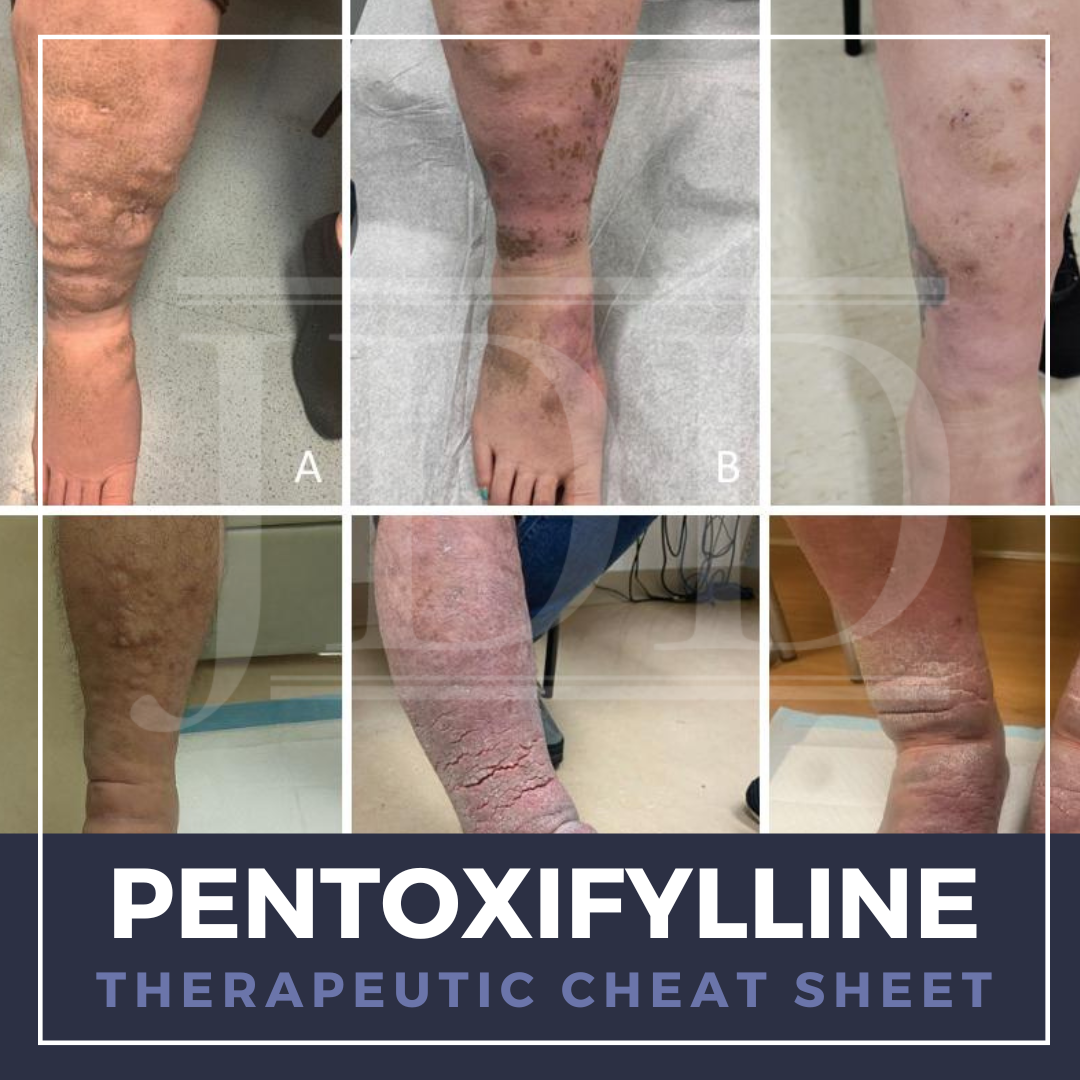
Pentoxifylline is a methyl-xanthine derivative traditionally used to treat symptoms of peripheral vascular disease and has emerged as a valuable therapeutic agent in dermatology for its anti-inflammatory and immunomodulatory properties. We continue our series, Therapeutic Cheat Sheet, with a closer look at pentoxifylline, which is FDA-approved for the treatment of intermittent claudication and is also used off label for dermatologic sequelae of peripheral vascular disease, vasculitis and vasculopathies, among others dermatoses.
