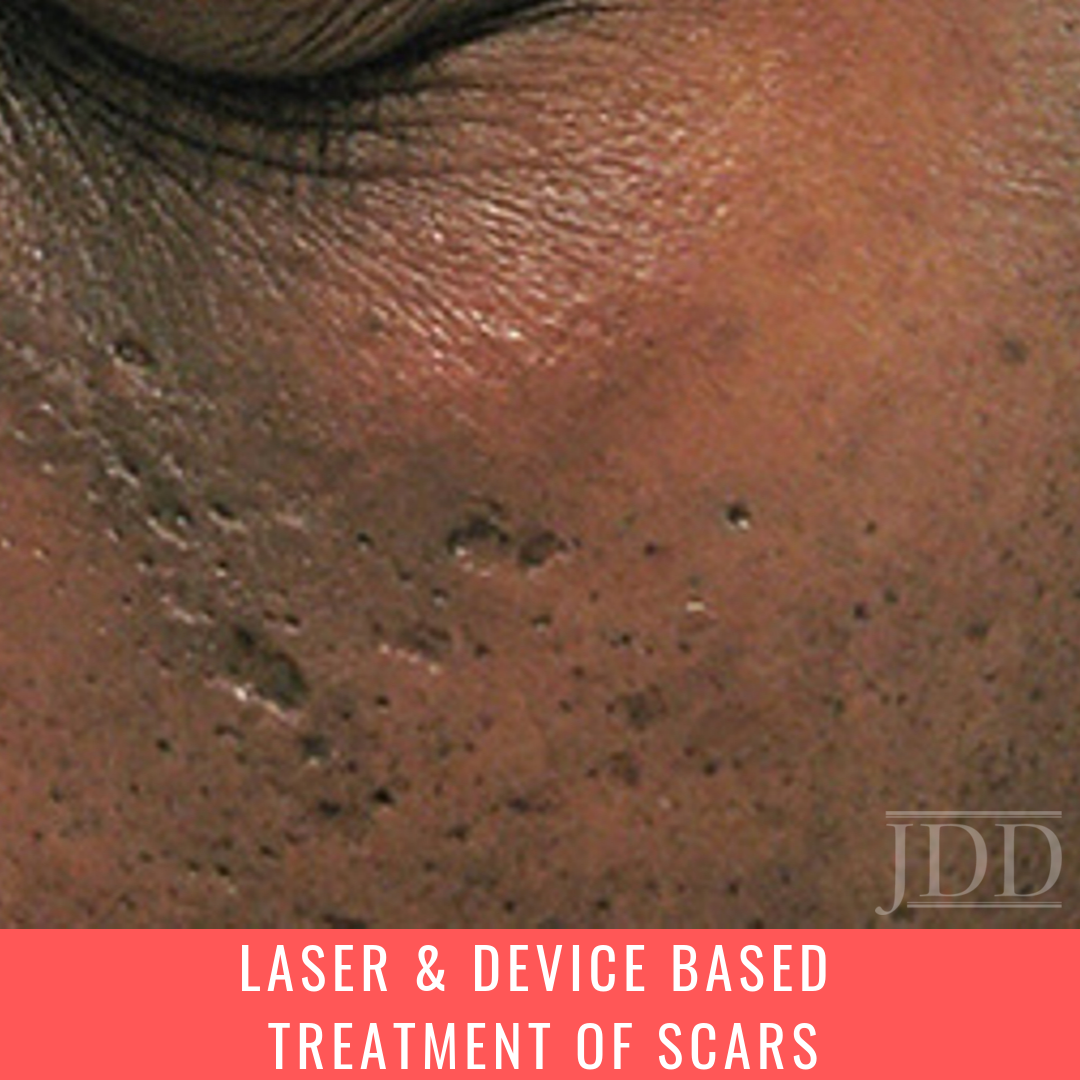
I absorbed Dr. Paul Friedman’s lecture on Laser and Device Based Treatment of Scars at the Skin of Color Update (brain: “Don’t’ say it. Don’t say it. Don’t say it. Don’t say it”)…with laser focus.
