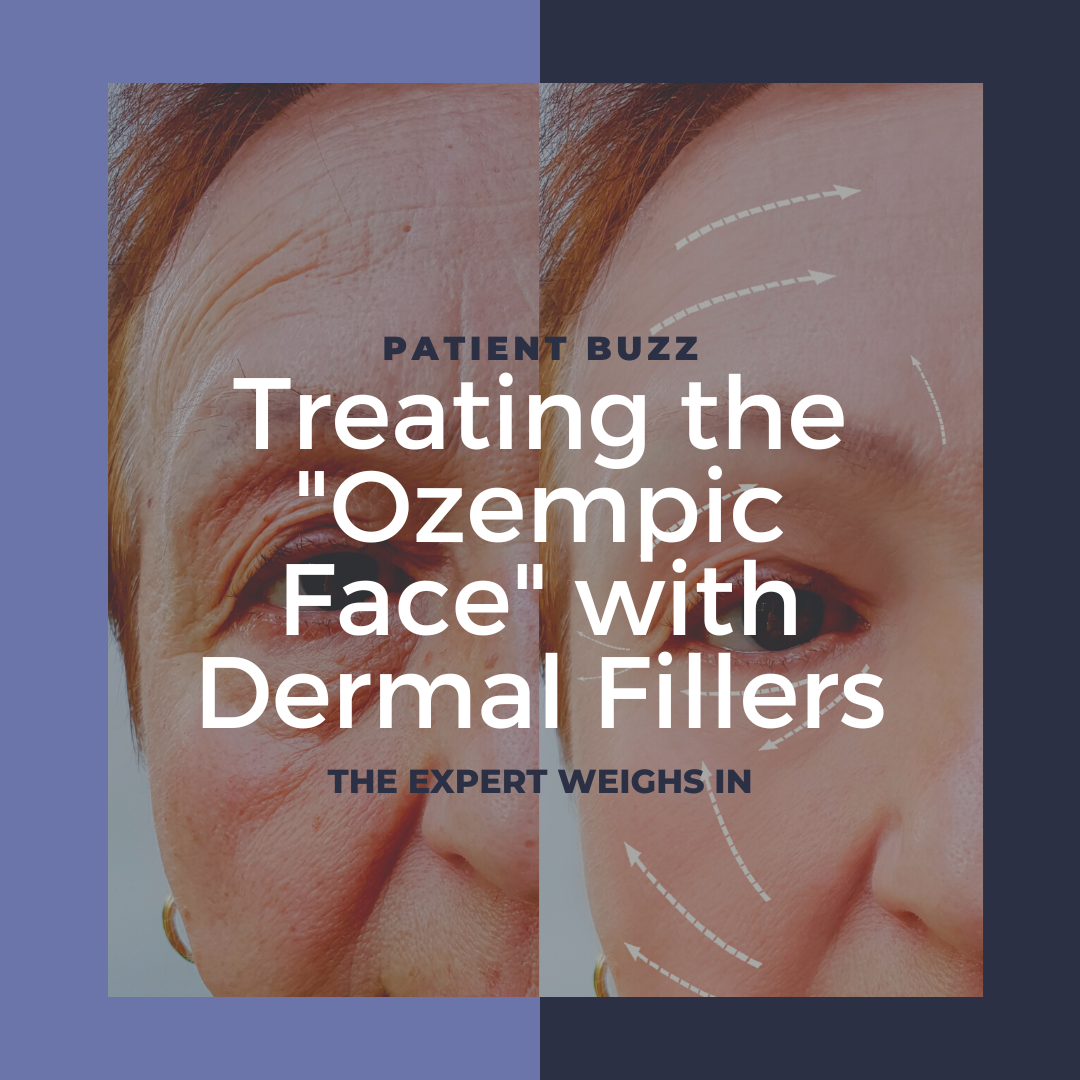
INSIDER recently posted an article on so-called “Ozempic Face” and the steps taken to treat a gaunt face after rapid weight loss. How common is “Ozempic Face,” and what’s the best way to treat it? What cautions should dermatologists keep in mind when treating patients who have experienced rapid weight loss?
For expert advice, I reached out to Robyn Siperstein, MD, FAAD, a dermatologist in Boca Raton and Boynton Beach, Florida.
