Collagen vascular diseases encompass a group of autoimmune disorders that can have a profound impact on an individual’s health and quality of life. At the 2023 Skin of Color Update, Dr. Ted Rosen, Professor and Vice-Chair of Dermatology at Baylor College of Medicine, explained how these conditions uniquely impact individuals with skin of color.
Missed the lecture?? Explore key insights and pearls right here!
Understanding Collagen Vascular Diseases and Their Impact
Collagen vascular diseases are a diverse group of autoimmune conditions that can affect multiple organ systems in the body. Conditions such as systemic lupus erythematosus, dermatomyositis, and scleroderma are hallmarked by the immune system’s attack on its own tissues, resulting in a spectrum of symptoms and complications.
Lupus
Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE), commonly referred to as lupus, is a complex autoimmune disease that can manifest in a variety of ways. It is important to note that lupus disproportionately affects African American individuals, with approximately one in 500 black women at risk. This highlights the substantial impact of the disease within this community.
SLE can be life-changing, and its manifestations vary widely. While we won’t delve into the rarest forms of the disease, it’s crucial to understand some of the common criteria used for diagnosing lupus (Figure 1).
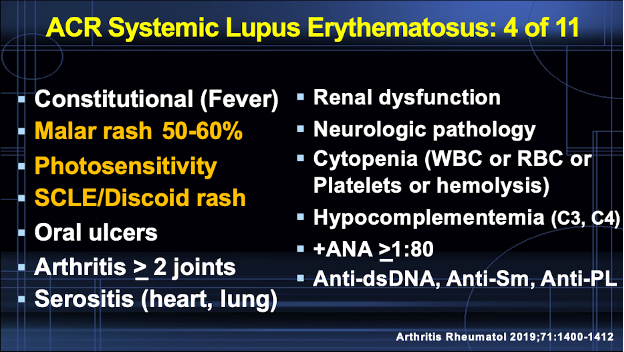
SLE often presents with symptoms like a distinctive skin rash, photosensitivity (an increased sensitivity to sunlight), and characteristic skin changes. In individuals with darker skin tones, the rash may appear more brown than red. Importantly, the associated facial rash spares the nasal labial folds (this is an important distinction from dermatomyositis). Skin color alterations can be subtle, making early diagnosis challenging.
Discoid Lupus
In discoid lupus affecting patients with skin of color, the rash tends to affect the face, scalp and ear. The rash is characterized by a hyperpigmented border surrounding a region of central hypopigmentation that may or may not demonstrate follicular plugging. Dr. Rosen notes that follicular plugging is less common in skin of color. Ear involvement is very common, so it is important to always check the ears!
The disease can lead to scarring and disfigurement, particularly in individuals with skin of color. These scarring lesions can be severe and have a considerable impact on patients’ well-being. It’s essential to recognize that lupus, due to chronic inflammation and vascular issues, can also increase the risk of squamous cell carcinoma. Early intervention is crucial in preventing such complications.
Treatment for lupus includes various options, such as corticosteroids, immunosuppressive agents, and monoclonal antibodies, among others. Dr. Rosen considers mycophenolate motefil as an adjunctive treatment, and it is slow to take effect. Emerging therapies, like Janus kinase (Jak) inhibitors and monoclonal antibodies such as Anifrolumab (Anti-IFN receptor), show promise in treating the disease. He emphasizes the importance of inclusive representation of ethnicities in clinical trials giving the example of Belimumab, a fully humanized monoclonal antibody that activates B-cells. This drug failed to show significant response in Black patients.
Dermatomyositis
Dermatomyositis is another collagen vascular disease that can affect individuals with skin of color. In dermatomyositis, muscle weakness is a primary symptom. Patients may struggle with everyday tasks like rising from a chair, climbing stairs, or even shampooing their hair.