Sorry.
But in all seriousness, his lecture was one that I anticipated with particular eagerness, among all of the fantastic lectures that comprised the weekend, for reasons both professional and personal. I’m very interested in lasers and other energy based devices, and hope to incorporate their use into a large part of my future practice. On a more personal level, however, I was looking to hear about options that I can one day use to treat the acne scarring on my face—scarring that is there despite two courses of isotretinoin, scarring that I conceal from the world beneath a chunky layer of bangs overlying my forehead. It is a myth that all dermatologists have perfect skin. In many cases, one’s personal struggles with their skin provides the impetus to seek a career in dermatology, and is a sustaining source of empathy when we see patients who are extremely distressed by the appearance of scars on their face and body, who are unable to confront the world in the manner that they would like, and who may remind us of ourselves. Please read on for some incredible tips that Dr. Paul Friedman shared that can help you improve your patients’ scars, and thereby change their lives.
This article will provide an overview of the following:
- General approach to treating cutaneous scarring with lasers and energy-based devices
- Hypertrophic scars
- Atrophic scars
- Hyperpigmented scars
- Hypopigmented scars
But first, let me share a few of the “A-ha” moments that I experienced during Dr. Paul Friedman’s lecture, in the hope that they will entice you to read on…
- A combination of intralesional 5-fluorouracil and triamcinolone (TAC) has been shown to be as effective as intralesional TAC alone. But what concentrations are we talking about here?
- Not only can PDL treat red, hyperemic scars, but it is also great for hypertrophic scars and keloids—and now I understand why!
- Non-ablative fractional lasers can be a great option in skin of color patients IF you are familiar with the ways in which the risk of treatment-related adverse outcomes can be minimized. These strategies are a must know if you wish to avoid complications!
- Hypopigmented scars have been found to respond well to combination treatment with the 1550-nm erbium-doped laser AND a few well-chosen topicals. Want to find out which ones?
General approach to treating cutaneous scarring with lasers and energy-based devices
Scars come in a wide variety of morphologies, and require a customized, often multi-modal approach to address their color and elevation. Fully or fractionally ablative lasers such as the 10,600-nm CO2 and 2940-nm erbium-doped yttrium aluminum garnet (Er:YAG) are useful for addressing contour changes in depressed and atrophic scars. When the patient is a known keloid former, the Er:YAG may be preferable; by virtue of its being strongly absorbed by water, it yields more superficial ablation, less dermal heating, and fewer effects on collagen remodeling. Non-ablative fractional devices, such as the 1550-nm erbium-doped fiber laser, have a wide variety of applications, and are great option scars for that would benefit from dermal remodeling and collagen induction, such as atrophic scars. Non-ablative lasers leave the stratum corneum intact, while fractionation creates thousands of microthermal zones (MTZ) of tissue injury interspersed with islands of intact tissue to promote rapid wound healing. These lasers have been shown to be safe and effective for various types of scars in Fitzpatrick skin types (FST) I – VI, on the face as well as the neck, trunk, and extremities. For scars that have a component of erythema and hyperemia, lasers that target hemoglobin, such as the 532-nm potassium titanyl phosphate (KTP) and 585- and 595-nm pulsed dye lasers (PDL), are useful. PDL lasers may furthermore be utilized for hypertrophic scars and keloids, as they are capable of reducing both pigmentation and the bulk of scar tissue.
Although long-standing scars will respond to treatment with lasers and other energy-based devices, treatment that is directed at newer scars will likely yield cosmetically superior results. The best timing for treatment initiation, however, remains a subject of debate.
