INTRODUCTION
Linear lichen planus pigmentosus (LPP) of the face is a rare acquired variant of lichen planus, with only a few cases published in the literature.1 It is an inflammatory condition with unknown etiology, characterized by blue-gray hyperpigmented macules, and tends to affect sun-exposed areas of the head and neck.1-4 The pathophysiology of linear LPP is poorly understood, though it is postulated to be caused by T-lymphocyte autoimmunity against keratinocytes.5-7 Linear LPP more frequently affects middle aged women and skin phototypes III to VI.1,3 It has also been proposed to be associated with hepatitis C infection, ultraviolet (UV) radiation, and contact allergens.1,3,8 Treatment for linear LPP is difficult and there is no established first-line therapy; however, tacrolimus ointment, topical corticosteroids, and various systemic agents are effective in improving the appearance.3,8,9
Linear LPP tends to show a unilateral distribution and can present along the lines of Blashko and in areas of koebnerization. Prior reports have characterized linear LPP that follows the lines of Blashko as more commonly affecting the trunk. Only 3 cases of linear LPP of the face have been reported in the literature.1
We present 3 cases of linear lichen planus pigmentosus of the forehead along the lines of Blashko, a unique presentation of linear LPP of the face. One of our cases also provides supporting evidence for tacrolimus as a preferred therapy. To our knowledge, this case series is the largest case series of linear LPP of the forehead to be reported. We review the literature, clinical presentation, and management options available for this entity.
CASE REPORTS
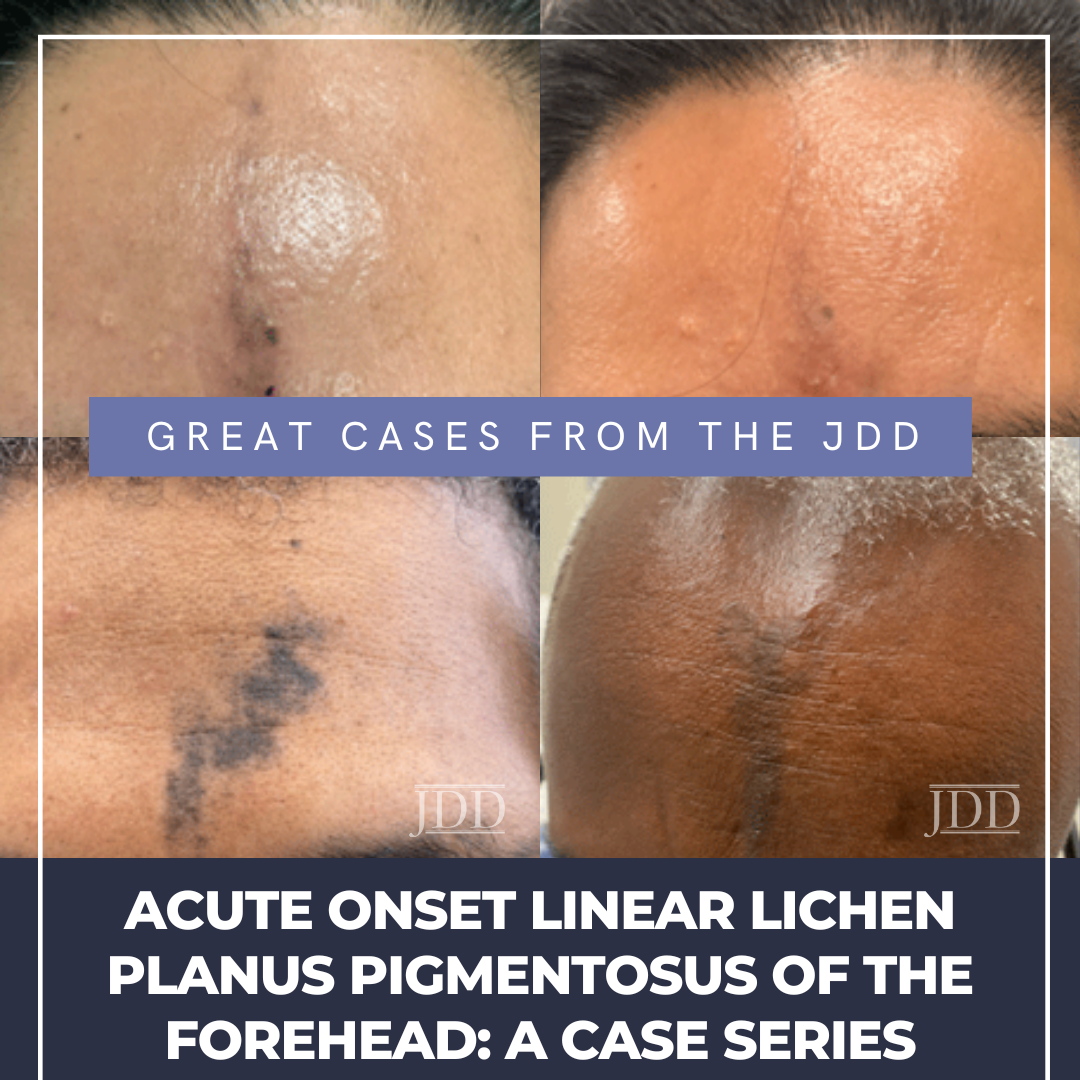
A 48-year-old man presented to the Ronald O. Perelman Department of Dermatology at NYU Grossman School of Medicine with a chief concern of 5 months of forehead discoloration (Figure 1). He denied itch, pain, and preceding trauma to the forehead. He had been using
Jamaican black castor oil on the affected area without significant symptom improvement, and denied use of lightening creams. Past medical history was negative for hepatitis C or dental amalgams, and the patient did not take any medications or supplements. Physical examination revealed brownish-black hyperpigmented macules coalescing into small patches with subtle scale extending in linear fashion from the medial forehead to the glabella. The biopsy revealed a perifollicular and epidermal band-like lymphocytic infiltrate with interface changes and melanophages in the dermis. The patient was diagnosed with LPP.
