Pediatric dermatologic emergencies are very real, highlights Dr. Kalyani Marathe, Associate Professor of Dermatology and Pediatrics at the University of Cincinnati, who lectured during ODAC 2023. Pediatric dermatologic emergencies represent almost 4% of emergency room visits, and of those, most are related to chronic skin disease, drug eruptions, and infections. Here, we will review some of those common pediatric dermatologic emergencies, their challenges in diagnosis, and their best practices in management.
Drug Eruptions
Drug eruptions can have variable presentations in children. They can easily be confused for infectious exanthems, for which a thorough history must be obtained.
Drug reaction with eosinophilia and systemic symptoms (DRESS)
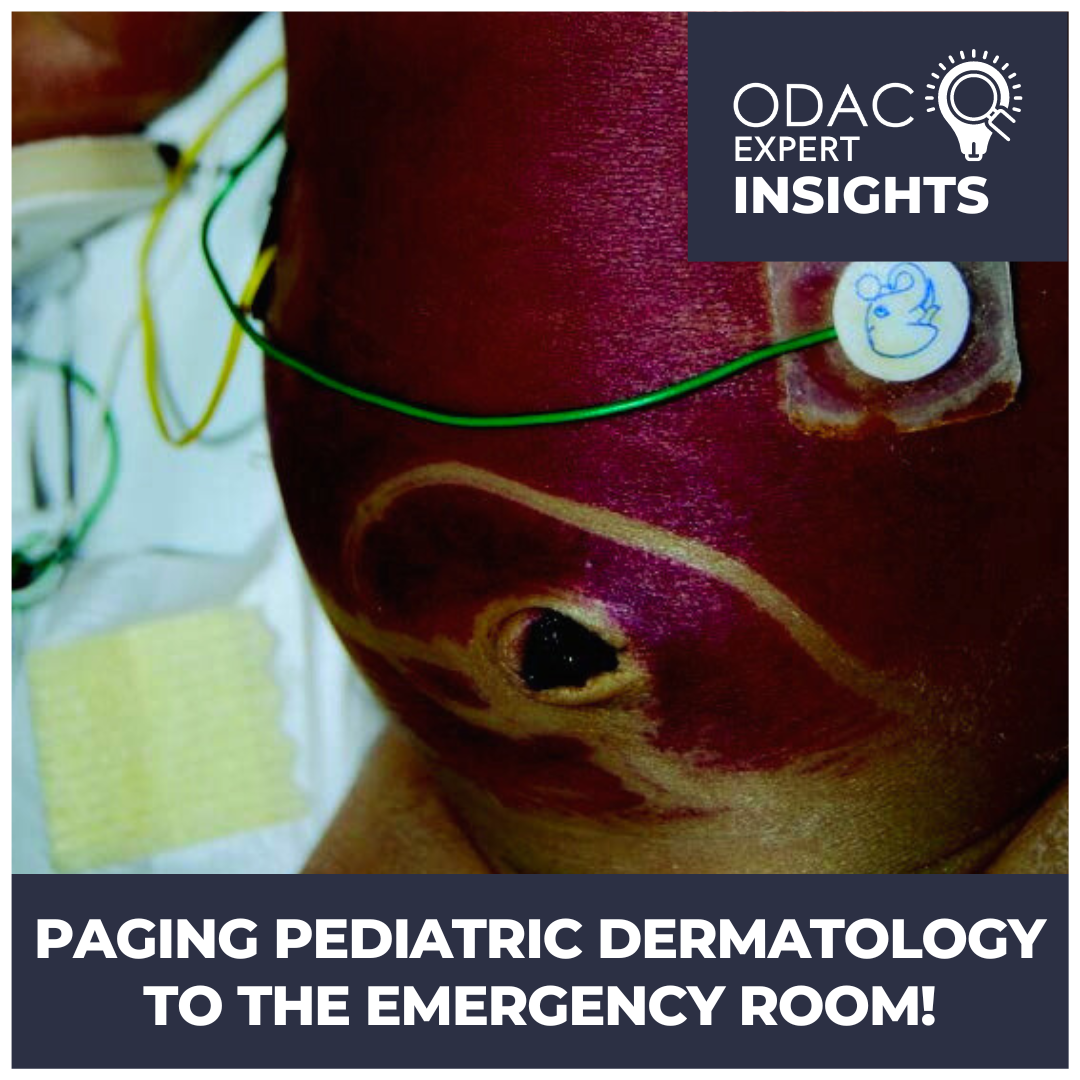
Consider this first case—a girl who presented to the emergency department three weeks after a course of trimethoprim-sulfamethoxazole (i.e., Bactrim) with dusky erythematous papules, as shown. Her labs also showed elevated liver enzymes, and she was diagnosed with DRESS.