Hypertrophic scars
Hypertrophic scars can be clinically challenging and treatment refractory, and therefore often require a combination approach to treatment that entails intralesional triamcinolone and/or 5-flurouracil (5-FU), as well as PDL. While intralesional triamcinolone (TAC) is commonly used to treat hypertrophic scars and keloids, we have all had patients who have experienced at least some of the undesired side effects of therapy, namely hypopigmentation, cutaneous atrophy, and telangiectasias. A combination of 5-FU (45 mg/mL; 0.9 mL of 50 mg/mL 5-FU) and TAC (1 mg/mL; 0.1 mL of 40 mg/mL) has been shown to be as effective as intralesional TAC 10 mg/mL alone. The combination therapy furthermore yielded results that caused fewer associated side effects and were thereby more cosmetically acceptable to patients.5
One of the most studied devices for the treatment of hypertrophic scars is the 585- or 595 nm PDL. Although how PDL decreases the bulk of hypertrophic scars and keloids is not precisely known, in vitro studies of keloid fibroblasts irradiated with PDL have demonstrated antiproliferative and apoptotic effects.1,2 PDL lasers have also been reported to bring about the regression of hypertrophic scars through the suppression of transforming growth factor-B1, and upregulation of matrix metalloproteinase.3,4 Treatment with low fluence (4.5-6 J/cm2) PDL, with relatively short pulse durations (0.45 – 3-milliseconds), and large spot sizes (10-12 mm) can be performed at 4-6 week intervals. Similar settings can also be employed for the treatment of erythematous, hyperemic scars. In the case of surgical scars, it is possible to start treatment as early as 2-4 weeks after suture removal. Treatment can also be combined with the aforementioned intralesional therapy as needed.
Because melanin is a competing chromophore at wavelengths of 585-595 nm, PDL is not safe to use on Fitzpatrick skin types (FST) V – VI. A more prudent option for hypertrophic scars and keloids in richly pigmented skin is a combination of intralesional 5-FU and TAC with non-ablative fractional resurfacing with a device such as the 1550-nm erbium-doped laser.
Atrophic scars
According to Dr. Friedman, a multimodal approach achieves the best outcome when treating atrophic scars. This approach might entail physical modalities, such as the use of filler on atrophic, distensible scars, subcision for the release of tethered scars, and punch excision or TCA-cross for ice pick scars. The choice of laser that is employed to treat atrophic scars depends on both the morphology of the scar, as well as the patient’s FST. Options include the 1064- or 1320-nm neodymium-doped yttrium aluminum garnet (Nd:YAG), 1450-nm diode, as well as various fully ablative, fractionated ablative, and fractionated non-ablative lasers. Ablative fractionated resurfacing lasers typically yield 50-75% improvement after 2-3 treatment sessions, but their use in FST V-VI patients carries a high risk of complications and is therefore not recommended. Likewise, conventional ablative resurfacing with CO2 or Er:YAG should be avoided in FST V-VI patients for the same reason.
One of the most frequently studied lasers for the treatment of atrophic acne scars is the non-ablative fractionated 1550-nm erbium-doped laser. While this laser has been reported in some studies to yield 51-75% clinical improvement after 3 monthly treatments in FST I-V,6 Dr. Friedman has found that 25-50% improvement after 5 sessions is a realistic outcome to counsel patients on. One of the benefits of this laser is that it can be used for a variety of acne scars—icepick, boxcar, rolling—on facial and extra-facial sites (15 mm handpiece, energy settings of 20-70 mJ/MTZ, treatment levels 7-10, 8-10 passes, 2-6 treatments at 1 month intervals).7
Know that the risk of PIH is greater in FST III+, but that this risk can be mitigated by utilizing lower treatment densities, halving the number of passes per session, doubling the total number of treatments, and increasing the interval between treatments.