 Case 2
Case 2A 49-year-old man presented to the Ronald O. Perelman Department of Dermatology with a history of skin discoloration on the forehead for 3 to 4 months (Figure 2). The patient saw another dermatologist at an outside institution, and had a shave biopsy performed. The biopsy showed a lymphocyte-mediated vacuolar interface dermatitis. Clinical exam revealed blue-gray hyperpigmented patches in a semi-linear distribution on the forehead. Based on clinical morphology and biopsy findings, he was given a presumed diagnosis of LPP.
 Case 3
Case 3A 45-year-old Hispanic woman presented to the Ronald O. Perelman Department of Dermatology with a 4-month history of a linear discoloration on her forehead (Figure 3). The discoloration started as a small patch and increased in size vertically. The patient denied pain or trauma to the area; however, mild pruritus and burning were present. The patient took iron for mild anemia, but was otherwise healthy. The biopsy revealed a perifollicular band-like lymphocytic infiltrate with interface changes, focal accentuation of the granular layer, and melanophages in the dermis. The patient was diagnosed with LPP and treated with tacrolimus 0.1% ointment twice daily for 7 months with notable improvement (Figure 4). She later developed frontal hairline involvement with mild perifollicular scaling and underwent treatment with intralesional triamcinolone at 2.5mg/mL.
 DISCUSSION
DISCUSSION
Lichen planus pigmentosus is an inflammatory condition that is a subset of lichen planus.1 LPP has been associated with other variants of lichen planus in about one-third of the cases reported, specifically with frontal fibrosing alopecia (FFA).3 More than 50% of patients diagnosed with FFA previously had LPP, often months to years before the onset of FFA.10 Multiple morphologies of LPP exist, such as diffuse, reticular, blotchy, perifollicular, annular, and linear, and they are not mutually exclusive.7 The linear morphology of LPP is rare, and can present in a Blashkoid, segmental, or zosteriform distribution.1,11-13 The presentation of linear LPP along the lines of Blashko has been proposed to be associated with susceptibility to genetic mosaicisms, which determine cell populations with distinct immunological and antigenic properties.1,3,7,9,11
While the etiology of linear LPP is largely unknown, some have proposed that this entity is a response to exposure to contact allergens such as nickel, henna and hair dye, mustard oil, and sandalwood oil. Linear LPP tends to affect middle-aged women, and typically affects individuals of skin phototypes III to IV, along with individuals of Latin American, Asian, and Middle Eastern heritage.1,3,14 The pathophysiology of linear LPP is also poorly understood, though it has been postulated to be caused by T-lymphocyte autoimmunity against keratinocytes.1,5 Clinically, patients present with blue-grey hyperpigmented patches, with or without pruritus, and without secondary changes such as scarring or atrophy.1,3,7
The main differential diagnosis for this clinical presentation includes erythema dyschromicum perstans (EDP) – of which there is significant clinical overlap – along with linear lichen planopilaris, linear atrophoderma of Moulin, and linear morphea.1,7,15 EDP, like LPP, can present with gray-blue macules
with or without raised erythematous borders, often without pruritis, and presents in patients of darker skin phototypes.7 EDP, however, tends to present on sun-protected areas of the skin like the trunk rather than on sun-exposed areas of the face and neck as seen in LPP, and tends to have erythematous borders.2-4,7 Linear lichen planopilaris tends to resolve with atrophy and presents with scaly, red-brown hyperpigmentation, while the hyperpigmentation of LPP is more of a blue-gray and does not resolve with secondary changes.1,16,17 While linear LPP of the face tends to affect middle-aged women, linear atrophoderma of Moulin typically affects children, and affected areas tend to be located on the trunk and extremities.7,17 Lastly, linear morphea tends to present with skin sclerosis, which is not seen in linear LPP of the face.17
Prior reports have demonstrated that LPP more commonly affects sun-exposed areas of the head and neck, and only 3 cases of Blashkoid linear LPP of the face have been reported.1,18,19 Our 3 cases thus demonstrate a unique and novel presentation of linear LPP of the face; all 3 patients presented with linear lichen pigmentosus of the forehead following the lines of Blashko without any notable preceding trauma or exposure to contact allergens. The clinical presentation appeared along the lines of Blashko on the face, which has not been well-documented in the literature. It is uncertain as to whether linear LPP of the forehead along the lines of Blashko is a separate entity or a rare subvariant of linear LPP.