Well, some may think this is the same disease as in adults, but there are some key differences:
-
- Facial involvement is common in pediatric DRESS but facial edema is less common than in adults.
- Common drug triggers (which may be less clear than in adults) usually involve antiepileptics or antibiotics (e.g., vancomycin, TMP-SMX). Medications like allopurinol are less likely in children.
- Lymphadenopathy and fever are more likely to be present in children than in adults.
For suspected DRESS, check labs during the acute eruption and after resolution. This should include:
-
- Complete blood count
- Liver function tests
- Creatinine
- Urinalysis
- Human herpesvirus-6
- Thyroid testing (at 3 and 6 months after)
Treatment can include steroids (1-2 mg/kg/day) with a long taper, cyclosporine 5mg/kg divided into twice-daily dosing for 2 weeks, or IVIG (after checking an IgA level).
Stevens-Johnson Syndrome/Toxic epidermal necrolysis (SJS/TEN)
The next case was of a 6-year-old boy who presented to the emergency department with several days of malaise, oral ulcerations, and burning in the eyes with blisters. It turns out he was started on carbamazepine for his seizure disorder two weeks prior, ultimately consistent with SJS/TEN due to an antiepileptic—a common trigger in children.

SJS/TEN is on a spectrum. Important clues like the positive Nikolsky sign, mucosal involvement (which precedes cutaneous involvement), and palmoplantar involvement can help make the diagnosis. The workup should include:
-
- Complete blood count
- Basic metabolic panel
- Liver function tests
- Erythrocyte sedimentation rate
- Urinalysis
- Consult ophthalmology
What’s shocking is that BSA>30% and systemic comorbidities (e.g., infection, renal failure, sepsis) increase mortality, which is about 4% for SJS/TEN and 16% for TEN.
For treatment, remember ABCDE, and you will know exactly what to do!
-
- A: Admit to burn unit or ICU
- B: Bathe gently with saline and cover with thick petrolatum
- C: Corticosteroids and cyclosporine can improve outcomes and reduce mortality
- D: Dress with non-adherent, silver dressings with mupirocin on eroded sites
- E: Eye lubrication and consider amniotic membrane transfer
Urticaria multiforme (UM)
Next, we learned about a young child with the shown eruption and history of recent ear infection treated with amoxicillin. Hopefully, you recognize the wheals and think of urticaria multiforme, a reaction to an antibiotic or virus. But these wheals are unique in UM since they:
-
- Have dusky centers (though are not truly targetoid)
- Can coalesce into larger plaques
- Are present for less than 24 hours

But once you can recognize them, you will know that the treatment involves marking the drug allergy and alternating sedating and non-sedating antihistamines.
Infectious eruptions
Erythema multiforme (EM)
Like UM, EM is associated with viral infections—usually herpes simplex virus (HSV). Unlike UM, however, EM usually involves the mucosa and has palmoplantar involvement. These fixed lesions characteristically have 3 zones of color:
-
- Central duskiness
- Rim of pallor
- Rim of erythema
The lesions will typically last 2 weeks and are best treated with topical steroids and oral acyclovir if HSV is suspected.
Bullous impetigo
The next case of a 4-year-old with 2 days of blisters and crusting on the upper and lower extremities, including the axilla, is shown. Recognize the collarette of scale and central crusting, which often involves the face, and may help make the diagnosis of bullous impetigo.