Hyperpigmented scars
Post-inflammatory hyperpigmentation is a frequent consequence of scarring, and does not always fade with a tincture of time. The goal of targeting pigmented lesions with lasers is promoting the epidermal extrusion of pigment particles, and in the case of quality-switched (QS) and picosecond lasers, facilitating their enhanced drainage by lymphatics and phagocytosis by macrophages. In addition to QS- and picosecond lasers, fractionated nonablative devices such as the 1927-nm low power diode laser, the 1927-nm thulium fiber laser, and again, the 1550-nm erbium-doped laser can also be effective at addressing hyperpigmentation. The latter, when administered for 3 sessions over 4-8 week intervals (15 mJ, treatment level 6) has been shown to almost completely eliminate PIH by 7 months after the final treatment.8
Hypopigmented scars
Hypopigmented scars can be a challenge to repigment, though both ablative and nonablative fractionated lasers have been shown to accomplish this with varying degrees of success. Theories as to how these devices are able to improve the appearance of hypopigmented scars include facilitating melanocyte repopulation and/or creating the illusion of color when the texture of the scar is both improved and blended with the surrounding skin. The 1550-nm erbium-doped laser (7-20 mJ, treatment level 7, density 1000-2500 MTZ/cm2, 4 treatments spaced 4 weeks apart) has yielded up to 50-75% improvement in hypopigmentation, with results lasting around 20 months.9,10 Adding topical bimatoprost and tretinoin or pimecrolimus contributed to this improvement.10
So what are your go-to lasers and settings for acne scars, for surgical scars, and other traumatic scars? What are your strategies for minimizing complications and optimizing outcomes in skin of color patients? What other types of treatment modalities do you like for scarring? Please share your comments at the end of this post, and on Instagram @nextstepsinderm!
Dr. Paul Friedman is the director of Dermatology and Laser Surgery Center in Houston, TX.
This information was presented by Dr. Paul Friedman at the 2019 Skin of Color Update held September 7-8 in New York City. The above highlights from his lecture were written and compiled by Dr Kimberly Huerth, Chief dermatology resident at Howard University in Washington DC.
Did you enjoy this post? Find more Skin of Color topics here.
References
- Zhu R, Yue B, Yang Q, et al. The effect of 595 nm pulsed dye laser on connective tissue growth factor (CTGF) expression in cultured keloid fibroblasts. Lasers Surg Med. 2015;47(2):203-209.
- Kuo Y, Wu W, Jeng S, et al. Activation of ERK and p38 kinase mediated keloid fibroblast apoptosis after flashlamp pulsed‐dye laser treatment. Lasers Surg Med. 2005;36(1):31-37.
- Kuo Y, Wu W, Jeng S, et al. Suppressed TGF-beta1 expression is correlated with up-regulation of matrix metalloproteinase-13 in keloid regression after flashlamp pulsed-dye laser treatment. Lasers Surg Med. 2005;36(1):38.
- Kuo Y, Jeng S, Wang F, et al. Flashlamp pulsed dye laser (PDL) suppression of keloid proliferation through down‐regulation of TGF‐β 1 expression and extracellular matrix expression. Lasers Surg Med. 2004;34(2):104-108.
- Darougheh A, Asilian A, Shariati F. Intralesional triamcinolone alone or in combination with 5‐fluorouracil for the treatment of keloid and hypertrophic scars. Clin Exp Dermatol. 2009;34(2):219-223.
- Alster TS, Tanzi EL, Lazarus M. The use of fractional laser photothermolysis for the treatment of atrophic scars. Dermatol Surg. 2007;33(3):295-299.
- Chrastil B, Glaich AS, Goldberg LH, Friedman PM. Second‐Generation 1,550‐nm fractional photothermolysis for the treatment of acne scars. Dermatol Surg. 2008;34(10):1327-1332.
- Katz TM, Goldberg LH, Firoz BF, Friedman PM. Fractional photothermolysis for the treatment of postinflammatory hyperpigmentation. Dermatol Surg. 2009;35(11):1844-1848.
- Glaich AS, Rahman Z, Goldberg LH, Friedman PM. Fractional resurfacing for the treatment of hypopigmented scars: A pilot study. Dermatol Surg. 2007;33(3):289-294.
- Massaki, Ane Beatriz Mautari Niwa, Fabi SG, Fitzpatrick R. Repigmentation of hypopigmented scars using an Erbium‐Doped 1,550‐nm fractionated laser and topical bimatoprost. Dermatol Surg. 2012;38(7):995-1001.
Image Credit:
Main image courtesy of the Journal of Drugs in Dermatology https://jddonline.com/articles/dermatology/S1545961618P1169X/3/