Upadacitinib (RINVOQ®) is a once daily oral medication that is FDA approved for a variety of conditions including psoriatic arthritis and atopic dermatitis. Jak inhibitors, like upadacitinib, are a class of drugs showing to be effective in treating inflammatory conditions. Upadacitnib is not only being used to treat rheumatoid arthritis and psoriatic arthritis, but was recently FDA approved in 2022 for the treatment of moderate to severe atopic dermatitis in patients 12 years old and older who did not respond well to previous treatment.1 In this Therapeutic Cheat Sheet, we will focus on upadacitinib and its use for several dermatologic conditions, including psoriatic arthritis and atopic dermatitis.
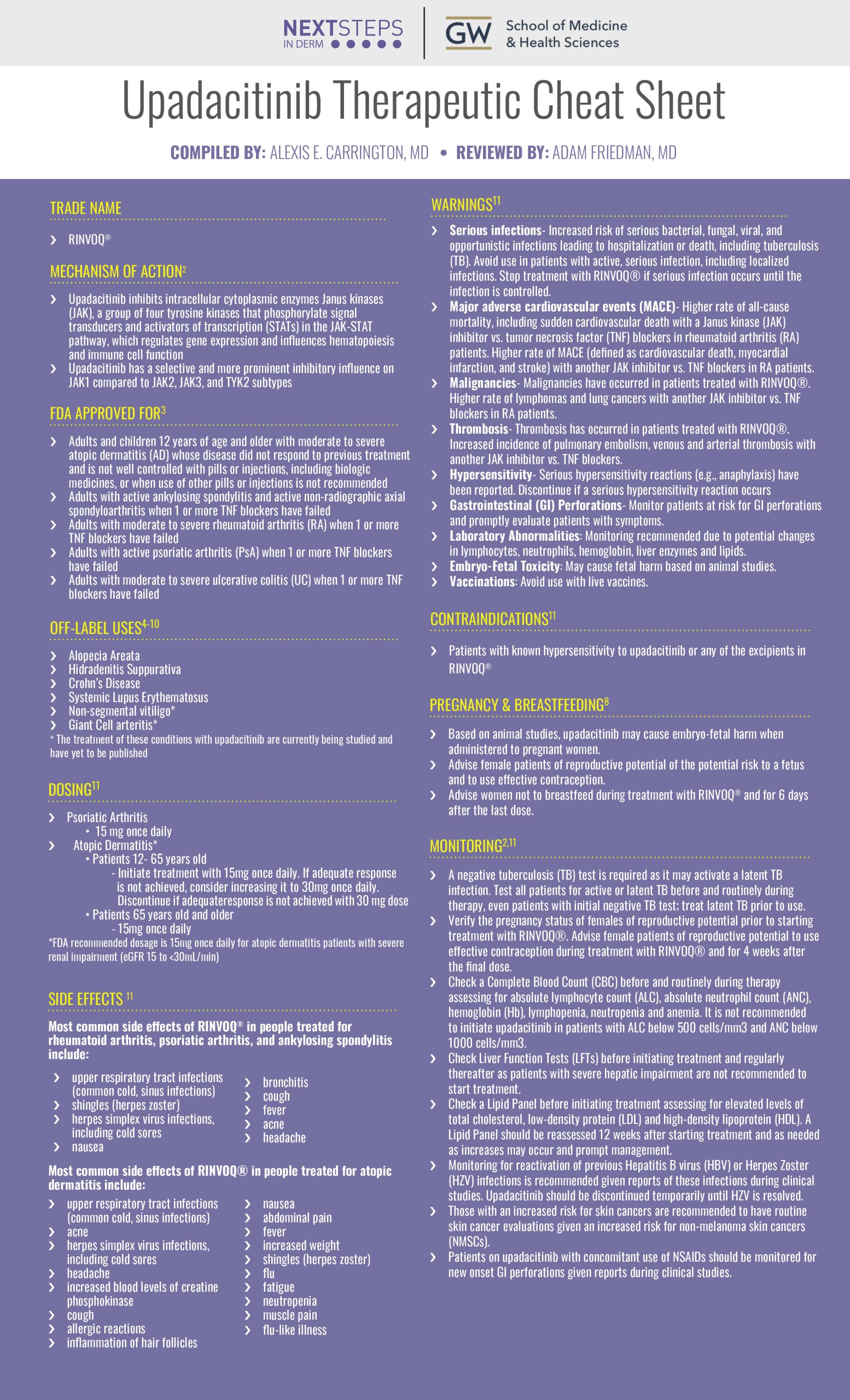
Upadacitinib Therapeutic Cheat Sheet
Compiled by: Alexis E. Carrington, MD, Reviewed by: Adam Friedman, MD
UPADACITINIB TRADE NAME
-
- RINVOQ®
MECHANISM OF ACTION2
-
- Upadacitinib inhibits intracellular cytoplasmic enzymes Janus kinases (JAK), a group of four tyrosine kinases that phosphorylate signal transducers and activators of transcription (STATs) in the JAK-STAT pathway, which regulates gene expression and influences hematopoiesis and immune cell function
- Upadacitinib has a selective and more prominent inhibitory influence on JAK1 compared to JAK2, JAK3, and TYK2 subtypes
FDA APPROVED FOR3
-
- Adults and children 12 years of age and older with moderate to severe atopic dermatitis (AD) whos disease did not respond to previous treatment and is not well controlled with pills or injections, including biologic medicines, or when use of other pills or injections is not recommended
- Adults with active ankylosing spondylitis and active non-radiographic axial spondyloarthritis when 1 or more TNF blockers have failed
- Adults with moderate to severe rheumatoid arthritis (RA) when 1 or more TNF blockers have failed
- Adults with active psoriatic arthritis (PsA) when 1 or more TNF blockers have failed
- Adults with moderate to severe ulcerative colitis (UC) when 1 or more TNF blockers have failed
OFF-LABEL USES OF UPADACITINIB 4-10
-
- Alopecia Areata
- Hidradenitis Suppurativa
- Crohn’s Disease
- Systemic Lupus Erythematosus
- Non-segmental vitiligo*
- Giant Cell arteritis*
* The treatment of these conditions with upadacitinib are currently being studied and have yet to be published
UPADACITINIB DOSING11
-
- Psoriatic Arthritis
- 15 mg once daily
- Atopic Dermatitis*
- Patients 12- 65 years old
- Initiate treatment with 15mg once daily. If adequate response is not achieved, consider increasing it to 30mg once daily. Discontinue if adequate response is not achieved with 30mg dose
- Patients 65 years old and older