Bullous impetigo can be treated systemically, such as with cephalexin, but a generalized cousin—staphylococcal scalded skin syndrome—should also be considered on the differential diagnosis.
Staphylococcal scalded skin syndrome (SSSS)
In this disease, Staphylococcus aureus produces toxins that result in superficial exfoliation. Usually, this disease occurs in children under age 5 whose immature kidneys are unable to clear the toxins. Patients can present with fever, irritability, skin tenderness, diffuse macular erythema, degloving of fingers or hands, periorbital skin involvement, perioral radial fissuring, or fragile blisters. The involvement can be very diffuse requiring IV antibiotics. But the benefit of choosing the right antibiotic (like penicillinase-resistant penicillin) can make your sick child go from sad to happy in a 24-hour period.
Reactive infectious mucocutaneous/mucosal-predominant eruption (RIME)
Previously called Mycoplasma-induced rash and mucositis (MIRM), this disease affects males more than women with an average age of 12. Usually, the disease has significant oral, ocular, and urogenital involvement, which can be diagnosed by nasopharyngeal swab of Mycoplasma PCR. Although it looks similar to SJS (which can be caused by Mycoplasma in children), treatment is different—antibiotics, systemic steroids, and IVIG. Unfortunately, recurrence is up to 8% with 3% mortality. Dr. Marathe’s pro tip is to use cyclosporine 4-5mg/kg divided twice daily over 5 days.
Eczema herpeticum
After using a facial mometasone cream, the shown infant was brought to the emergency room. The punched-out ulcerations and vesicles on an erythematous base were consistent with eczema herpeticum, caused by HSV in areas of a compromised skin barrier.

The question posed by the emergency provider was, “Should the patient be admitted?” When faced with this question, ask yourself 3 questions:
-
- Is the eyelid margin (specifically, the lash line) involved?
- Is there diffuse involvement?
- Are there systemic symptoms like fevers and chills?
If any of the answers are yes, then the patient should be admitted and swabbed for HSV1 and HSV2 with PCR and bacterial culture if there is impetiginization present. Treatment should include acyclovir 60mg/kg/day divided every 8 hours, topical mupirocin to open lesions, and oral cephalexin if there is bacterial superinfection. Hold topical steroids until 24 hours of antibiotics are complete.
Tinea capitis
Another interesting case was of a 6-year-old child presenting with a 1-year history of a scaly scalp that came and went with ketoconazole shampoo and cream treatment. Notice the shown pictures with scaly alopecic patches with broken-off “black dot” hairs and occipital and posterior cervical lymphadenopathy as signs classic for tinea capitis.

Tinea capitis is the dermatophytosis of the scalp spread through direct contact with animals, humans, and fomites. Most of the cases in the United states are caused by Trichophyton tonsurans while the most common organism worldwide, Microsporum canis, is the inflammatory counterpart. Treat tinea with griseofulvin solution (20-25 mg/kg for 8 weeks or at least two weeks past symptom resolution) or terbinafine crushed (1/4 tab daily for <20 kg, ½ tab otherwise).
Once tinea becomes inflammatory, it can form a kerion, which has purulent discharge and is often confused with infection; however, treatment of a kerion should include anti-inflammatory measures like topical or systemic steroids.
Other Scary Stuff
Although we have looked at cool cases with important pediatric dermatologic emergencies, there are other scary diagnoses worth knowing. Keep your eyes peeled for other diagnoses with these tips:
-
- ‘Blueberry muffin’ babies should be evaluated as an emergency for TORCH infection or malignancy
- Cutaneous atrophy in a neonate should prompt consideration of neonatal lupus, for which an EKG should be performed to evaluate for heart block
- Newborns with blisters or erosions may raise suspicion for neonatal pemphigus.
And with that, hopefully you feel prepared next time you hear the pager, summoning you to the emergency room to evaluate a pediatric dermatologic condition.
This information was presented by Dr. Kalyani Marathe during the 2023 ODAC Dermatology, Aesthetic and Surgical Conference. The above highlights from her lecture were written and compiled by Dr. Nishad Sathe.
Did you enjoy this article? Find more on Pediatric Dermatology here.