacy, safety, and appropriate laboratory monitoring for deucravacitinib. The expert panel also concludes that deucravacitinib has a superior safety profile to traditional JAK inhibitors. After reviewing the clinical trials, the panel did not find evidence of a causal role for deucravacitinib in inducing laboratory abnormalities and did not recommend baseline and ongoing laboratory monitoring for patients treated with deucravacitinib.
J Drugs Dermatol. 2025;24(2):147-155.
REFERENCES
-
- SOTYKTU [prescribing information]. Bristol-Myers Squibb; Revised Sept 2022. Available at https://www.accessdata.fda.gov/drugsatfda_docs/label/ 2022/214958s000lbl.pdf. Accessed Nov 25, 2025.
- Wegman T, Catlett I, Banerjee S, Singhal S. Deucravacitinib, a tyrosine kinase 2 inhibitor, in systemic lupus erythematosus: a phase ii, randomized, double-blind, placebo-controlled trial. Arthritis Rheumatol. 2023 Feb;75(2):242-252. PMID: 36369798.
- Arriens C, Morand EF, Askanase AD, et al. design of two randomized, placebo-controlled, phase 3 trials of deucravacitinib, an oral, selective, allosteric tyk2 inhibitor, in systemic lupus erythematosus. Adv Ther. 2025 Nov;42(11):5830-5844. PMID: 40920289.
- Bokor LA, Martyin K, Krebs M, et al. Deucravacitinib shows superior efficacy and safety in cutaneous lupus erythematosus compared to various biologics and small molecules – A systematic review and meta-analysis. Autoimmun Rev. 2025 Feb 28;24(3):103723. PMID: 39694128.
- Stolte KN, Mesas-Fernández A, Meier K, et al. TYK2 inhibition with deucravacitinib ameliorates erosive oral lichen planus. Exp Dermatol. 2024 Apr;33(4):e15080. PMID: 38628035.
- Zhao K, Xiao S, Zhao Y, Tu C. Real-world safety of deucravacitinib: insights from the Food and Drug Administration Adverse Event Reporting System. Int J Clin Pharm. 2025 Oct;47(5):1215-1223. PMID: 40202574.
- Armstrong AW, Lebwohl M, Warren RB, et al. Deucravacitinib in plaque psoriasis: Four-year safety and efficacy results from the Phase 3 POETYK PSO-1, PSO-2 and long-term extension trials. J Eur Acad Dermatol Venereol. 2025 Jul;39(7):1336-1351.. PMID: 40045918.
- Shah M, Burshtein J, Zakria D, et al. A Review of the safety and efficacy of deucravacitinib for plaque psoriasis: an expert consensus panel. J Drugs Dermatol. 2025 Feb 1;24(2):147-155. PMID: 39913225.
Did you enjoy this Therapeutic Cheat Sheet? You can find more here.

