Metronidazole is a nitroimidazole with antiprotozoal, antibacterial, and anti-inflammatory properties and is available in oral and topical formulations. The diverse mechanisms of action of metronidazole have expanded its utility across various dermatologic conditions. Topical metronidazole is well tolerated and has demonstrated improvements in inflammatory papules and pustules of rosacea. We continue our series, Therapeutic Cheat Sheet, with a closer look at topical metronidazole, which is FDA-approved for rosacea.
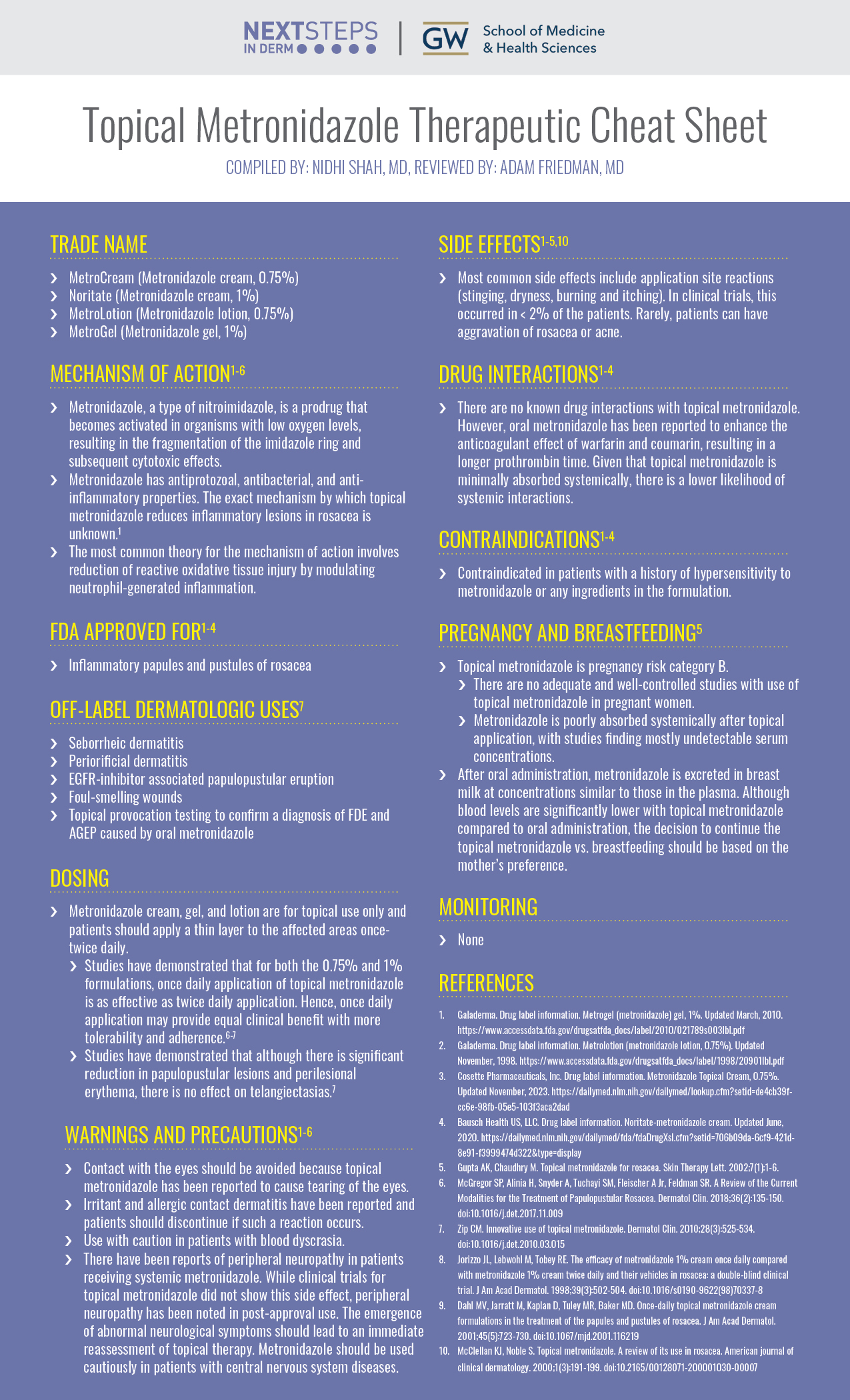
Topical Metronidazole Therapeutic Cheat Sheet
Compiled by: Nidhi Shah, MD, Reviewed by: Adam Friedman, MD
TRADE NAME
-
- MetroCream (Metronidazole cream, 0.75%)
- Noritate (Metronidazole cream, 1%)
- MetroLotion (Metronidazole lotion, 0.75%)
- MetroGel (Metronidazole gel, 1%)
MECHANISM OF ACTION1-6
-
- Metronidazole, a type of nitroimidazole, is a prodrug that becomes activated in organisms with low oxygen levels, resulting in the fragmentation of the imidazole ring and subsequent cytotoxic effects.