Linear LPP is difficult to treat and does not have an established first-line therapy. Treatment consists of avoiding triggers such as UV radiation and contact allergens, and using topical and systemic therapies to reduce inflammation. Among these treatments, tacrolimus has been demonstrated as an effective agent to accelerate the healing process and has been reported to produce 50% improvement in 12 weeks when given as 0.03% or 0.1% ointment.7,8,20 A wide range of other therapeutics have been also employed with varying rates of efficacy. Medium to high potency topical corticosteroids can accelerate the healing process but have been predominately used in cases of LPP inversus.7,20 Depigmentation agents such as 4% hydroquinone, Kojic acid, and a combination of tretinoin 0.025% to 0.05% and hydroquinone 4% have been employed as an adjuvant therapy with an anti-inflammatory agent to decrease hyperpigmentation.7,18,21,22 Q-switched laser (1064 nm Nd-YAG) has been used every 3 weeks for up to 4 months, but efficacy is variable.7,23 Anti-inflammatory agents such as dapsone and oral corticosteroids have been used in combination with tacrolimus; however, clinicians must be mindful of side effects such as hemolysis from dapsone and numerous systemic effects from prolonged oral corticosteroids.7,24-26 Lastly, isotretinoin has been shown to be effective with 27% of 27 patients improving greater than 50%, and an additional 50% to 55% of patients showing 25% to 50% improvement after 20mg or 3mg daily for 6 months.7,27
One of our cases supports the use of tacrolimus as an effective treatment for linear LPP of the face. While 2 of our cases were lost to follow up, our third case was treated with tacrolimus 0.1% ointment twice daily for 7 months and showed remarkable improvement. Although the treatment of tacrolimus was positive in this case, more research is needed to establish tacrolimus as a preferred therapy for linear LPP of the forehead.
To our knowledge, this is the largest reported series of linear LPP of the forehead. We report that treatment with tacrolimus can lead to significant reduction in the size, pigmentation, and erythema of the affected region, which is consistent with prior reported cases of facial linear LPP. More research is needed, however, to determine whether linear LPP of the face along the lines of Blashko is its own entity or a subvariant of linear LPP.
It is also notable that while there have been 3 well-documented cases of linear LPP of the face along the lines of Blashko reported in the literature over the span of 30 years,3 we have seen 3 cases of linear LPP of the face in the past 18 months, suggesting a potential rise in incidence. As such, it is important that we learn more about the treatment and classification of linear LPP of the face to most effectively reduce the medical and cosmetic sequelae of this phenomenon.
DISCLOSURES
REFERENCES
2. Ghosh A, Coondoo A. Lichen planus pigmentosus: the controversial consensus. Indian J Dermatol. 2016;61(5):482-486.
3. Kennedy AM, Muhaj FF, Tschen JA, Silapunt S. Linear lichen planus pigmentosus of the face with histological findings of lichen planopilaris – an uncommon variant of lichen planus. Dermatol Online J. 2021;27(4). Epub 20210415.
4. Kumarasinghe SPW, Pandya A, Chandran V, et al. A global consensus statement on ashy dermatosis, erythema dyschromicum perstans, lichen planus pigmentosus, idiopathic eruptive macular pigmentation, and Riehl’s melanosis. Int J Dermatol. 2019;58(3):263-272. Epub 20180903.
5. Chieregato C, Zini A, Barba A, Magnanini M, Rosina P. Lichen planopilaris: report of 30 cases and review of the literature. Int J Dermatol. 2003;42(5):342- 345.
6. Lyakhovitsky A, Amichai B, Sizopoulou C, Barzilai A. A case series of 46 patients with lichen planopilaris: demographics, clinical evaluation, and treatment experience. J Dermatolog Treat. 2015;26(3):275-279. Epub 20140701.