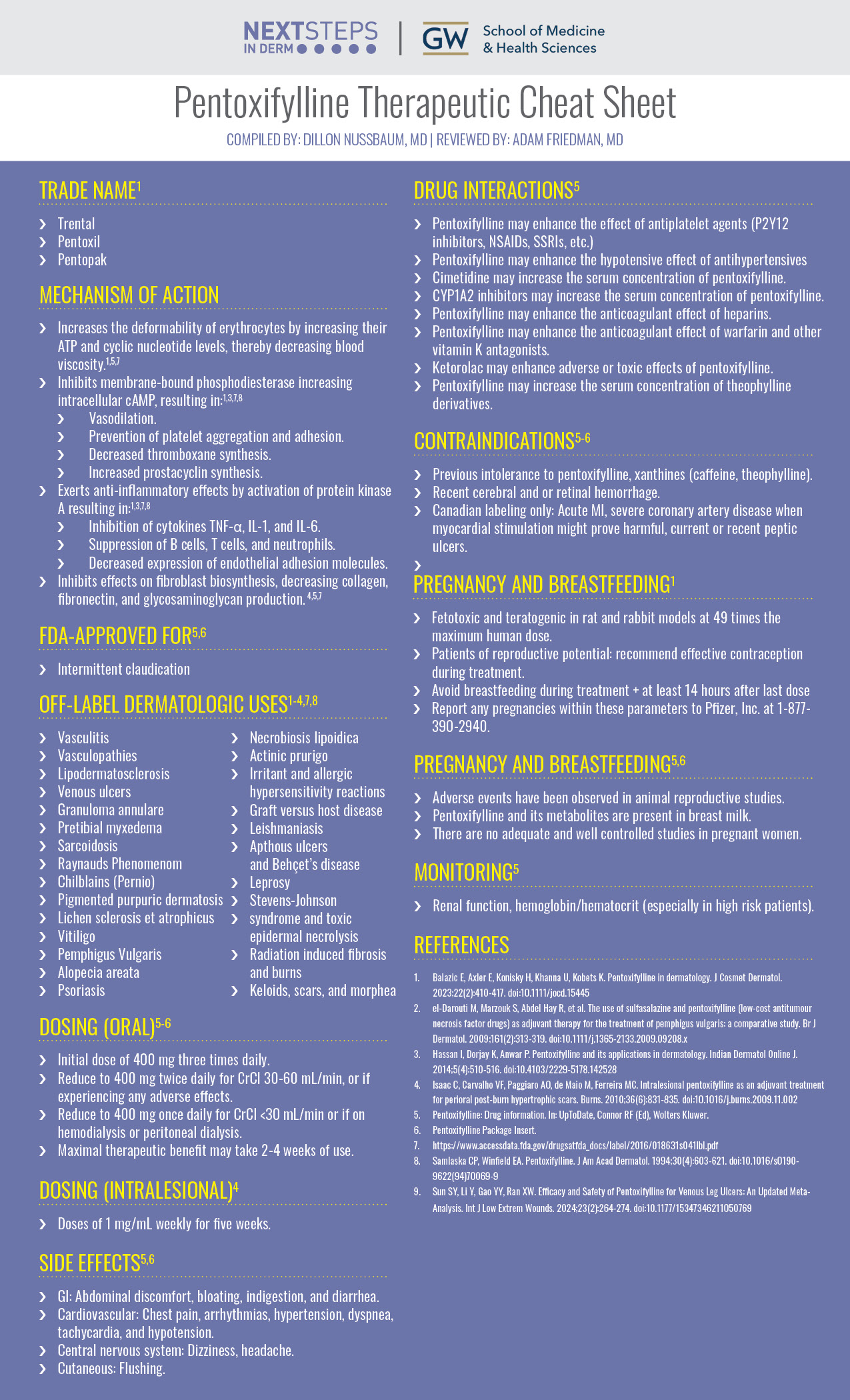
Pentoxifylline Therapeutic Cheat Sheet
Compiled by: Dillon Nussbaum, MD | Reviewed by: Adam Friedman, MD
TRADE NAME
-
- Trental
- Pentoxil
- Pentopak
MECHANISM OF ACTION
-
- Increases the deformability of erythrocytes by increasing their ATP and cyclic nucleotide levels, thereby decreasing blood viscosity.1,5,7
- Inhibits membrane-bound phosphodiesterase increasing intracellular cAMP, resulting in:1,3,7,8
- Vasodilation.