- Metronidazole has antiprotozoal, antibacterial, and anti-inflammatory properties. The exact mechanism by which topical metronidazole reduces inflammatory lesions in rosacea is unknown.1
- The most common theory for the mechanism of action involves reduction of reactive oxidative tissue injury by modulating neutrophil-generated inflammation.
FDA APPROVED FOR1-4
-
- Inflammatory papules and pustules of rosacea
OFF-LABEL DERMATOLOGIC USES7
-
- Seborrheic dermatitis
- Periorificial dermatitis
- EGFR-inhibitor associated papulopustular eruption
- Foul-smelling wounds
- Topical provocation testing to confirm a diagnosis of FDE and AGEP caused by oral metronidazole
DOSING
-
- Metronidazole cream, gel, and lotion are for topical use only and patients should apply a thin layer to the affected areas once-twice daily.
- Studies have demonstrated that for both the 0.75% and 1% formulations, once daily application of topical metronidazole is as effective as twice daily application. Hence, once daily application may provide equal clinical benefit with more tolerability and adherence.6-7
- Studies have demonstrated that although there is significant reduction in papulopustular lesions and perilesional erythema, there is no effect on telangiectasias.7
- Metronidazole cream, gel, and lotion are for topical use only and patients should apply a thin layer to the affected areas once-twice daily.
WARNINGS AND PRECAUTIONS1-6
-
- Contact with the eyes should be avoided because topical metronidazole has been reported to cause tearing of the eyes.
- Irritant and allergic contact dermatitis have been reported and patients should discontinue if such a reaction occurs.
- Use with caution in patients with blood dyscrasia.
- There have been reports of peripheral neuropathy in patients receiving systemic metronidazole. While clinical trials for topical metronidazole did not show this side effect, peripheral neuropathy has been noted in post-approval use. The emergence of abnormal neurological symptoms should lead to an immediate reassessment of topical therapy. Metronidazole should be used cautiously in patients with central nervous system diseases.
SIDE EFFECTS1-5,10
-
- Most common side effects include application site reactions (stinging, dryness, burning and itching). In clinical trials, this occurred in < 2% of the patients. Rarely, patients can have aggravation of rosacea or acne.
DRUG INTERACTIONS1-4
-
- There are no known drug interactions with topical metronidazole. However, oral metronidazole has been reported to enhance the anticoagulant effect of warfarin and coumarin, resulting in a longer prothrombin time. Given that topical metronidazole is minimally absorbed systemically, there is a lower likelihood of systemic interactions.
CONTRAINDICATIONS1-4
-
- Contraindicated in patients with a history of hypersensitivity to metronidazole or any ingredients in the formulation.
PREGNANCY AND BREASTFEEDING5
-
- Topical metronidazole is pregnancy risk category B.
- There are no adequate and well-controlled studies with use of topical metronidazole in pregnant women.
- Metronidazole is poorly absorbed systemically after topical application, with studies finding mostly undetectable serum concentrations.
- After oral administration, metronidazole is excreted in breast milk at concentrations similar to those in the plasma. Although blood levels are significantly lower with topical metronidazole compared to oral administration, the decision to continue the topical metronidazole vs. breastfeeding should be based on the mother’s preference.
- Topical metronidazole is pregnancy risk category B.
MONITORING
-
- None
FURTHER READING
If you would like to learn more about topical metronidazole, check out the following articles in the Journal of Drugs in Dermatology:
Williamson T, LaRose A, Cameron J, et al.
Abstract
Objective: To assess differences in patient-reported treatment side effects and concerns associated with azelaic acid 15% foam (AAF) vs metronidazole cream (MC) and metronidazole gel (MG).
Methods: This study used matching-adjusted indirect comparison (MAIC) to compare patient-reported outcomes from survey data evaluating rosacea treatments. Outcomes of interest included percentages of patients reporting concerns and side effects and measures of importance of the concerns and tolerability of the side effects. Patients in each analysis (MG vs AAF and MC vs AAF) were matched using stabilized inverse propensity scores.
