Acne is a common skin condition that can be an important clue to an underlying endocrine disorder, such as polycystic ovarian syndrome (PCOS, Fig. 1). The first part of this 2-part series focused on the diagnosis and pathophysiology of PCOS-related acne. This article will focus on the diagnostic workup, including laboratory studies and imaging, and treatment options for patients with hormonal acne related to PCOS.

PCOS is a complex disorder characterized by elevated androgen levels, irregular menses and polycystic ovaries. Both hyperandrogenism and insulin resistance are central to the pathophysiology of PCOS, and this abnormal hormonal milieu may result in acne, hirsutism, androgenic alopecia and/or acanthosis nigricans. Since PCOS is a lifelong disorder associated with long-term cardiometabolic and reproductive implications, it is important for clinicians to be able to identify potential PCOS patients. As discussed in the previous article, if the clinical history and physical exam point toward a state of hyperandrogenism, laboratory studies and imaging may be helpful to confirm the diagnosis.
Biochemical evidence of hyperandrogenism can manifest as an elevated testosterone (free and/or total) or DHEA-sulfate level on laboratory studies (see Fig 2).
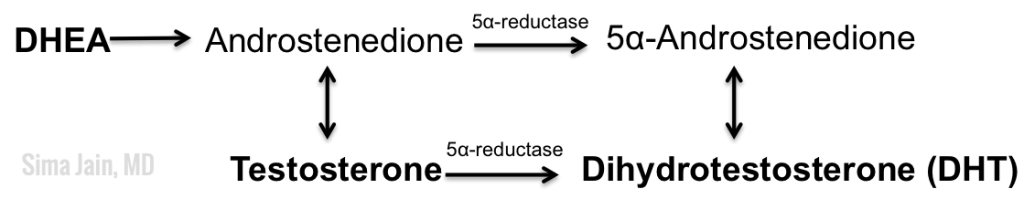
The table below outlines the important hormones to evaluate in PCOS.
Other labs to consider depending on clinical setting:
- Thyroid-stimulating hormone (TSH) level to rule out thyroid dysfunction
- Prolactin level to rule out hyperprolactinemia
- Cortisol level to rule out Cushing syndrome
- 17-hydroxyprogesterone level to rule out the most common form of congenital adrenal hyperplasia (CAH)
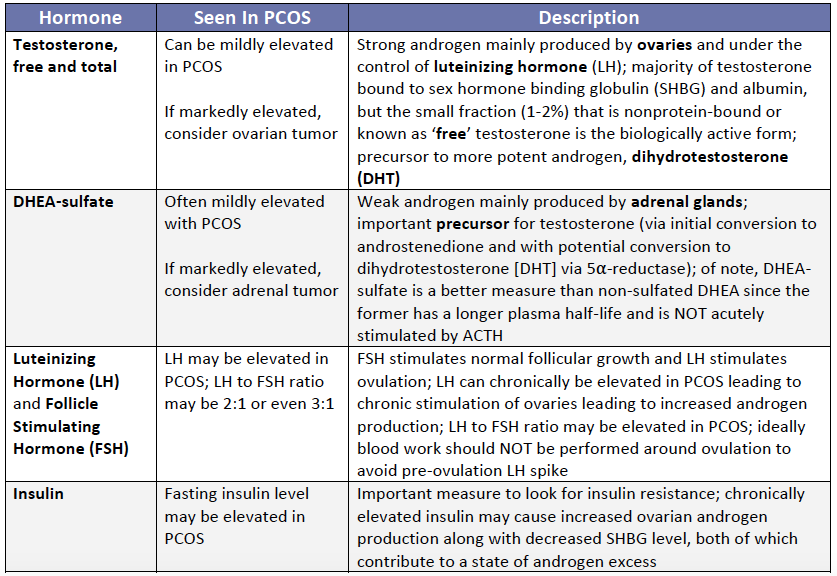
In addition to the above labs, imaging can also be quite helpful. Pelvic ultrasound may reveal polycystic ovaries, which is often seen in the setting of chronic anovulation. The ovaries may be 1.5 -3 times larger than normal and often have more than 12 follicles per ovary. Often, the cysts can be seen lined up along the periphery forming the appearance of a ‘pearl necklace’ or ‘string of pearls’ (see Fig 3). The follicles are small and immature, as they have never reached full development. Although the above findings are seen in many women with PCOS, they may also be noted sometimes in women without PCOS, so the clinical setting is important when interpreting these findings.
