Explaining Mohs micrographic surgery to patients can be a challenge for Mohs surgeons and their staff. Yet patients may have an incomplete understanding of the surgery if they look to Internet videos – rather than to their Mohs surgeon – for answers to their Mohs questions.
Most patient-oriented video resources do not comprehensively explain Mohs, according to the authors of a letter to the editor published in the February issue of the Journal of Drugs in Dermatology. The authors found that Internet videos about Mohs discussed all three components of the surgery only 19% of the time. The videos discussed post-operative wound care only 21% of the time.
What are some key tips for explaining Mohs to patients so that patients have a good understanding of the surgery? I interviewed a panel of two Mohs surgeons – Joel L. Cohen, MD, FAAD, FACMS, associate clinical professor of dermatology at the University of California, Irvine, and Hayley S. Goldbach, MD, assistant professor of dermatology at the Warren Alpert Medical School of Brown University, Providence, R.I.
Mohs surgery is complicated and very different from other forms of surgery. Do you find it challenging to help your skin cancer patients have a good understanding of Mohs?
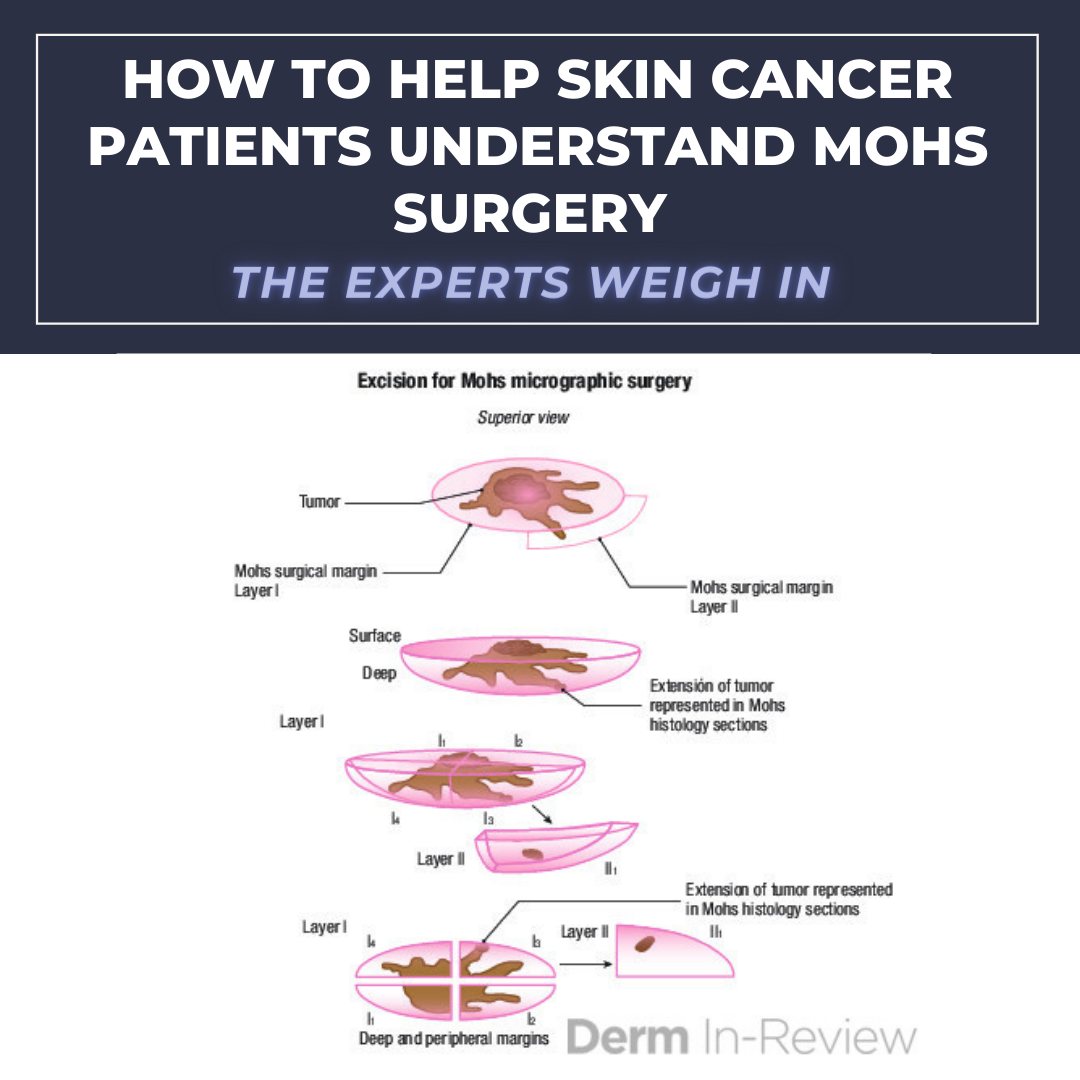
Dr. Cohen: I try to explain things very simply to patients. I draw a cartoon and explain that Mohs micrographic surgery allows us to see a more complete margin than traditional excision. It is much like looking at the crust of a pie or a chocolate candy wrapper. And I contrast this to bread loaf sizes of the tissue with an excision, where there’s a higher risk of missing an intervening tumor in between those slices simply because not all of the margin is being seen.