- 15mg once daily
- Patients 12- 65 years old
- Psoriatic Arthritis
*FDA recommended dosage is 15mg once daily for atopic dermatitis patients with severe renal impairment (eGFR 15 to <30mL/min)
UPADACITINIB SIDE EFFECTS11
Most common side effects of RINVOQ® in people treated for rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis include:
-
- upper respiratory tract infections (common cold, sinus infections)
- shingles (herpes zoster)
- herpes simplex virus infections, including cold sores
- bronchitis
- nausea
- cough
- fever
- acne
- headache
Most common side effects of RINVOQ® in people treated for atopic dermatitis include:
-
- upper respiratory tract infections (common cold, sinus infections)
- acne
- herpes simplex virus infections, including cold sores
- headache
- increased blood levels of creatine phosphokinase
- cough
- allergic reactions
- inflammation of hair follicles
- nausea
- abdominal pain
- fever
- increased weight
- shingles (herpes zoster)
- flu
- fatigue
- neutropenia
- muscle pain
- flu-like illness
UPADACITINIB WARNINGS11
-
- Serious infections- Increased risk of serious bacterial, fungal, viral, and opportunistic infections leading to hospitalization or death, including tuberculosis (TB). Avoid use in patients with active, serious infection, including localized infections. Stop treatment with RINVOQ® if serious infection occurs until the infection is controlled.
- Major adverse cardiovascular events (MACE)- Higher rate of all-cause mortality, including sudden cardiovascular death with a Janus kinase (JAK) inhibitor vs. tumor necrosis factor (TNF) blockers in rheumatoid arthritis (RA) patients. Higher rate of MACE (defined as cardiovascular death, myocardial infarction, and stroke) with another JAK inhibitor vs. TNF blockers in RA patients.
- Malignancies– Malignancies have occurred in patients treated with RINVOQ®. Higher rate of lymphomas and lung cancers with another JAK inhibitor vs. TNF blockers in RA patients.
- Thrombosis– Thrombosis has occurred in patients treated with RINVOQ®. Increased incidence of pulmonary embolism, venous and arterial thrombosis with another JAK inhibitor vs. TNF blockers
- Hypersensitivity– Serious hypersensitivity reactions (e.g., anaphylaxis) have been reported. Discontinue if a serious hypersensitivity reaction occurs
- Gastrointestinal (GI) Perforations- Monitor patients at risk for GI perforations and promptly evaluate patients with symptoms
- Laboratory Abnormalities: Monitoring recommended due to potential changes in lymphocytes, neutrophils, hemoglobin, liver enzymes and lipids
- Embryo-Fetal Toxicity: May cause fetal harm based on animal studies.