7. Robles-Méndez JC, Rizo-FrÃas P, Herz-Ruelas ME, Pandya AG, Ocampo Candiani J. Lichen planus pigmentosus and its variants: review and update. Int J Dermatol. 2018;57(5):505-514. Epub 20171026.
8. Al-Mutairi N, El-Khalawany M. Clinicopathological characteristics of lichen planus pigmentosus and its response to tacrolimus ointment: an open label, non-randomized, prospective study. J Eur Acad Dermatol Venereol. 2010;24(5):535-540. Epub 20091015.
9. Tziotzios C, Brier T, Lee JYW, et al. Lichen planus and lichenoid dermatoses: conventional and emerging therapeutic strategies. J Am Acad Dermatol. 2018;79(5):807-818.
10. Berliner JG, McCalmont TH, Price VH, Berger TG. Frontal fibrosing alopecia and lichen planus pigmentosus. J Am Acad Dermatol. 2014;71(1):e26-e27.
11. Vineet R, Sumit S, K GV, Nita K. Lichen planus pigmentosus in linear and zosteriform pattern along the lines of Blaschko. Dermatol Online J. 2015;21(10). Epub 20151016.
13. Weston G, Payette M. Update on lichen planus and its clinical variants. Int J Womens Dermatol. 2015;1(3):140-149. Epub 20150916.
14. Cobos G, Kim RH, Meehan S, Elbuluk N. Lichen planus pigmentosus and lichen planopilaris. Dermatol Online J. 2016;22(12). Epub 20161215.
15. Asz-Sigall D, González-de-Cossio-Hernández AC, Rodríguez-Lobato E, et al. Linear Lichen Planopilaris of the Face: Case Report and Review. Skin Appendage Disord. 2016;2(1-2):72-75. Epub 20160825.
16. Cañadas NG, Luna PC, Etcheverry MD, et al. Liquen plano pilar lineal de la cara. [Linear lichen planopilaris of the face]. Dermatol Online J. 2010;16(7):11. Epub 20100715.
17. Zhao N, Qu T. Linear lichen planopilaris of the face. Eur J Dermatol. 2012;22(5):691-692.
18. Sonthalia S, Das A, Sharma S. Co-localization of linear lichen planus pigmentosus and milia in a child. Indian J Dermatol. 2016;61(2):237.
19. Seo JK, Lee HJ, Lee D, Choi JH, Sung HS. A case of linear lichen planus pigmentosus. Ann Dermatol. 2010;22(3):323-325. Epub 20100805.
20. Dizen Namdar N, Kural E, Pulat O, Metineren MH, Sarici G. Lichen planus pigmentosus-inversus: 5 Turkish cases. J Eur Acad Dermatol Venereol. 2016;30(3):450-452. Epub 20141103.
21. Kumar YH, Babu AR. Segmental lichen planus pigmentosus: an unusual presentation. Indian Dermatol Online J. 2014;5(2):157-159. 22. Dlova NC. Frontal fibrosing alopecia and lichen planus pigmentosus: is there a link? Br J Dermatol. 2013;168(2):439-442. Epub 20121005.
23. Kim JE, Won CH, Chang S, Lee MW, Choi JH, Moon KC. Linear lichen planus pigmentosus of the forehead treated by neodymium:yttrium-aluminumgarnet laser and topical tacrolimus. J Dermatol. 2012;39(2):189-191. Epub 20110927.
24. Muñoz-Pérez MA, Camacho F. Pigmented and reticulated plaques of folds. A case of lichen planus pigmentosus-inversus? Eur J Dermatol. 2002;12(3):282.
25. Verma P, Pandhi D. Topical Tacrolimus and oral dapsone combination regimen in lichen planus pigmentosus. Skinmed. 2015;13(5):351-354. Epub 20151001.
26. Sindhura KB, Vinay K, Kumaran MS, Saikia UN, Parsad D. Lichen planus pigmentosus: a retrospective clinico-epidemiologic study with emphasis on the rare follicular variant. J Eur Acad Dermatol Venereol. 2016;30(11):e142-e144. Epub 20151104.
27. Muthu SK, Narang T, Saikia UN, Kanwar AJ, Parsad D, Dogra S. Low-dose oral isotretinoin therapy in lichen planus pigmentosus: an open-label nonrandomized prospective pilot study. Int J Dermatol. 2016;55(9):1048-1054. Epub 20160407.
SOURCE
Rodriguez, Elijah, et al. “Acute Onset Linear Lichen Planus Pigmentosus of the Forehead: A Case Series.” Journal of Drugs in Dermatology: JDD 22.1 (2023): 94-97.
Content and images used with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
Did you enjoy this JDD case report? You can find more here.