Chemical peeling is one of the oldest resurfacing procedures used in dermatology, and it is still the most popular. Why the staying power? For reasons such as, ease of use, versatility, and low cost have helped maintain chemical peels as a cornerstone of the aesthetic repertoire. In this two-part primer, I’ll review the basics of chemical peels including agents used, techniques and potential complications.
Basic Principles
At its core, chemical peeling is the use of a chemical agent to ablate the skin surface in a controlled fashion. Once the skin has regenerated, it will have improved appearance and texture. This technique can be used to treat rhytides, dyschromia, acne, actinic keratoses and whole host of other conditions and cosmetic concerns.
Peels can be classified by their depth:
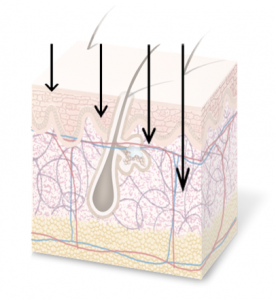
Superficial peels – ablation of the epidermis to the upper papillary dermis. Superficial peels require little to no down time, though they may need to be repeated several times to see full results.
Medium depth peels – ablation reaches anywhere from the papillary dermis down to the upper reticular dermis. They require about 1 week of down time.
Deep peels – ablation to the mid reticular dermis. They require 2-3 weeks of down time. Deep peels provide the most dramatic results, though their use has largely fallen out of favor.
Common Peeling Agents
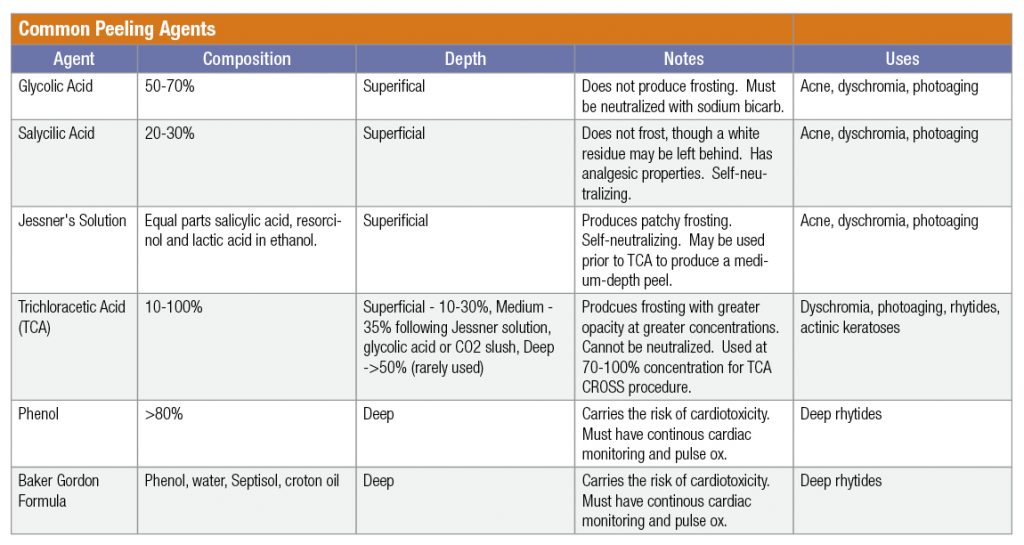
Click here to download a PDF version of the Chemical Peels Agents Table.
Potential complications
Chemical resurfacing is generally very safe when performed with the correct technique. However, there are several risks which must be kept in mind. These include scarring (especially when performed on the neck), dyschromia (especially in phototypes III-VI), infection, herpes reactivation and persistent erythema.
History Taking
A thorough history and physical exam will help guide you in your choice of the proper peeling agent. For instance, special attention should be paid to the patient’s smoking history. Smoking will impede healing following the procedure, (especially for medium and deep peels). It would also be key to note a history of keloid formation, history of herpes labialis or inflammatory disorders of the skin.
Patients who have undergone rhytidectomy in the past 6 months will likely have poor wound healing after a chemical peel.
Classically, it has been recommended that peels be withheld after a course of isotretinoin for 6-12 months, though expert opinions vary when it comes to this timeframe.
Patients who have been exposed to radiation should be examined for the presence of pilosebaceous units in the area to be treated, as they are necessary for proper healing.
Preparation
Prior to chemical peeling, complementary procedures such as botulinum toxin injection for rhytids can be considered. Topical retinoids can also be used leading up to a peel in order to augment the peel’s effect, as they will help increase exfoliation. Patients with dyschromia or at risk for dyschromia should be given hydroquinone cream to use in the weeks leading up to their peel. If a patient has a history of herpes labialis or if they are undergoing a medium or deep peel, regardless of HSV status, they should be prescribed a 10-14-day course of antivirals to start on the day of their peel. Another key item to mention to patients is that they should not wear contact lenses or jewelry on the day of the procedure.
For patients at risk for dyschromia, such as phototypes III-VI, a test spot can be treated along the lateral hairline in advance of the procedure evaluate the likely response to the peel.
Patients should use light skincare and apply no makeup on the day of their peel.
Stay tuned for part 2, where I’ll be discussing technique and aftercare.
References:
Monheit, G.D. & Chastain, M.A.. (2008). Chemical and mechanical skin resurfacing. Dermatology. 2313-2328.
O’Connor, A. A., Lowe, P. M., Shumack, S. and Lim, A. C. (2018), Chemical peels: A review of current practice. Australas J Dermatol, 59: 171-181. doi:10.1111/ajd.12715
Did you enjoy this post? Find other articles on Aesthetic Derm Topics by clicking here.