- Vaccinations: Avoid use with live vaccines
- Hepatic Impairment: RINVOQ® is not recommended in patients with severe hepatic impairment.
CONTRAINDICATIONS11
-
- Patients with known hypersensitivity to upadacitinib or any of the excipients in RINVOQ®
PREGNANCY & BREASTFEEDING8
-
- Based on animal studies, upadacitinib may cause embryo-fetal harm when administered to pregnant women.
- Advise female patients of reproductive potential of the potential risk to a fetus and to use effective contraception
- Advise women not to breastfeed during treatment with RINVOQ® and for 6 days after the last dose
MONITORING2,11
-
- A negative tuberculosis (TB) test is required as it may activate a latent TB infection. Test all patients for active or latent TB before and routinely during therapy, even patients with initial negative TB test; treat latent TB prior to use.
- Verify the pregnancy status of females of reproductive potential prior to starting treatment with RINVOQ®. Advise female patients of reproductive potential to use effective contraception during treatment with RINVOQ® and for 4 weeks after the final dose.
- Check a Complete Blood Count (CBC) before and routinely during therapy assessing for absolute lymphocyte count (ALC), absolute neutrophil count (ANC), hemoglobin (Hb), lymphopenia, neutropenia and anemia. It is not recommended to initiate upadacitinib in patients with ALC below 500 cells/mm3 and ANC below 1000 cells/mm3.
- Check Liver Function Tests (LFTs) before initiating treatment and regularly thereafter as patients with severe hepatic impairment are not recommended to start treatment.
- Check a Lipid Panel before initiating treatment assessing for elevated levels of total cholesterol, low-density protein (LDL) and high-density lipoprotein (HDL). A Lipid Panel should be reassessed 12 weeks after starting treatment and as needed as increases may occur and prompt management.
- Monitoring for reactivation of previous Hepatitis B virus (HBV) or Herpes Zoster (HZV) infections is recommended given reports of these infections during clinical studies. Upadacitinib should be discontinued temporarily until HZV is resolved.
- Those with an increased risk for skin cancers are recommended to have routine skin cancer evaluations given an increased risk for non-melanoma skin cancers (NMSCs).
- Patients on upadacitinib with concomitant use of NSAIDs should be monitored for new onset GI perforations given reports during clinical studies
Upadacitinib is effective at treating inflammatory conditions and is being used by dermatologists more in recent years given its effectiveness towards psoriatic arthritis and atopic dermatitis. The list of inflammatory conditions that JAK inhibitors are effective against continues to grow. For that reason, practitioners should continue to follow newly published reports studies focusing on the off-label uses of this medication.
Further Reading
If you would like to learn more about upadacitinib, check out the following two articles recently published in the Journal of Drugs in Dermatology:
Jak Inhibitor Safety Compared to Traditional Systemic Immunosuppressive Therapies
Stefano Daniele, Christopher Bunick
Abstract:
Dermatologists treating atopic dermatitis are interested in the safety profile of the recently available JAK inhibitors, upadacitinib and abrocitinib, especially after they received boxed safety warnings. Long-term clinical trial data using these JAK inhibitors for the treatment of atopic dermatitis suggest that they are associated with very low incidence rates of malignancy, major adverse cardiac events, and thromboembolic events. However, a knowledge gap exists regarding the incidence of adverse events for JAK inhibitors compared to traditional systemic therapies used to treat poorly controlled atopic dermatitis as well as baseline rates in both atopic dermatitis and reference control populations. To address this gap, we analyzed data regarding adverse events of special interest for methotrexate, cyclosporine, and systemic corticosteroids and calculated the incidence of adverse events per 100 patient-years for these drugs. We also examined data regarding baseline incidence of adverse events in atopic dermatitis and control patients. We found that compared to upadacitinib and abrocitinib, traditional systemic therapies for atopic dermatitis demonstrated equal or higher incidence rates for malignancy (excluding non-melanoma skin cancer), non-melanoma skin cancer, major adverse cardiac events, and venous thromboembolism. Moreover, the use of upadacitinib and abrocitinib also exhibited either comparable or lower incidence of malignancy (excluding non-melanoma skin cancer), major adverse cardiac events, and venous thromboembolism, but higher rates of non-melanoma skin cancer, in comparison to baseline rates in atopic dermatitis or control patients. These findings indicate that JAK inhibitors should be positioned, at least based on safety, ahead of traditional systemic therapies for atopic dermatitis treatment.