If the diagnosis of PCOS is strongly suspected or confirmed, certain treatment options should be considered specific to the pathophysiology. The different therapeutic options depend on many factors including patient age, childbearing status, and smoking status. The following is a brief synopsis of each medication. Please note that potential risks of each medication are not discussed here.
A combined oral contraceptive pill (COCP) is the mainstay chronic treatment for PCOS patients not seeking pregnancy. COCPs contain a synthetic estrogen (ethinyl estradiol) in combination with a progestin. There are different types of progestins that have varying levels of androgenic activity, but the COCPs often chosen for PCOS have progestins with a lower androgenic potential, such as norgestimate. COCPs work by decreasing ovarian androgen production as they decrease LH levels, increasing the level of SHBG (which reduces free testosterone) and regulating menstrual cycles. It also reduces the risk of endometrial cancer that is seen in PCOS patients with chronic anovulation.
Another important medication is spironolactone, which is a weak diuretic that is often used off-label for hormonal acne, hirsutism and androgenic alopecia. It inhibits the binding of both DHT and testosterone to androgen receptors. Due to its ability to inhibit androgens at different physiological levels, it has been widely used in women with androgenic alopecia, excess sebum, hirsutism and acne.
Metformin, a biguanide hypoglycemic drug, is another important medication to consider, especially in a setting of insulin resistance. Elevated plasma levels of insulin can increase production of ovarian androgens in PCOS. Metformin can ameloriate this as it decreases insulin levels, improves insulin sensitivity, decreases hepatic glucose output, and may correct ovarian and functional adrenal hyperandrogenism in PCOS, leading to clinical improvement in acne. Referral to endocrinology for patients with insulin resistance should also be considered for further evaluation and management.
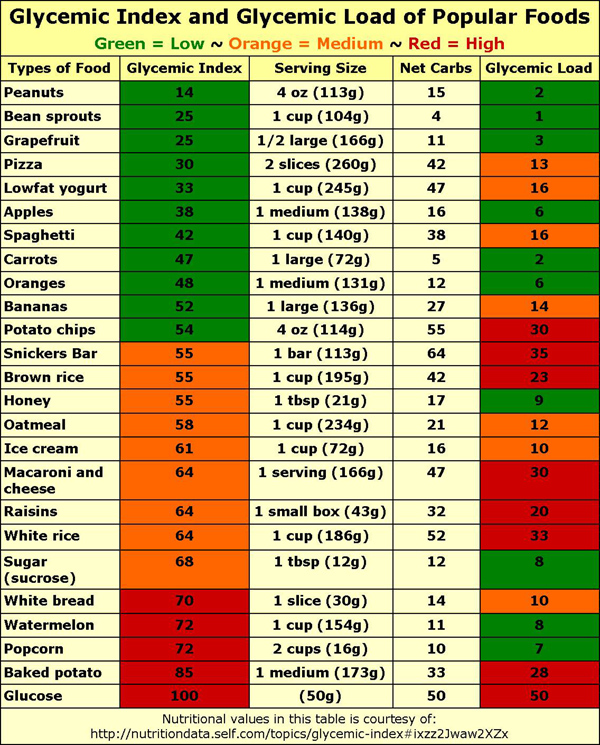
Diet counseling is imperative since there is no cure for PCOS, and the aim of treatment is to reduce symptoms and prevent further complications. A low glycemic index diet (see Fig 4) is integral to PCOS treatment as the goal is to reduce insulin levels and the effect on androgen levels. Exercise and maintenance of a healthy body weight are also important lifestyle changes to help decrease insulin resistance since weight reduction can result in a decrease in LH, insulin and testosterone.
Diet counseling, weight reduction, and the above described medications are all important facets in the treatment of PCOS and can have a significant impact not only in the patient’s self confidence but also can decrease the overall long-term morbidity of PCOS.
In conclusion, PCOS is a complex syndrome with long-term implications. Due to the dermatologic manifestations resulting from the abnormal hormonal milieu, dermatologists are often the first, and sometimes only, physician these patients see. Thus, it is important to be cognizant of the symptoms and signs for early diagnosis and avoidance of long-term complications.
Photo Credits:
Figures 1 & 2 Courtesy of Sima Jain, MD
Figure 3 Courtesy of Dr. J Ray Ballinger
Figure 4 Courtesy of http://nutritiondata.self.com/topics/glycemic-index#ixzz2Jwaw2XZx
If you missed part 1 of this 2-part series, you can find it here.
Did you enjoy this post? Find more on Medical Derm Topics here.