Results: When compared to AAF, MG-treated patients more frequently reported concerns with treatment efficacy (54% vs 4%), application (7% vs 3%), and treatment side effects. MC-treated patients more frequently reported concerns with treatment efficacy (61% vs 5%) and dryness (8% vs 5%). AAF-treated patients more frequently reported concerns with cost of treatment compared with MG (7% vs 1%) and MC (9% vs 4%). Among patients reporting concerns, level of importance associated with these concerns was similar for AAF-treated patients compared with MG- and MC-treated patients. When compared to AAF-treated patients, MG-treated patients more frequently reported side effects of dryness (26% vs 15%) and uneven skin tone (3% vs 0%), and MC-treated patients more frequently reported side effects of burning (7% vs 3%), itching (7% vs 5%), and redness (7% vs 5%). MG- and MC-treated patients indicated greater intolerance for reported side effects than AAF-treated patients.
Conclusions: MG- and MC-treated patients more frequently reported treatment concerns and side effects than AAF-treated patients, and tolerability of those side effects was higher for patients treated with AAF. While treatment cost is a more frequent concern in patients treated with AAF, these patients less frequently reported concerns with treatment efficacy and reported similar or greater tolerance to side effects than patients treated with either MC or MG.
J Drugs Dermatol. 2020;19(3):295-304.
Topical Rosacea Therapy: The Importance of Vehicles for Efficacy, Tolerability and Compliance
Jackson JM, Pelle M.
Abstract
Many topical medications are available for the treatment of papulopustular rosacea. While treatments contain metronidazole, azelaic acid, or sodium sulfacetamide-sulfur as the active ingredient, the composition of the vehicle formulations varies widely. These vehicles come in gels, creams, lotions and foams; some ingredients are common to many vehicles, while some vehicles contain unique ingredients designed to optimize skin penetration and delivery of the active drug to its target. Vehicles can also influence tolerability, which is always a concern in patients with heightened skin sensitivity, and compliance, which is typically lower for topical treatments than oral treatments. Ideally, the vehicle of any rosacea treatment should enhance drug delivery, be nonirritating and be easy to use. Ingredients that help repair barrier function are also desirable. This review will focus on the key components of the vehicles from the most commonly used topical therapies for papulopustular rosacea and how vehicle formulations influence the delivery of active ingredient, skin barrier repair, tolerability and compliance.
J Drugs Dermatol. 2011;10(6):627-633.
REFERENCES
-
- Drug label information. Metrogel (metronidazole) gel, 1%. Updated March, 2010. https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021789s003lbl.pdf
- Drug label information. Metrolotion (metronidazole lotion, 0.75%). Updated November, 1998. https://www.accessdata.fda.gov/drugsatfda_docs/label/1998/20901lbl.pdf
- Cosette Pharmaceuticals, Inc. Drug label information. Metronidazole Topical Cream, 0.75%. Updated November, 2023. https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=de4cb39f-cc6e-98fb-05e5-103f3aca2dad
- Bausch Health US, LLC. Drug label information. Noritate-metronidazole cream. Updated June, 2020. https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=706b09da-6cf9-421d-8e91-f3999474d322&type=display
- Gupta AK, Chaudhry M. Topical metronidazole for rosacea. Skin Therapy Lett. 2002;7(1):1-6.
- McGregor SP, Alinia H, Snyder A, Tuchayi SM, Fleischer A Jr, Feldman SR. A Review of the Current Modalities for the Treatment of Papulopustular Rosacea. Dermatol Clin. 2018;36(2):135-150. doi:10.1016/j.det.2017.11.009
- Zip CM. Innovative use of topical metronidazole. Dermatol Clin. 2010;28(3):525-534. doi:10.1016/j.det.2010.03.015
- Jorizzo JL, Lebwohl M, Tobey RE. The efficacy of metronidazole 1% cream once daily compared with metronidazole 1% cream twice daily and their vehicles in rosacea: a double-blind clinical trial. J Am Acad Dermatol. 1998;39(3):502-504. doi:10.1016/s0190-9622(98)70337-8
- Dahl MV, Jarratt M, Kaplan D, Tuley MR, Baker MD. Once-daily topical metronidazole cream formulations in the treatment of the papules and pustules of rosacea. J Am Acad Dermatol. 2001;45(5):723-730. doi:10.1067/mjd.2001.116219
- McClellan KJ, Noble S. Topical metronidazole. A review of its use in rosacea. American journal of clinical dermatology. 2000;1(3):191-199. doi:10.2165/00128071-200001030-00007
Did you enjoy this Therapeutic Cheat Sheet? You can find more here.