J Drugs Dermatol. 2022 Dec 1;21(12):1298-1303.
Off-label uses of JAK Inhibitors in Dermatology
Dillon Nussbaum, Erika McCormick, Sapana Desai, Emily Murphy, Karl Saardi, Adam Friedman
Abstract:
The Janus kinase (JAK)-signal transducer and activator of transcription (STAT) pathway is a crucial component of immune function, and JAK inhibitors allow dermatologists to regulate this pathway in certain disease states. Once bound to ligands, JAKs phosphorylate cytokine receptors and STAT proteins, which translocate to the nucleus and activate transcription of immunologic proteins.1 Four JAK isoforms have been identified: JAK1, JAK2, JAK3, and tyrosine kinase 2 (TYK2). The different isoforms bind varyingly to cytokines including interleukin (IL)-2, IL-4, IL-7, IL-9, IL-15, and IL-21. While the first-generation JAK inhibitors — tofacitinib, ruxolitinib, and baricitinib — block multiple JAK isoforms, second generation JAK inhibitors, such as decernotinib, abrocitinib, and upadacitinib, target a particular JAK, reducing adverse effects.
J Drugs Dermatol. 2022 Oct; 21(10):1143.
References
-
- Lytvyn Y, Mufti A, Abduelmula A, Sachdeva M, Maliyar K, Georgakopoulos JR, Yeung J. Efficacy and Safety of Upadacitinib for Management of Moderate-to-Severe Atopic Dermatitis: An Evidence-Based Review. Pharmaceutics. 2022 Nov 14;14(11):2452. doi: 10.3390/pharmaceutics14112452. PMID: 36432643.
- Padda IS, Bhatt R, Parmar M. Upadacitinib. [Updated 2022 Jul 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK572088/
- “RINVOQ® (Upadacitinib) Treatment for RA, PsA, AD, AS, Nr-AxSpA and UC.” RINVOQ, https://www.rinvoq.com/. Accessed 1 Dec. 2022.
- Tanaka Y. State-of-the-art treatment of systemic lupus erythematosus. Int J Rheum Dis. 2020 Apr;23(4):465-471. doi: 10.1111/1756-185X.13817. Epub 2020 Mar 5. PMID: 32134201; PMCID: PMC7187183.
- Kozera E, Flora A, Frew JW. Real-world safety and clinical response of Janus kinase inhibitor upadacitinib in the treatment of hidradenitis suppurativa: A retrospective cohort study. J Am Acad Dermatol. 2022 Dec;87(6):1440-1442. doi: 10.1016/j.jaad.2022.07.047. Epub 2022 Aug 4. PMID: 35934210.
- Shalabi MMK, Garcia B, Coleman K, Siller A Jr, Miller AC, Tyring SK. Janus Kinase and Tyrosine Kinase Inhibitors in Dermatology: A Review of Their Utilization, Safety Profile and Future Applications. Skin Therapy Lett. 2022 Jan;27(1):4-9. PMID: 35081305.
- Nussbaum, D. McCormick, E. Desai, S. Murphy, E. Saardi, K. Friedman, A. Off-label uses of JAK Inhibitors in Dermatology. J Drugs Dermatol. 2022 Oct;21(10):1143-1146. doi:10.36849/JDD.2021.NVRN1022
- Bourkas AN, Sibbald C. Upadacitinib for the treatment of alopecia areata and severe atopic dermatitis in a paediatric patient: A case report. SAGE Open Med Case Rep. 2022 Nov 28;10:2050313X221138452. doi: 10.1177/2050313X221138452. PMID: 36467009; PMCID: PMC9709177.
- Gori N, Cappilli S, Di Stefani A, Tassone F, Chiricozzi A, Peris K. Assessment of alopecia areata universalis successfully treated with upadacitinib. Int J Dermatol. 2022 Jul 2. doi: 10.1111/ijd.16342. Epub ahead of print. PMID: 35780287.
- Home – ClinicalTrials.gov. “Search of: Upadacitinib – List Results – ClinicalTrials.Gov.” Accessed December 13, 2022. https://clinicaltrials.gov/ct2/results?cond=upadacitinib&term=&cntry=&state=&city=&dist=.
- RINVOQ® (upadacitinib) [Package Insert]. North Chicago, Ill.: AbbVie Inc. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/211675s003lbl.pdf
Did you enjoy this therapeutic cheat sheet? You can find more here.