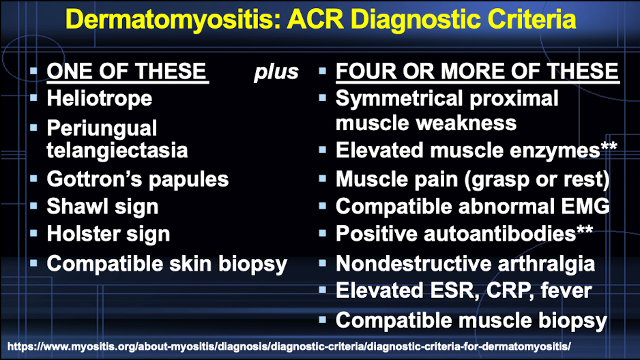
Skin manifestations are also common in dermatomyositis, but these can be subtle, particularly in individuals with darker skin. Typical skin findings include Gottron’s papules, heliotrope rash, and the shawl sign. However, these signs may present differently in people with skin of color, appearing more brown or grayish instead of violet or red. The heliotrope rash in skin of color may manifest as periorbital edema only. In contrast to lupus, the facial rash does NOT spare the nasolabial folds. The ACR diagnostic criteria requires a skin manifestation (or suggestive skin biopsy) as one of the diagnostic criteria (Figure 2).
Autoantibodies play a crucial role in the diagnosis and management of dermatomyositis. Anti-TIF1-gamma and anti-NXP-2 antibodies are associated with an increased risk of malignancy, making them essential markers in the evaluation of patients. In addition, male sex, age greater than 45 years, and skin of color increase risk of malignancy, which tends to manifest within the first year after diagnosis of dermatomyositis.
Scleroderma
Scleroderma, a rare collagen vascular disease, is characterized by the hardening and tightening of the skin and connective tissues (Figure 3). The disease can be particularly challenging for individuals with skin of color. In localized scleroderma, known as morphea, skin lesions may appear as large, hardened areas with hyperpigmentation.
Linear morphea can result in the loss of pigmentation and thickening of the skin.
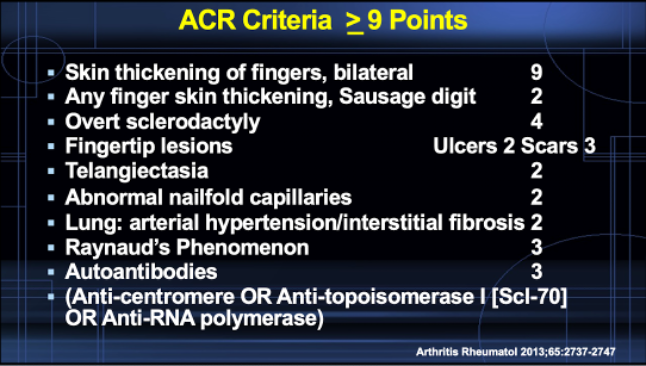
In progressive systemic scleroderma, skin involvement may manifest as confetti-like depigmentation. This condition can also lead to a range of internal organ complications, including heart, lung, and renal involvement. African American individuals appear to experience more severe forms of systemic scleroderma with a higher death rate.
Therapeutic options for scleroderma include steroids, immunosuppressive agents, and potential emerging monoclonal antibody therapies. Antimalarials have been found to be beneficial for morphea. Dr. Rosen notes that mycophenolate motefil is most helpful for scleroderma compared to the other connective tissue diseases.
In conclusion, collagen vascular diseases can affect individuals of all skin colors, but there are distinct variations in how these diseases manifest and impact people with skin of color. It is essential for healthcare providers to be aware of these nuances to ensure early diagnosis and appropriate management.
Advancements in treatments and emerging therapies offer hope for improved outcomes for individuals with collagen vascular diseases, regardless of their skin tone. With increased awareness and research, we can strive for more equitable care and better outcomes for all affected individuals.
This information was presented by Dr. Ted Rosen during the 2023 Skin of Color Update conference. The above highlights from his lecture were written and compiled by Dr. Sarah Millan.
Did you enjoy this article? You can find more on Medical Dermatology here.