Dr. Goldbach: Every patient comes with disparate levels of health literacy and different levels of understanding Mohs surgery. I don’t find it challenging to ensure patients understand the procedure but it’s important to emphasize the rationale and expectations behind the surgery. Explanations can be tailored to a patient’s level of education and interest.
There are a lot of components to Mohs surgery. What are the key components that every Mohs patient should know, such as tumor excision, pathology and defect closure?
Dr. Goldbach: It’s key for patients to know that the benefit of Mohs surgery is full margin analysis. While I prepare the patient for surgery I usually discuss the concept of Mohs (I like using the often referenced peanut butter cup analogy) and what to expect from the surgical day. When it comes to defect closures, it’s important for patients to understand that the surgical closure is designed not only to minimize the size of scars but really to optimize the contour of a scar and restore integrity to the cosmetic subunits of a face. For my closures, especially flaps, I often draw schematics so that the patient is not surprised by the suture lines.
Dr. Cohen: I explain to patients very carefully that Mohs surgery is a tissue-sparing approach to removing these skin cancers. We are taking a very small margin and looking at a complete margin under the microscope while they wait (perimeter of the tissue plus the depth) in their room with a family member or friend.
I explain that we don’t know how large the skin cancer will be until we finish analyzing the tissue under the microscope, but that the defect should be smaller than it would be with traditional bread loaf slices of an excision because Mohs is looking at the full margin so a smaller rim of tissue around the tumor is taken. And Mohs surgery is associated with many studies showing a significantly higher cure rate than traditional excision. And I emphasize that once we reach that point of tumor clearance, we will then repair the surgical defect in most cases, but sometimes we let the site heal on its own by second intention. I show them the book of similar sized and located surgical defects from a few 3-ring binders that I have accumulated over many years to illustrate repairs and the healing process, and I even talk to them about laser treatment of scars if they are interested in some cases.
What are the key risks/benefits that Mohs surgeons should explain to every patient before surgery?
Dr. Goldbach: We always spend time with our patients going over the consent forms. I like to underline key portions and physically annotate the form with patient-specific risks — damage to the globe, temporal branch of the facial nerve, etc. But for every patient I always make sure to emphasize the risk of bleeding, infection, scarring and recurrence.
Dr. Cohen: As with any surgical procedure, there is a risk of bleeding, infection and prominent scarring. There is a risk of recurrence of the tumor, but with Mohs it is very, very low — about 1% for a primary BCC. Depending on the location of the tumor, I explain that there are certain anatomic structures that we are more concerned about. Around the eye, we are concerned about trauma to the eye itself or pulling on the eyelid after surgery. At the temple, we discuss the temporal nerve and how it is single-handedly responsible for elevation of the eyebrow on that side of the face. At the lateral chin area, I explain the risk of trauma to the marginal mandibular nerve. At the lateral neck posterior triangle, I explain the risk of trauma to the spinal accessory nerve.
What should every Mohs surgeon communicate to their patients about post-op wound care?
Dr. Cohen: Wound care is something that I emphasize a 3-pronged approach: explain, demonstrate and give a handout. It’s really important that patients with a sutured closure know that they should not create any tension vectors to the area of the stitches. This means no scrubbing or rubbing to clean the area of the stitches. This means not using sticky tape across the sutured wound edges, that can pull on the stitches and cause dehiscence. This means keeping the wound clean, moist with ointment, and covered with a non-stick bandage.
Dr. Goldbach: Post-op care discussions are the best investments you can make. You can avoid a significant amount of stress for both the surgeon and the patient if you spend the time to explain what to expect during the postoperative period. Your job as a surgeon doesn’t end when the last stitch is placed. I always discuss wound care in detail including why we recommend each aspect of wound care. In particular, many patients are under the erroneous impression that wounds should be exposed to air so we always take the time to discuss the use of postoperative emollients. We also discuss pain control, scar formation, swelling and signs of infection. Our team uses a “teach back” approach to wound care and also provides written instructions.
What tools do you use to educate your skin cancer patients about Mohs, such as personal conversations, handouts or videos?
Dr. Goldbach: Verbal discussions, handouts, and written diagrams currently form the cornerstone of our educational tools. Videos are not a current part of our practice but I can see incorporating that into our workflow in the future.
