Poised at the microphone, Dr. Sima Jain taught us how to use dermoscopy to diagnose difficult clinical cases during the 17th Annual ODAC Dermatology, Aesthetic and Surgical Conference in Orlando, Florida. Dermoscopy uses epiluminescent microscopy to help the provider get a more in-depth examination of the skin. It is extremely helpful for aiding the diagnosis of pigmented skin lesions. Some of the most difficult clinical cases to diagnose are alopecias, pigmented malignant neoplasms, SCCs, and amelanotic melanoma. Dr. Jain’s lecture provided pearls on how to use dermoscopy to accurately diagnose these conditions.
Dr. Jain began with a case of a 39-year-old female physician who presented with hair loss at the front of the scalp for 6 months. Her hair loss was asymptomatic, and she had no burning, itching or scaling of the scalp. During her lecture, Dr. Jain outlined the area of hair loss on the frontal scalp that showed a receding hairline and very fine facial papules to the forehead. She then pointed out that there was a decrease in the lateral 1/3 of the eyebrow hair density.

Dermoscopic exam showed there were white regular dots on the scalp that represented eccrine and follicular openings with perifollicular scaling.
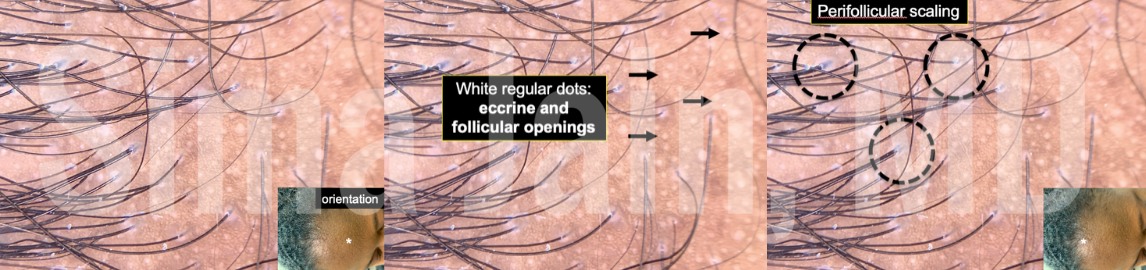
The finding of perifollicular scale is consistent with lichen planopilaris (LPP), which is a cicatricial (scarring) form of alopecia that is considered to be a follicular variant of lichen planus. It is hypothesized that lichen planopilaris is an autoimmune disorder in which T cells attack follicular antigens and cause loss of hair follicles. She detailed several important hallmarks for lichen planopilaris:
-
- Perifollicular scaling
- Progressive alopecia from destruction of the hair follicle
- Fibrotic white dots and areas
- Loss of number follicular ostia
Dermoscopy can help in identifying these features which leads to early diagnosis of the scarring alopecia. It also helps the provider to figure out where to biopsy the scalp for definitive diagnosis given that not all of the scalp follicles will be affected in a similar way. She summarized the case by bringing it back to the initial case where the patient had a variant of lichen planopilaris called frontal fibrosing alopecia. This variant can cause loss of hair in the eyebrows, fine facial papules on the forehead, and gradual recession of the frontal hairline.
Furthermore, Dr. Jain taught us that dermoscopy can be used to diagnose androgenetic alopecia. Androgenetic alopecia is a non-scarring hair loss that is one of the most common types of hair loss affecting both women and men. In women, there is gradual thinning of hair often at the part line followed by more diffuse hair loss over time. In men, there is often hair loss at the temples forming a receding hairline. There is also a thinning hair patch at the top of the head leading to progressive baldness. The peripilar sign on dermoscopy shows hyperpigmentation around the follicle which corresponds to perifollicular inflammation. The signs to look for on dermoscopy are:
-
- Peripilar sign
- Yellow dots
- Heterogeneity in hair shaft thickness
Next for the hair disorders, Dr. Jain instructed that there are 4 signs on dermoscopy to look for when diagnosing alopecia areata. Alopecia areata is a non-scarring alopecia that causes hair loss in round patches, often on the scalp. Similar to lichen planopilaris, it is an autoimmune disorder where T cells attack the hair follicles and cause hair loss. One of the most important signs to look for on dermoscopy is the presence of exclamation mark hairs. They look like tapered hairs and are a marker for disease activity. Other important signs to evaluate for are:
-
- White hairs
- Yellow dots
- Black dots
To round out difficult diagnoses for hair disorders, Dr. Jain discussed using dermoscopy to diagnose trichotillomania. Trichotillomania is a type of hair-pulling disorder where the patient has intermittent urges to pull his or her hair from hair-bearing areas of the body such as the eyebrows, eyelids, and scalp. Clinically patients may present with bald patches and have increased hair pulling episodes during times of stress. For the provider, it may be difficult to diagnose trichotillomania without a complete history of present illness. Dermoscopy can aid in diagnosis if the following signs are present:
-
- Broken hairs of variable length and shape
- V-shaped hairs
- Flame, coiled and/or tulip hairs that look like wavy or cone-shaped hair residue from severe mechanical pulling and shedding
- Yellow dots, broken hairs, black dots
Dr. Jain presented a second case of a 41-year-old male patient who presented with melanoma on his back. The features that helped her identify that it was a melanoma were discovered with dermoscopy. What she saw was a blue-white veil, shiny white lines, milky red and pink areas, and irregular blood vessels.
Dermoscopy can also pick up features of melanomas including the pseudopods, broadened network, regression, and reverse or negative pigment network. One of the most important features of melanoma, as mentioned above, is the shiny white structures (formerly known as crystalline structures) since these may be present in a featureless melanoma or amelanotic melanoma. These white structures indicate malignant tumor-induced stromal reaction and extracellular matrix change. They are associated with malignant growths like melanoma or BCC but can also be seen in benign growths like scar and dermatofibromas. The thick bright white lines are best observed with polarized dermoscopy.
A pearl to differentiate melanoma versus a pigmented BCC is that a pigmented BCC will not have a pigment network. However, melanoma as a pigmented lesion will have a pigment network. A BCC will also have telangiectasias, “spoke wheel” and “leaf-like” areas, blue-gray to brown dots, and blue ovoid nests.
The look of the vasculature in the lesion being evaluated with the dermatoscope can be helpful to determine if the lesion is benign or malignant. Dr. Jain showed an example of an SCC in situ that had glomerular vessels. This image was compared to an amelanotic melanoma that had polymorphic and dot vessels.
In summary, dermoscopy can be a very important tool to help the provider come up with a diagnosis for many challenging clinical cases. From alopecia to pigmented malignant lesions, the dermatoscope can provide features that would be otherwise missed on clinical exam and potentially lead to incorrect management. Knowing how to use dermoscopy can lead to early diagnosis and subsequent effective treatments.
This information was presented by Dr. Sima Jain at the 17th Annual ODAC Dermatology, Aesthetic and Surgical Conference held January 17–20, 2020 in Orlando, FL. The above highlights from her lecture were written and compiled by Dr. Nicole Negbenebor, PGY-2 dermatology resident at Brown University in Providence, Rhode Island, and one of the 7 residents selected to participate in the Sun Young Dermatology Leader Mentorship Program (a program supported by an educational grant from Sun Pharmaceutical Industries, Inc.).
Image Credits:
All clinical images are courtesy of Dr. Sima Jain.
Did you enjoy this article? Find more on Medical Dermatology here.