- Prevention of platelet aggregation and adhesion.
- Decreased thromboxane synthesis.
- Increased prostacyclin synthesis.
- Exerts anti-inflammatory effects by activation of protein kinase A resulting in:1,3,7,8
- Inhibition of cytokines TNF-α, IL-1, and IL-6.
- Suppression of B cells, T cells, and neutrophils.
- Decreased expression of endothelial adhesion molecules.
- Inhibits effects on fibroblast biosynthesis, decreasing collagen, fibronectin, and glycosaminoglycan production. 4,5,7
FDA APPROVED FOR5,6
-
- Intermittent claudication
OFF-LABEL DERMATOLOGIC USES1-4,7,8
-
- Vasculitis
- Vasculopathies
- Lipodermatosclerosis
- Venous ulcers
- Granuloma annulare
- Pretibial myxedema
- Sarcoidosis
- Raynauds Phenomenom
- Chilblains (Pernio)
- Pigmented purpuric dermatosis
- Lichen sclerosis et atrophicus
- Vitiligo
- Pemphigus Vulgaris
- Alopecia areata
- Psoriasis
- Necrobiosis lipoidica
- Actinic prurigo
- Irritant and allergic hypersensitivity reactions
- Graft versus host disease
- Leishmaniasis
- Apthous ulcers and Behçet’s disease
- Leprosy
- Stevens-Johnson syndrome and toxic epidermal necrolysis
- Radiation induced fibrosis and burns
- Keloids, scars, and morphea
DOSING (ORAL)5,6
-
- Initial dose of 400 mg three times daily.
- Reduce to 400 mg twice daily for CrCl 30-60 mL/min, or if experiencing any adverse effects.
- Reduce to 400 mg once daily for CrCl <30 mL/min or if on hemodialysis or peritoneal dialysis.
- Maximal therapeutic benefit may take 2-4 weeks of use.
DOSING (INTRALESIONAL)4
-
- Doses of 1 mg/mL weekly for five weeks.
SIDE EFFECTS5,6
-
- GI: Abdominal discomfort, bloating, indigestion, and diarrhea.
- Cardiovascular: Chest pain, arrhythmias, hypertension, dyspnea, tachycardia, and hypotension.
- Central nervous system: Dizziness, headache.
- Cutaneous: Flushing.
DRUG INTERACTIONS5
-
- Pentoxifylline may enhance the effect of antiplatelet agents (P2Y12 inhibitors, NSAIDs, SSRIs, etc.)
- Pentoxifylline may enhance the hypotensive effect of antihypertensives
- Cimetidine may increase the serum concentration of pentoxifylline.
- CYP1A2 inhibitors may increase the serum concentration of pentoxifylline.
- Pentoxifylline may enhance the anticoagulant effect of heparins.
- Pentoxifylline may enhance the anticoagulant effect of warfarin and other vitamin K antagonists.
- Ketorolac may enhance adverse or toxic effects of pentoxifylline.
- Pentoxifylline may increase the serum concentration of theophylline derivatives.
CONTRAINDICATIONS5,6
-
- Previous intolerance to pentoxifylline, xanthines (caffeine, theophylline).
- Recent cerebral and or retinal hemorrhage.
- Canadian labeling only: Acute MI, severe coronary artery disease when myocardial stimulation might prove harmful, current or recent peptic ulcers.