Have you noticed “Ozempic Face” in your patients?
Yes, I have many patients with sudden weight loss, some from Ozempic and others from gastric bypass or even illness, whose faces look gaunt and drastically different, often out of proportion with their body. I actually saw this quite a bit in the last few years with those who were seriously ill with COVID as well, however with Ozempic, the weight loss is more extreme (50-60 pound weight loss instead of 20-30 pounds) and therefore the effect on the face is more obvious and distressing to patients.
How commonly do you treat cosmetic patients who recently experienced rapid weight loss?
I treat these patients every day in my office, and they need global volumization, otherwise they will look disproportionate if you only treat one feature. This can be done with many different products, but I favor hyaluronic acid fillers for their safety profile and immediate results.
Is there a difference in how weight loss appears on the face depending on the rapidity of weight loss?
Mostly, it is simply more noticeable to everyone when there is a sudden difference in someone’s face vs. a slow change over time. However, the faster weight loss gives the other tissues less time to adjust and therefore the skin is more likely to sag as it does not have the proper time to remodel around the new volume underneath. In addition, these patients are often over 40, which is a time when the skin and soft tissues are less likely to spring back to their shape before the weight gain since collagen and elastin are diminished.
What techniques do you use with your patients who have recently experienced rapid weight loss? What fillers have you found work best and in what manner?
I start with the temple as temple hollowing can be the biggest and most obvious sign of weight loss followed by the cheeks and jawlines. I inject a higher G prime filler deeper to replace the deep fat pads, and then a softer hyaluronic acid filler that spreads (less cohesive) more superficially to smooth out the contour changes. In most areas we are not trying to define the face but instead mimic the deep and superficial fat that has been reduced throughout. After the temple, I move downward to treat the sub-malar hollows and pre-auricular region. Then I move to the jawline and marionette area, which recedes. A filler with a stronger G prime and cohesivity is important on the jawline so it remains in place and anchors the face with a nice straight line from the chin to the gonial angle.
Should these techniques be used during the weight loss process or only when the weight loss is complete?
I would not recommend certain stimulatory fillers like Sculptra until people are done with their weight loss. If the body is losing weight, it is technically in what we call a starvation state, where there are not enough calories to keep up with the body’s energy needs. When the body is in this state, it is keeping its energy for the vital organs, such as the heart and brain, to function, and will not have any excess energy to create more collagen. It is important when being treated with stimulatory fillers to eat a lot of protein and make sure the calories coming in are more than necessary so that the body can expend the extra energy to make new collagen.
However, with hyaluronic acid fillers, this is not a problem and injections can be used at any time. It is important to warn patients that if they lose weight they often won’t see the improvement from the fillers since they could lose more fat than what was replaced with the filler. To prevent patients from getting disappointed with the results, it may make sense to wait, unless they want to maintain their look while slowly losing weight and understand they will continually need more.
Are there any cautions with injecting fillers into patients who have experienced rapid weight loss?
In patients without a thick fatty layer, it takes more skill, as there is less of a space to place the filler, since we do not want to inject filler into the muscle, which becomes the most prominent layer after the fat above and below recedes. In these cases, we need to recreate the space where the fat pads used to be located so knowledge of anatomy is essential. I use a cannula with a fanning technique to slowly spread the filler throughout the face to create a softer appearance. These patients are more at risk for the filler to show through the skin because they have less superficial fat to hide any filler lumps and bumps that can happen with filler boluses, which is why I do not use that technique in these patients. Additionally, I believe it is more likely to hit a blood vessel without a nice fatty layer to glide in, so I treat slowly and with less force mainly with a cannula.
If the patient regains the weight, what is the impact to the face if fillers were used during or after weight loss?
It is rare for someone to regain the weight faster than the clinical appearance of the filler recedes so this is not usually a problem. Often the patients look better when they regain the weight, and then refilling is no longer necessary.
What should every dermatology clinician know about treating patients with rapid weight loss?
I recommend physicians inject slowly in stages over time since these patients with massive weight loss often need numerous syringes, and the swelling from multiple syringes can obscure the end outcome and lead to an unnatural effect if done all at once. If the filler is done correctly and slowly, and utilizing the knowledge of the location of the fat pads, the results can be very rewarding.
Did you enjoy this Patient Buzz expert commentary? You can find more here.