Dr. Cohen: While we demonstrate wound care to patients themselves, we encourage them to have one family member or friend with them for this part so that there is an extra set of eyes and ears during the explanation process of the wound care for the next few weeks.
If you provide handouts or videos, did you create these yourself or do you use materials from outside sources?
Dr. Goldbach: We have handouts that have been created from a hybrid of outside sources and updated with surgeon preference/edits.
Dr. Cohen: Over the years, we have made handouts regarding wound care and fine-tuned them along the way. These handouts vary from skin grafts to other types of sutured closures. We’ve also created specific instructions about wounds that are healing/granulating on their own by second intention.
What is your success with these communication tools?
Dr. Cohen: With the 3-pronged approach of explain, demonstrate and handout, patients usually do a pretty good job of getting it. But having a family member or friend there really helps as well. And sometimes that family member will ask if it’s okay to take some pictures or even a video of part of the wound care demonstration process. That can also be really helpful for certain closures when you want the bandage done or oriented a very specific way.
Dr. Goldbach: In my experience, verbal discussion with “teach back” is the most effective teaching tool and also has the added benefit of making patients feel cared for. Patients also tend to respond well to written instructions. Surgery can be a stressful experience and we know that patients don’t always retain all of what is discussed during an office visit or surgical procedure. My team tries to give the instructions to patients after the final layer but before the closure so that patients can read through the handout and have time to ask questions. As far as electronic resources, as of right now, most of my patients overall seem to prefer handouts and verbal communication.
How do you ensure that patients know what they need to know in order to make informed decisions, have reasonable expectations and properly care for their wound post-operatively?
Dr. Cohen: We call patients the day after surgery and review any questions or concerns. And we make sure patients know to call us if they have any questions or concerns that arise.
Dr. Goldbach: As far as informed consent, it’s important to assess a patient’s understanding of their diagnosis, options and risks. Depending on the patient I will also involve their family members and other physicians or members of their care team. Expectation management is also a huge part of preparing patients for surgery. When I work with residents I find that they often try to reassure patients (“you won’t even notice a scar,” “most people don’t have pain,” etc.) and I try to help them pivot to a caring model of realistic expectations. The more prepared a patient is for the surgical experience, the better able they are to manage any complications.
How have you changed the ways that you communicate about Mohs surgery with your patients over time?
Dr. Cohen: For some patients, my experience over the years often helps me identify folks that I think may have trouble with wound care and we offer to bring those people back in a few days to go over the process again. And they are free to bring a different family member if they would like (as sometimes an older patient might bring a spouse in the first place when they really should have brought their daughter or son).
Dr. Goldbach: After I attended journalism school, I became particularly interested in “patient facing” communication. What I have found is that you cannot have a one-size-fits-all approach to patient education. Don’t assume you know what the patient knows or doesn’t know or what their particular concerns are. I recall a recent pre-operative consultation where a younger patient came in very anxious. Before talking to the patient, I assumed it was fear of scarring or pain, but in fact the patient was most anxious about hair loss because they had recently regrown their hair after chemotherapy. We had a totally different conversation than I had expected.
Do you take special considerations in communicating with elderly patients? If so, how do you modify your patient education approach?
Dr. Goldbach: Absolutely. Of course elderly patients are not a monolith. However, I do have some general considerations. First and foremost, I like to know what sort of support system my elderly patients have at home because that can affect operative and post- operative decision making. We try to invite caretakers into the room during the wound dressing so that they can learn and ask questions as well. Mobility can be an issue with wound dressing so different strategies often need to be employed.
What other tips and tricks do you use in explaining and/or preparing patients after a skin cancer diagnosis?
Dr. Cohen: If it’s a BCC, I really try to calm their concerns. I explain that these are slow growing tumors that are not very aggressive and that we should just take care of it before it gets bigger and deeper, and becomes more of an issue.
Dr. Goldbach: This is another place where “teach back” communication can be the most successful. I try to communicate the diagnosis, the treatment options and what to expect if surgical treatment is selected. One thing I have found helpful is showing before and after photos of my prior patients so they have an idea of what to expect. As a younger female surgeon, I also find it is important to discuss my training credentials and experience.
What resources do you wish existed to help educate your Mohs patients?
Dr. Goldbach: I wish we had access to more open source patient handouts on niche topics. We have many, many of our own but it would be great to have access to more and on a PRN basis. For example, dilute vinegar soaks, Efudex wraps, bandaging ears, silicone scar sheets, etc.
Dr. Cohen: The American College of Mohs Surgery has some great content on their website explaining Mohs surgery and some of the different types of repairs. The AAD also has some very good patient resources, as does the Skin Cancer Foundation.
Did you enjoy this article? You can find more here.