PREGNANCY AND BREASTFEEDING5,6
-
- Adverse events have been observed in animal reproductive studies.
- Pentoxifylline and its metabolites are present in breast milk.
- There are no adequate and well controlled studies in pregnant women.
MONITORING5
-
- Renal function, hemoglobin/hematocrit (especially in high risk patients).
FURTHER READING
If you would like to learn more about pentoxifylline, check out the following articles published in the Journal of Drugs in Dermatology:
Improvement of Pretibial Myxedema Following Administration of Teprotumumab, published in the Journal of Drugs in Dermatology
Washington, H. Nam, M. Pitch, B. Anderson, J. Stokes, and M. Helm
Abstract:
Pretibial myxedema (PTM) is a rare complication of Graves’ disease. It is characterized by non-pitting edema with hyperpigmented hyperkeratotic papules and plaques on bilateral lower legs. Effective treatments for patients with PTM are lacking. The etiology of PTM is unknown; however, it may be similar to the mechanism of thyroid-associated ophthalmopathy (TAO). Activated fibroblasts produce inflammatory cytokines and synthesize excessive glycosaminoglycans (GAG) that accumulate in the dermis and subcutaneous tissue. A recent, novel pathway implicates IGF-1 receptor as a mediator in this process. We present two patients with refractory PTM that improved following treatment with teprotumumab, an IGF-1 receptor inhibitor approved for use in TAO.
J Drugs Dermatol. 2022;21(11):1252-1254.
Intralesional Mode of Drug Administration in Psoriasis, published in the Journal of Drugs in Dermatology
Sathyan, K. Agarwal, I. Podder, A. Patil, L. Kircik, J. Weinberg, P. Yamauchi, S. Grabbe, and M. Goldust
Abstract:
The use of various conventional systemic and topical therapies in psoriasis has resulted in various major and minor side effects. Hence, we need to switch to intralesional administration of antipsoriatic drugs, to achieve better safety and efficacy profile. Intralesional drug therapy is most suitable for scalp, nail, and localized and recalcitrant plaque psoriasis. However, there are specific drugs, which can be used for this purpose, under strict monitoring. We have attempted to review all the possible drugs and indications where intralesional administration is feasible, along with their efficacy, adverse effects, dosage, and recommended duration of treatment.
J Drugs Dermatol. 2022;21(2):186-190.
References
-
- Balazic E, Axler E, Konisky H, Khanna U, Kobets K. Pentoxifylline in dermatology. J Cosmet Dermatol. 2023;22(2):410-417. doi:10.1111/jocd.15445
- el-Darouti M, Marzouk S, Abdel Hay R, et al. The use of sulfasalazine and pentoxifylline (low-cost antitumour necrosis factor drugs) as adjuvant therapy for the treatment of pemphigus vulgaris: a comparative study. Br J Dermatol. 2009;161(2):313-319. doi:10.1111/j.1365-2133.2009.09208.x
- Hassan I, Dorjay K, Anwar P. Pentoxifylline and its applications in dermatology. Indian Dermatol Online J. 2014;5(4):510-516. doi:10.4103/2229-5178.142528
- Isaac C, Carvalho VF, Paggiaro AO, de Maio M, Ferreira MC. Intralesional pentoxifylline as an adjuvant treatment for perioral post-burn hypertrophic scars. Burns. 2010;36(6):831-835. doi:10.1016/j.burns.2009.11.002
- Pentoxifylline: Drug information. In: UpToDate, Connor RF (Ed), Wolters Kluwer.
- Pentoxifylline Package Insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/018631s041lbl.pdf
- Samlaska CP, Winfield EA. Pentoxifylline. J Am Acad Dermatol. 1994;30(4):603-621. doi:10.1016/s0190-9622(94)70069-9
- Sun SY, Li Y, Gao YY, Ran XW. Efficacy and Safety of Pentoxifylline for Venous Leg Ulcers: An Updated Meta-Analysis. Int J Low Extrem Wounds. 2024;23(2):264-274. doi:10.1177/15347346211050769
Did you enjoy this Therapeutic Cheat Sheet? You can find more here.